PRE2016 1 Groep1: Difference between revisions
mNo edit summary |
|||
| (399 intermediate revisions by 5 users not shown) | |||
| Line 1: | Line 1: | ||
[[File:titleHoist.jpg|600px]] | |||
== Group members == | == Group members == | ||
Marissa Damink 0858700 (M) | Marissa Damink 0858700 (M) | ||
| Line 6: | Line 7: | ||
Nicky Alexander 0886116 (N) | Nicky Alexander 0886116 (N) | ||
Jesse van Kempen 0907453 (JE) | [mailto:j.a.v.kempen@student.tue.nl?subject=USE:%20PassiveHoist Jesse van Kempen] 0907453 (JE) | ||
Jasmijn Kleij 0906848 (JA) | Jasmijn Kleij 0906848 (JA) | ||
== | == Abstract == | ||
The goal of this project was to improve the current passive patient hoist by making adjustments to enhance the convenience for primary users. In literature hardly any research was found about the use of passive patients hoists in hospitals and nursing homes. The first step of this research was to gain information from the users of the hoist by taking interviews and conducting a survey. Based on the results of the interviews and the survey seven requirements to improve the current passive hoist were made and implemented in the first design. Due to the feedback some alternations of the first design have been executed which resulted in the final design of the patient hoist. This final design consists of two different end products, one new patient hoist design that consists of all adjustments and one which is functioning as an add-on for the current patient hoist. | |||
== Introduction == | |||
- | Our current society is facing the societal dilemma of ageing, given that the ratio of care takers and caregivers is out of balance and will be expanded even more in the future. | ||
Technological advancements in health care are taking place, such as better treatment for diseases, and those also contribute to the increase of elderly people, because their lifespan is extended. | |||
Due to this, there will be a lack of caregivers in the future and therefore it will almost be inevitable that robots are partially taking over tasks. These tasks cannot be of great complexity of course, as robots are unable to think autonomous like humans. | |||
From this point of view, we have come up with a good use for robotics in which the relatively few human caregivers left in the future can focus on important and risky care tasks which should not be given in the hands of robots, like for instance the use of robots in operating theatres. | |||
Our idea will be realized by improving the current patient hoist in hospitals and nursing homes, in which patients who are not able to relocate themselves anymore, are transferred by lifting them. The patients can be transferred between for instance a bed and a chair or to places like restrooms and sitting rooms etc. | |||
However, unlike already existing patient lifts, our improved patient hoist (I.P.H.) can work partially autonomous and will be equipped with an interaction device. Due to this, the new patient hoist is able to detect emotions of patients. The USE-centered design method will play a significant role in our design cycle so the I.P.H. can be beneficial for all sorts of groups. | |||
=== Hypothesis === | |||
To guide the research several hypotheses have been set up. These are divided in main hypotheses with several sub-hypotheses. Some of these will be investigated through surveys and others will become clear from interviews. | |||
'''Caregivers need to be supported by the patient hoist''' | |||
- Caregivers need to be supported by cameras for navigating the patient hoist. | |||
- Caregivers need a patient hoist that can navigate itself and avoid obstacles. | |||
- The caregiver would like to be warned by the patient hoist whenever the patient is anxious. | |||
- Patients appreciate it when they are reassured by the patient hoist whenever they are anxious. | |||
- Caregivers need a patient hoist that can provide information about the weight or the 'BMI' of the patient. | |||
'''Patients and caregivers attach value to interaction during the process of lifting.''' | |||
- | - Patients need a certain level of interaction with the caregiver during the process of lifting. (So more need for touch/eye contact/speech, or no need?) (Survey) | ||
- | - During the interaction between patient and caregiver eye contact is more important than speech for a pleasant interaction. (Survey) | ||
- | - During the interaction between patient and caregiver eye contact is more important than physical contact for a pleasant interaction. (Survey) | ||
- Patients do not mind if the caregiver is absent for a certain part of the lifting process. | |||
=== Objectives and approach === | |||
- | The main objective of the project is to improve the current passive patient hoist. The passive instead of the active patient hoist is chosen, because a human-robot interaction adjustment can be of good use for this hoist. The interaction between patient and caregiver by using a passive hoist is not constant during the process as the distance between caregiver (behind the hoist) and patient (in the yoke of the hoist) is much larger than with an active hoist. | ||
To be able to determine the shortcomings and disadvantages of the current passive patient hoist it is important to get enough inside information. This information will be gathered by literature research, taking interviews and conducting a survey of the primary users of the hoist. After analysis of all this collected information the hypotheses stated above can either be confirmed or disconfirmed. The answers of the hypotheses are, next to the now known shortcomings and problems, used to set up requirements for the new design of the passive hoist. The new design will be sketched and a demonstration film will be made to illustrate/clarify the meanings of the made adjustments in the design. At the end feedback will be gathered to verify whether the adjustments in the new design are successful and a final design will be proposed by taking the feedback into account. | |||
== Scenarios == | |||
To give you all a proper view about the current use of the passive patient hoist, the current working method will be described in the next two scenarios: | |||
- | === '''Scenario 1''': - Inside one room - === | ||
“Transporting from bed to chair inside a room with the passive patient hoist” | |||
Mr. A is a 75 year old inhabitant of Parc Imstenrade, a home for the elderly. Mr. A, who cannot stand up by himself and therefore not able to relocate himself anymore, lies in his bed in room 23. Caregiver Lilly is going to put Mr. A in his chair near the window so he can see the nearby public garden. She will use the passive patient hoist to do so. | |||
2 | Lilly takes a lifting mat of the proper size for Mr. A and puts 2 whalebones in the backside of the lifting mat for better support for Mr. A’s back during the lifting process. She brings the bed to the right working height so she can work more easily without risking back problems. Lilly explains to Mr. A. what she is doing and is going to do at every step of the lifting process so he will not be surprised by any actions. First she turns Mr. A to his left side and pushes the lifting mat underneath him. Then she turns him to his right side so the mat can be equally divided underneath him. As soon as Mr. A lies back on his back again, Lilly lowers the bed, because the working height is too high for the patient hoist to lift Mr. A from his bed. Now the bed is at proper height and Mr. A lies correctly in the lifting mat, the patient hoist is called over. Lilly pushes the legs of the hoist beneath Mr. A.’s bed and guides the yoke of the hoist to the right position above Mr. A. By using the remote control of the hoist Lilly lowers the yoke so it can be attached to the lifting mat. The yoke is attached between Mr. A.’s legs and along both sides at shoulder height to the mat. The arms of Mr. A will stay inside the yoke and the mat during the lifting process. Once the mat is well attached to the yoke, Lilly lifts the yoke by using the remote control again. During the lifting Mr. A. is brought from a lying position to a sitting position in the mat. This is not very comfortable for Mr. A. because the lifting mat cuts a little bit between his legs. Once free from the bed, Lilly can move the patient hoist with Mr. A. towards his chair near the window. Note that this is not an easy task for her, because she has to push hard enough to get the hoist into motion, mind the environment of the hoist to prevent bumping up against things and hold one hand at the yoke so it will not shake too much, so Mr. A. will not get motion sick or scared due to the trembling. As they arrive at the chair, Lilly brings the hoist to the right position in front of the chair and moves the legs of the hoist from each other with the remote control so the hoist can be placed around the chair. She places the yoke with Mr. A .inside exactly above his chair so his back and the back of the chair are exactly in the same position. When chair and yoke are in the right position Lilly presses the remote control again to lower the yoke. Mr. A. is then gently lowered into his chair with the lifting mat underneath him. Once Mr. A. sits in his chair the yoke is released from the mat and the hoist is slowly driven away from the chair by Lilly while preventing a collision between the yoke and Mr. A. The whalebones in the backside of the lifting mat are removed, because they are not comfortable for Mr. A.’s back while sitting. Lilly asks Mr. A. whether he wants the lifting mat to stay underneath him or not. He does not want it underneath him, therefore Lilly pulls the mat from between his legs to the outside of his hips towards his back to remove it underneath him. Now Mr. A. can enjoy his sightseeing. | ||
=== '''Scenario 2''': - Transportation - === | |||
“Transporting from bed to general living room with the passive patient hoist” | |||
It is morning in ‘De Tulp’, a home for the elderly and the 70 year old Mrs. B. who suffers from paraplegia lies in bed. She is ready for nurse Jane to transport her to the general living room where she can sit next to her close friend Mrs. C. to gossip about the cute Mr. D of next door. Due to her illness Mrs. B. is not able to replace herself anymore so she will be transferred from her bed to the chair in de living room next to Mrs. C. by the passive patient hoist. Nurse Jane will use the same method as caregiver Lilly to bring Mrs. B. from her bed in the yoke as was done with Mr. A. in scenario 1. When this is done and Mrs. B. hangs above her bed in the yoke, Jane will drive the hoist out of Mrs. B.’s room over the corridor to the living room. Just like Lilly, Jane will explain what she is doing to Mrs. B. during the lifting and transfer process so Mrs. B. will be at ease and not surprised by any actions during her transfer. Jane will need to coordinate the whole process very carefully, because she needs to exert enough force to push the patient hoist. She has to take into account the surroundings of the hoist to prevent accidents during the transfer. She also frequently has to keep the yoke steady with one hand during the process so Mrs. A will not get motion sick or scared due to the trembling of the yoke. Before the transportation process of Mrs. B. with the hoist really can start Jane has to turn the yoke with Mrs. B. inside manually into the right direction. Due to this Mrs. B.’s face points forward, while the hoist and Jane are behind her. Mrs. B. is now able to see in what direction she is pushed by Jane. Jane can now start the transportation by pushing the hoist towards the room door. At the door Jane needs to be extra careful and make sure that she does not bump into something. This is necessary, because her sight about what is happening directly outside the door is not sufficient enough. She also needs to push the hoist with more power to drive over the little threshold. Once outside Mrs. B.’s room, Jane needs to focus again extra carefully to provide Mrs. B. a safe ride and to prevent any collisions with other humans or items in the hallway. Keep in mind that Jane and Mrs. B. cannot make any eye contact during the transportation process so Jane has to observe very attentively (as far as possible) whether something is going wrong with Mrs. B. The use of speaking is now the only solution for any interaction between them. Once arrived at the door of the living room, the threshold situation repeats itself and precise coordination of Jane is required. Jane puts Mrs. B. in the chair next to Mrs. C. by using the remote control to open the legs of the hoist and to lower the yoke just like was done to put Mr. A. in his chair in scenario 1. Mrs. B. en Mrs. C. can now finally continue their discussion about Mr. D. | |||
== Literature study == | |||
=== State-of-the-art === | |||
A patient hoist is a mechanical device for lifting a patient out of bed into a (wheel)chair. There are two kinds of hoists, the active and the passive one. The active hoist is meant for patients who still can stand up, but cannot move very well. It lifts the patient from a bed to a standing-up position on the hoist, after which the patient can be moved to a chair. The passive hoist is used for patients who are too weak to stay standing up. It moves the patient in a sitting position.<ref>http://www.domicare.nl/tilliften-badliften-verrijdbaar/</ref> | |||
Most passive hoists consist of a frame with a sling attached to it. The patient gets secured in the sling by the nurse and the hoist lifts the patient upwards. Next the hoist can be moved by the nurse towards the bed or chair and afterwards the hoist lowers the patient onto the bed or chair. Finally, the nurse releases the patient from the sling. There are lots of different models for passive hoists. Most hoists move the patient along a vertical axis, after which the whole device can be moved by the nurse. Some work with a rail which can transport the patient over a horizontal axis, after the patient has been lifted up. These rails can be integrated into the room, or can be moved from bed to bed. | |||
Most passive hoists consist of a frame with a sling attached to it. The patient | An active hoist does not move the patient from a lying position to a sitting position like the passive lift, but moves the patient from a sitting to a standing position. It can be used to transport the patient, but sometimes the active hoist is only used to help the patient to stand after which he/she can walk by him/herself, possibly with the help of a caregiver. This helps patients to maintain their mobility.<ref> http://www.arjohuntleigh.nl/producten/transfer-oplossingen/actieve-tilliften/</ref> | ||
An active hoist does not move the patient from a lying position to a | |||
A lot of research has been done about the use of patient hoists in hospitals and nursing homes. | A lot of research has been done about the use of patient hoists in hospitals and nursing homes. Johnsson et al. (2004)<ref name=Johnsson>Johnsson C., Kjellberg K. & Lagerstrom M. (2004) A direct observation instrument for assessment of nurses’ patient transfer technique (DINO). Applied Ergonomics35 (6), 591–601.</ref> proposed a model that simulated the balance between the nurse and the patient during a transfer task. The movement between the patient and the nurse should be harmonious, otherwise it may cause injuries. | ||
Research has proven that a lot of difficulties exist with the current patient hoists. Even when a hoist is available nurses do not always use it. Several reasons are: “(..) lack of time and availability, difficulty of use, space constraints, and patient preferences.” | Research has proven that a lot of difficulties exist with the current patient hoists. Even when a hoist is available nurses do not always use it. Several reasons are: “(..) lack of time and availability, difficulty of use, space constraints, and patient preferences.”.<ref name=six{{>http://ovidsp.tx.ovid.com.dianus.libr.tue.nl/sp-3.22.0a/ovidweb.cgi?QS2=434f4e1a73d37e8ce55b227ffaae5fa148541856cb5686bfad9f6431240b98c07524237e1720f34b02eb8fa2b88b7b97cae33df7331783914f69c8dde4ca12d06569431bde95318885c0300c9e4cb854a6adb57292dc4b9d5d515362ffaf06f20e36f3c9460a88b948e9e5dcf4c00bab436508a09afdce5366e7c719263f67d40a206676fd0c0a5686e4e1da71239e75c2ce0637418cb6107561917b1c775b62b2deac9baf23bbafabe516e9e595ddb3711a24619f5e9fff0b6524d61d8e55df726a6944468052b4402c3d9ae720be38f03cb8a56190a0535e3fa712b6c3423a74b470672b139464e79db6d185645a45cb60d8e15bd92bcee10aa989a2dfbadeef09927167e35fcee3135359c01e825083f314bc5221e7c8644d3bbcbe868deccbffbe8e7109265789c479c547d2e3fdb26a430178a76903ff214576e1d05cdf304d7473261f3c184d70eea1d98c1e23e9483a61fdd973d2af33538480ec1aee29fd33ec82224c9b14f035663bed6db11254245dfcda166d7bd10d7e687e549e4d066e920b3493fb}}</ref> By including the nurses in the buying process and buying a powered lift instead of a mechanical one, a nursing home can improve the chance of the hoist actually being used. Furthermore a hoist cannot decrease the risk coming with lifting, but it can still reduce it significantly.<ref name=six{{>http://ovidsp.tx.ovid.com.dianus.libr.tue.nl/sp-3.22.0a/ovidweb.cgi?QS2=434f4e1a73d37e8ce55b227ffaae5fa148541856cb5686bfad9f6431240b98c07524237e1720f34b02eb8fa2b88b7b97cae33df7331783914f69c8dde4ca12d06569431bde95318885c0300c9e4cb854a6adb57292dc4b9d5d515362ffaf06f20e36f3c9460a88b948e9e5dcf4c00bab436508a09afdce5366e7c719263f67d40a206676fd0c0a5686e4e1da71239e75c2ce0637418cb6107561917b1c775b62b2deac9baf23bbafabe516e9e595ddb3711a24619f5e9fff0b6524d61d8e55df726a6944468052b4402c3d9ae720be38f03cb8a56190a0535e3fa712b6c3423a74b470672b139464e79db6d185645a45cb60d8e15bd92bcee10aa989a2dfbadeef09927167e35fcee3135359c01e825083f314bc5221e7c8644d3bbcbe868deccbffbe8e7109265789c479c547d2e3fdb26a430178a76903ff214576e1d05cdf304d7473261f3c184d70eea1d98c1e23e9483a61fdd973d2af33538480ec1aee29fd33ec82224c9b14f035663bed6db11254245dfcda166d7bd10d7e687e549e4d066e920b3493fb}}</ref> | ||
Despite several researches it is not clear what | Despite several researches it is not clear what patients prefer. Some studies show that patients prefer a mechanical hoist, while other studies concluded that patients were more comfortable with a ceiling lift.<ref name=Johnsson>Johnsson C., Kjellberg K. & Lagerstrom M. (2004) A direct observation instrument for assessment of nurses’ patient transfer technique (DINO). Applied Ergonomics35 (6), 591–601.</ref> | ||
There have been several attempts to improve the passive hoists with help of robotics. One of the earliest attempts was in the period 1990-1992 in a study of Patrick A. Finlay (3). In this study it was recognized that several specification were needed. First the robot should be able to move the patient without | There have been several attempts to improve the passive hoists with help of robotics. One of the earliest attempts was in the period 1990-1992 in a study of Patrick A. Finlay.<ref name=Finlay>Finlay, P. A. (1992). PAM: a robotic solution to patient handling. Industrial robot, 19(3), 13-15.</ref> In this study it was recognized that several specification were needed. First the robot should be able to move the patient without causing injuries. Of course, every patient is different and especially patients that have to be moved with the hoist can have numerous of physical problems the robot has to take into account. The robot should also be able to collect the patient from a lot of different positions and move them to lots of other possible positions. Third, the robot should be able to move through a hospital without accidents. Finally, the robot should not work too slow, because nurses and patients otherwise find the waiting time not worth to use the robot. The decision was made to make it a nurse controlled device, to get the patients and nurses to slowly get used to it. | ||
A initial design for the robot, which was called the Patient Assistant for Mobility (PAM) was already made up: | A initial design for the robot, which was called the Patient Assistant for Mobility (PAM) was already made up: | ||
“The patient surface of PAM is made up of an array of slats or tines which, using a patented method of deployment, are able to be insinuated gently under the patient to support his/her weight and draw him/her onto the trolley surface. The patient surface has a Z-axis to adjust its height, is additionally articulated at the hip and knee joints, and can thus move to set the patient into a seated or other intermediate pose. (…) Sensors are used to monitor the stability of the platform, and as a useful by-product these are processed to provide a readout of patient weight. For patients with special nursing needs, selected tines can be disabled so that no contact is made with the corresponding part of the body. The patient surface has an autonomous acquisition capability, so that a single command enables a patient to be collected from a bed once the PAM is parked in approximately the correct orientation at the bedside. Articulation of the patient surface is normally in telemanipulator mode, but the PAM also contains a memory enabling details of patients and furniture to be stored, so that a collection and placement sequence can be played back whenever required.” (3) | “The patient surface of PAM is made up of an array of slats or tines which, using a patented method of deployment, are able to be insinuated gently under the patient to support his/her weight and draw him/her onto the trolley surface. The patient surface has a Z-axis to adjust its height, is additionally articulated at the hip and knee joints, and can thus move to set the patient into a seated or other intermediate pose. (…) Sensors are used to monitor the stability of the platform, and as a useful by-product these are processed to provide a readout of patient weight. For patients with special nursing needs, selected tines can be disabled so that no contact is made with the corresponding part of the body. The patient surface has an autonomous acquisition capability, so that a single command enables a patient to be collected from a bed once the PAM is parked in approximately the correct orientation at the bedside. Articulation of the patient surface is normally in telemanipulator mode, but the PAM also contains a memory enabling details of patients and furniture to be stored, so that a collection and placement sequence can be played back whenever required.”<ref name=Finlay>Finlay, P. A. (1992). PAM: a robotic solution to patient handling. Industrial robot, 19(3), 13-15.</ref> | ||
Although this project started the demonstrator phase in 1992, it is unclear what happened with PAM after that. | Although this project started the demonstrator phase in 1992, it is unclear what happened with PAM after that. | ||
Another attempt to improve the patient hoist was 2007, in a project led by Lakshitha Dantanarayana ( | Another attempt to improve the patient hoist was in 2007, in a project led by Lakshitha Dantanarayana.<ref>Griffiths, H. (2012). Adverse risk: a ‘dynamic interaction model of patient moving and handling’. Journal of nursing management, 20(6), 713-736.</ref> In this project the author developed a smart hoist in collaboration with the resident and carers of the residential care facility. Some adaptions they found to be useful were weight measurement, rear view mirrors, ability to monitor the environment and assisted manoeuvering. | ||
The researchers equipped a standard patient hoist with | The researchers equipped a standard patient hoist with cameras in the front, just above the floor to provide information about the part of the environment that is blocked from view by the hanging patient and implemented strain gauges into the design to measure the weight of patients. Other improvements were cameras to monitor the environment behind the carers and robotic wheels. The patient hoist also had a navigation assistance algorithm implemented. The main change however was that the patient hoist was motor driven, but still moved by applying forces to the handles. The force was measured by the hoist and a similar movement was applied by the motors. This ensured the hoist could be used intuitively, and the learning curve was short. | ||
Several users trials were executed, and the researchers implemented the feedback in the final design. There was no clear conclusion whether the smart hoist was better than the traditional hoist, but several points for improvement were found. | Several users trials were executed, and the researchers implemented the feedback in the final design. There was no clear conclusion whether the smart hoist was better than the traditional hoist, but several points for improvement were found. | ||
Besides the hoist other solutions for lifting patients are researched, like the HAL exoskeleton and the Japanese lifting robot RIBA, but those projects are beyond the scope of our research. | Besides the hoist other solutions for lifting patients are researched, like the HAL exoskeleton and the Japanese lifting robot RIBA, but those projects are beyond the scope of our research. | ||
== | == USE-aspects == | ||
This subject is in many ways related to USE-aspects. First of all there are many different stakeholders and users. The primary users are of course the patients and the nurses. The secondary users are the people who pay the hoist, in this case the hospital management and the government and the tertiary users are the maintenance people. The preferences of all these users have to be taken into account. For instance, the patients want the hoist to be comfortable, while the nurses want it to be easy to use. The hospital management wants the hoist to be made as cheap as possible and the maintenance people prefer that the important components are easy to repair or to replace. This can lead to conflicts since it can be difficult to take all these preferences into account at the same time. | |||
The focus of this project is therefore mainly on the preferences of the primary users. The main question is how the hoist can be improved so that it is less uncomfortable for both patient and nurse. An important aspect that will be taken into account in this research is the interaction between patient, hoist and nurse. The patients are a vulnerable group and being transferred with a hoist can be terrifying. The process however can also be bothersome for the caregiver. So important questions are: 'How does a patient want to be comforted?', 'Does this differ between different groups of patients?' and 'What does the nurse want?'. These are the kind of questions that will be answered in the research. The hoist however is not only a technical problem. A lot of these problems are actually more related to social or use aspects. | |||
== Research == | |||
=== Interviews === | |||
==== Interview questions ==== | |||
Before the interviews were taken a list with questions was made to ask about the desired information which could be obtained from the nurses and patients. After that several interviews were taken and the list was adapted a little (version 2) to answer new questions that had arisen during the research. | |||
[[ Questions for caregiver and patient ]] | |||
==== Collected interviews ==== | |||
In total five interviews were taken. All of them were with nurses who had experience with the passive patient hoist. Unfortunately no interviews with patients have been taken as this group was unapproachable. | |||
The first two interviews were taken with Petra and Lianne, both nurses from Buurtzorg, which is a private care institution. Another two interviews were taken with Linda and Rachelle, both interns in their last year of their nurse education. The last interview was taken with Lisan who works in a nursing home with patients who suffer from dementia. | |||
A link for the full versions of the collected interviews: [[ Collected interviews ]] | |||
==== Results of interviews ==== | |||
Several problems emerged from the interviews. Here the most important points that were made clear in the interviews are summarized per interview. | |||
===== Interview 1 ===== | |||
This interview states that interaction between patient and caregiver is very important to establish good collaboration and trust between them. | |||
Everybody should feel safe and comfortable while using the passive patient hoist. | |||
Whenever the patient feels scared or not secure a good explanation about the taken actions should be provided, so trust and feeling safe can be created within the patient. Therefore it is a good idea to implement a device that can recognize emotions of the patient to assist the caregiver at his work. The hoist is not always experienced suitable for both patient and caregiver. The patient often dislikes for example the lifting mat, because it can cut in the patient’s legs. The caregiver on the other hand finds it difficult to move the hoist over a unsmooth floor or in small rooms. Further, the caregiver does not stand very close to the patient while operating the hoist. | |||
===== Interview 2 ===== | |||
From this interview can be concluded that the use of the passive patient hoist is an improvement in comparison with lifting of patients manually by the caregiver in which for example back pain can be reduced or prevented. However the hoist is not perfect and consists flaws. Maneuverability of the hoist has proven to be a main issue. When working with demented patients interaction between them and caregiver is a bit different than with not demented patients. Direct commands and explanation about the taken actions are given to the demented patients to reassure them, but sometimes an explanation has no use for them, because they do not understand it. Therefore they are sometimes distracted with a stuffed animal to smoothen the lifting process. At the same time these patients do not always express whether they are feeling uncomfortable or scared. Caregivers try to make something out/read the facial gesticulation of the patients to estimate how they are feeling. A device that could determine their emotions and one that could distract or reassure them during the process would be of good use. | |||
===== Interview 3 ===== | |||
This interview shows that using the passive patient hoist is not an easy task in nursing homes. In these homes are often small doorsteps present which makes it difficult for the caregiver to drive over. During the transport process the visibility for the caregiver is deficient due to the post of the hoist. To prevent this limited view the caregiver walks alongside the hoist. However, this is also not very convenient, because it makes it more difficult to push the hoist with sufficient power. A device that improves this navigation process is reflected as a good idea. Another practical aspect is the lifting mat. This mat is not very pleasant for patients, because it sometimes cuts in the legs of the patient during the lifting process. Further, during the process these mats are provided with whalebones at the backside for extra support for the patient. This whalebones need to be inserted before the process starts and removed by the caregiver whenever the patient sits, because it is not comfortable for the backbone while sitting. A big issue with these whalebones is that they get lost very easily, because they do not have a fixed place at the hoist. | |||
During the lifting process interaction is again important. Whenever a patient feels uncomfortable he is asked what is wrong and all actions are explained extensively. It depends on the patient, whether they are comfortable with more interaction or less. | |||
===== Interview 4 ===== | |||
Social interaction between patient and caregiver remains a crucial element during the lifting process. A lot of eye contact is made between them and they converse during the process. Whenever a patient is not acquainted with the hoist or if the patient is scared the caregiver will communicate more and try to make more eye contact as well to reassure the patient. When the patient is familiar with the hoist less interaction between him and the caregiver is needed to put the patient at ease. A technical aspect of the hoist is that the battery is heavy and it’s lifespan is very short. Another hoist like the ceiling hoist would be more suitable in smaller rooms and steering is much easier. However it is not a practical solution for existing care homes, because rails need to be constructed all over the nursing home. | |||
===== Interview 5 ===== | |||
The main point that can be concluded from this interview is that interaction is an important, but also a difficult point. Especially since the patients are suffering from dementia they do not really understand what you are saying. Still it is important to keep communicating about what you are doing and to comfort the patient. This is also possible by touching the patient, by eye contact or by distracting them with a stuffed animal. Over time you learn to recognize whether the patient is uncomfortable, because you get to know them. It is very important for nurses to get to know their patients. The main problems with the hoist are that you have to do several things at the same time and it is heavy to turn and move the hoist when it is loaded with a patient. It is especially difficult to navigate the hoist safely through small spaces while watching the patient. | |||
=== Survey === | |||
==== Design of survey ==== | |||
'''Hypotheses:''' | |||
:- Both patients and caregivers prefer eye contact most in the process of caregiving during transportation in the hoist. | |||
:- Patients like to be comforted by voice interaction between patient and caregiver or between patient and someone else during the process of caregiving during transportation in the hoist. | |||
:- Patients like to be comforted by physical contact in the process of caregiving during transportation in the hoist and also caregivers prefer to have some extent of body contact during care giving. | |||
'''Design of the survey''' | |||
Link to survey: https://docs.google.com/forms/d/e/1FAIpQLScinjbrL8rMoxs1CQOP0JCgIO3u_tavH2K1LGRcKIa9q_bFVA/viewform | |||
==== Method ==== | |||
The code in Stata can be found by this link: [[Stata code]]. | |||
In the previous week (week 3) some data for the survey was already gathered and a power analysis was conducted. Since the standard deviation at that moment was around 0.7, this value is used for the power analysis, together with a power of 0.8 and an alpha level of 0.05. | |||
This showed that 24 to 32 respondents are needed to be able to see a significant result in the data. A mean difference of 0.5 points difference on the Likert-scale is used. The Likert-scale is the scale of 0 to 5 that was used in the survey. | |||
Then data was collected again, especially of patients, because there was not enough data of this group. A sample size of 29 participants for each group was gathered. | |||
The data was prepared for analysis, for example by giving proper names to the variables i.e. After that, the new standard deviation is determined. | |||
The following hypotheses were analyzed. | |||
:- What way of interaction receives most preference? | |||
:- H0: There is no difference in the need for interaction between patients and caregivers | |||
:- H0: There is no difference in preference for eye contact between patients and caregivers | |||
:- H0: There is no difference in preference for voice interaction between patients and caregivers | |||
:- H0: There is no difference in preference for body contact between patients and caregivers | |||
==== Results ==== | |||
Using the new standard deviation (again 0.7), the sample size (29 participants per group) and again an alpha level of 0.05, the power is calculated. The value of the power is 0.76, this value is all right. In an ideal case 5 to 10 more patient participants should have been collected, but the analysis is continued anyway as the power has proven to be good enough. | |||
Code: | |||
power twomeans 2 2.5, sd(0.7) n(58) alpha(0.05) //to compute power with given sample size -> 29 participants per group | |||
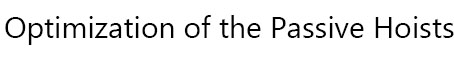
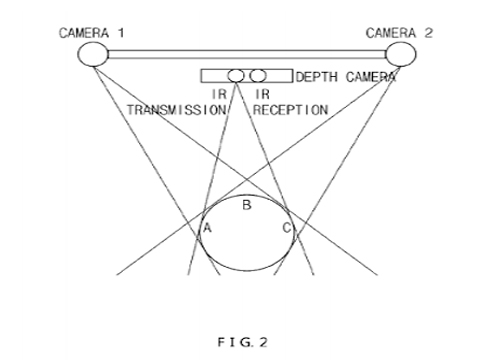
The results, shown in figure 1, are: | |||
Total mean for eye contact is 2.21, for voice interaction 2.24 and for body contact/interaction 2.75. The difference between patient and caregiver in eye contact is 0.05, for voice interaction it is around 0.5 and for physical contact it is 0.75. | |||
[[File:Result-interaction1.jpg]]Figure 1: Total mean values | |||
[[File:1.jpg]] Figure 2: T-test of interaction | |||
For the t-test of interaction by role of patient of caregiver, the t-value is 2.49 (fig. 2). There are 37 degrees of freedom and the p-value is 0.009. | |||
[[File:2.jpg]] Figure 3: T-test of eye contact | |||
For the t-test of eye contact by role of patient of caregiver, the t-value is 0.17 and there are 37 degrees of freedom (fig. 3). | |||
[[File:3.jpg]] Figure 4: T-test of voice interaction | |||
For the t-test of voice interaction by role of patient of caregiver, the t-value is 2.0 (fig. 4). There are 37 degrees of freedom and the p-value is 0.027. | |||
[[File:4.jpg]] Figure 5: T-test of physical contact | |||
For the t-test of physical contact by role of patient of caregiver, the t-value is 2.45 (fig. 5). There are 37 degrees of freedom and the p-value is 0.01. | |||
==== Discussion and conclusion of survey ==== | |||
The results mean: | |||
What way of interaction receives most preference? | |||
:Command: tabstat oog voice lichamelijkcontact, by(rol) | |||
Eye contact receives most preference. With body contact you see that patients do not really like it. The value of preference is higher, which means their preference is lower. Also, the difference with preference of body contact between patients and caregivers is quite high. | |||
What also turns out is that the preference for voice interaction is a little less for patients than for caregivers. This means that caregivers like talking to their patients more than patients prefer to talk to their caregivers. This is not what was hypothesized so further research will be done by using interviews and a t-test on voice interaction. | |||
H0: There is no difference in the need for interaction between patients and caregivers | |||
:Command: t-test interactie, by(rol) | |||
There is a significant result, which means the preference for interaction between patients and caregivers is not the same. The p-value is significant, so H0 is rejected. | |||
H0: There is no difference in preference for eye contact between patients and caregivers. | |||
:Command: t-test oog, by(rol) | |||
A t-test is conducted where the preference for eye contact is compared between patients and caregivers. There is no significant result because the p-value is not significant. This means that H0 cannot be rejected, so there is no difference in preference for eye contact between patients and caregivers. | |||
H0: There is no difference in preference for voice interaction between patients and caregivers | |||
:Command: t-test voice, by(rol) | |||
A t-test is conducted where the resulting p-value is 0.03. This value is below 0.05 which means that H0 can be rejected, so there actually is a significant difference in preference for voice interaction between patients and caregivers. However, this resulting p-value is not very far below 0.05, therefore it is not completely sure whether this difference is significant. | |||
=== | H0: There is no difference in preference for body contact between patients and caregivers | ||
:Command: t-test lichamelijkcontact, by(rol) | |||
This final t-test shows a large significant result, a significant p-value. This means H0 can be rejected and there is a difference in preference for body contact between patients and caregivers. Patients prefer this way less than caregivers. | |||
Noldus company for face detection software is contacted for a free trial software. Via telephonic contact Noldus promised to send this trial version as soon as possible. | |||
== Analysis == | |||
From both the survey and the interviews several things can be concluded. First a answer the question whether our hypotheses were true or not will be provided. | |||
'''Caregivers need to be supported by the patient hoist''' | |||
From the interviews can be concluded that caregivers do not really need to be supported by the patient hoist, they can manage without, but it could help much. Nurses have indicated that especially a hoist that helps with navigating through small spaces would be of great help. Thus the hypothesis that nurses would need to be supported by cameras for navigating can be confirmed. It is less clear whether the second sub-hypothesis, “Caregivers need a patient hoist that can navigate itself and avoid obstacles” can be confirmed. Nurses have mentioned that they would like to have help with navigating, but none of them mentioned they would like the hoist to move by itself. At least one of them, Lisan, has mentioned an aversion for a self-moving hoist. She was convinced a nurse should always be present. So it can be concluded that this sub-hypothesis is untrue. Not much consensus was found on the third sub-hypothesis: “The caregiver would like to be warned by the patient hoist whenever the patient is anxious”. Some nurses mentioned that it could be handy, but other nurses mentioned that this is the task of the caregiver and by getting to know the patient a caregiver could identify by herself whether the patient was anxious. So this hypothesis can neither be confirmed nor rejected. The fourth sub-hypothesis “Patients appreciate it when they are reassured by the patient hoist whenever they are anxious” can also neither be confirmed nor rejected, because it was not possible to interview a patient. As patients a very vulnerable group, the nurses did not want them to be interviewed. The last sub-hypothesis was: ”Caregivers need a patient hoist that can provide information about the weight or the 'BMI' of the patient”. One nurse mentioned it would not be necessary, because they weigh the patient already once a month. However, the other nurses never gave a clear answer to this question and therefore it can neither be confirmed nor rejected. | |||
'''Patients and caregivers attach value to interaction during the process of lifting.''' | |||
This hypothesis was examined by a survey. From this survey and the interviews can be concluded that most patients and caregivers do indeed attach much value to interaction during the lifting process. In the interviews it was mentioned as one the most important aspects of the tilling process. From the survey can be concluded that both patients and caregivers prefer eye contact most during the process of caregiving. This is also what was hypothesized. Results of the survey show also that both caregivers and patients like to have voice interaction to some extent. However, the preference for voice interaction is significantly larger for caregivers than for patients. Patients do prefer voice interaction, but to a much lesser extent than caregivers do, and also to a much lesser extent than was hypothesized. For body contact there is a large significant difference in preference for caregivers and patients. Patients actually dislike body contact during the process which was not hypothesized. From these results it can be concluded that eye contact is the most important factor of interaction during caregiving. This will be used to optimize interaction in the process of caregiving during transportation in the patient hoist. Voice interaction is less important for patients, but this can also be taken into consideration in the design for optimizing the patient hoist. | |||
'''Problems''' | |||
As the hypotheses are now answered, the main problems of the current design can be identified and requirements that the improved design must meet can be proposed. | |||
A lot of nurses have mentioned that they have trouble with moving the hoist. A lot of these problems were caused by wheels that got stuck. The swivel caster wheels, which are currently used, do not roll as smoothly as hoped. This is caused by a rough surface or the orientation of the wheels. Therefore the first requirement for the new design is that ''wheels are used that do not get stuck''. | |||
Another problem that many nurses encountered was that the hoist was heavy to push when loaded with a patient. It was also very difficult to turn the patient or the arm of the hoist when also focusing on the wellbeing of the patient. That is why the following two requirements were set up: | |||
''Less force should be needed to push the hoist'' and ''less force should be needed to move or turn the patient when loaded in the hoist''. | |||
From the hypotheses can also be concluded that nurses do have trouble with moving the hoist around in small spaces and would like some assistance with that. It is difficult for the nurse to keep an eye on everything, mainly because the patient is blocking a significant part of the field of sight of the nurse. This leads to the fourth requirement: ''The hoist should give a better overview to the nurse during the transfer''. | |||
A conclusion that was drawn from the survey was that patient and nurses value eye contact during the transfer for a great deal. However, on longer distances where the patient is facing towards the moving direction of the hoist there is no eye contact at all. This can lead to a less comfortable experience for the patient, that is why another requirement holds that ''during the whole process eye contact between the patient and the nurse is guaranteed''. | |||
Another problem that was examined was whether the nurses would like assistance with recognizing whenever the patient is uncomfortable. Although some mentioned that a nurse would learn this by time, for inexperienced nurses recognizing anxiety can be a challenge, because the patients are not always able to express their feelings. That is why it is likely that the following requirement still can be an improvement to the hoist: ''The hoist should be able to recognize anxiety in the patients''. | |||
The last requirement is: ''The hoist should be able to comfort the patient''. It was not possible to examine whether the patients would like this, but especially since the design could be a bridge between the current lift and full automated one, it is likely that it can add something important to the hoist. | |||
== Requirements == | |||
In this section the best solutions for the earlier stated requirements will be discussed. | |||
'''Requirement a: During the whole process eye contact between the patient and the nurse is guaranteed. ''' | |||
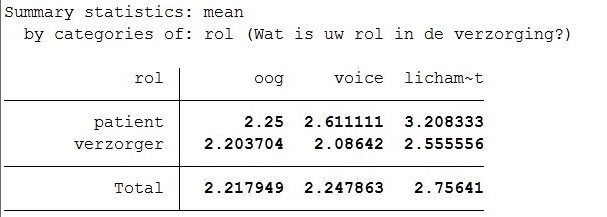
One way to realize this is by the use of cameras and displays. A patient, who is sitting in the lift, can be filmed by a camera. This images are transferred to a display that is attached to the back of the lift where the nurse is standing, who is also filmed. The patient also should have a display in sight, so eye contact can be established at all time. However, when you look at a screen, you do not look in the camera. This is because they are at two different places. For this reason, eye contact via videos is difficult. However, there has been a lot of research on improving video-mediated communication. As stated in “eye contact and video-mediated communication: a review”<ref>Leanne S. Bohannon a,⇑ , Andrew M. Herbert b , Jeff B. Pelz c , Esa M. Rantanen, Eye contact and video-mediated communication: A review., file:///C:/Users/s130798/Documents/School/Year%203/Robots%20everywhere/Literatuuronderzoek%203-10/1-s2.0-S0141938212001084-main.pdf</ref> video-conferencing has become a popular video technology because it improves real-time communication. Video-conferencing is a richer form of communication than email or telephone, however, the authors says that video-conferencing is not quite as informative as face-to-face communication. Some research was done about ways to improve video-conferencing and eye contact during the use of webcams. Franc Solina and Robert Ravnik proposed a method related to the mona lisa effect.<ref>Todorović D. Geometrical basis of perception of gaze direction. Vision Research 46:3549-3562, 2006 | |||
</ref> This method establishes eye contact during video calling and it used big screens and cameras mounted above the screen.<ref>Franc Solina, Robert Ravnik, Fixing Missing Eye-Contact in Video Conferencing Systems, http://ieeexplore.ieee.org.dianus.libr.tue.nl/stamp/stamp.jsp?arnumber=5974027</ref> However, a still better method must be possible. Stereo matching method, shown in figure 6, is a method that could solve our problem. With stereo matching a color image is used in a stereo camera as an input. This is configured by two cameras, they create a reference point.<ref name=Hwang>Hwang et al. method and apparatus for providing eyecontact function to multiple points of attendance using stereo image in video conference system, 2016, http://www.freepatentsonline.com/20160150182.pdf</ref> However there is a problem with stereo matching, since most of the stereo matching methods only consider paired images in specific orders. To treat video images of stereo matching as a static image causes flickerings.<ref> Jinglin Zhang Cong Bai Jean-Francois Nezan Jean-Gabriel Cousin, Joint motion model for local stereo video-matching method,2015, | |||
http://opticalengineering.spiedigitallibrary.org.dianus.libr.tue.nl/article.aspx?articleid=2478969</ref> | |||
[[file:Eye_contact1.jpg]] | |||
Figure 6: Stereo matching method | |||
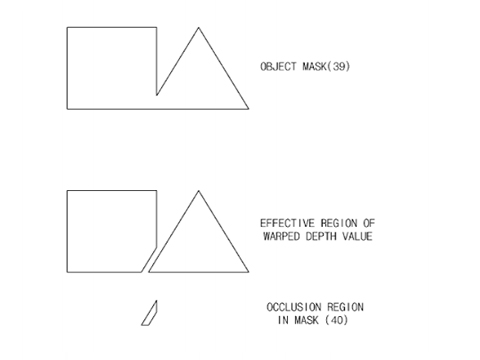
Recently, a patent for “Method and apparatus for providing eye contact function to multiple points of attendance using stereo image in video conference system” has been proposed.<ref name=Hwang>Hwang et al. method and apparatus for providing eyecontact function to multiple points of attendance using stereo image in video conference system, 2016,http://www.freepatentsonline.com/20160150182.pdf</ref> The patent presents an invention to improve eye contact. It improves eye contact images between remote attendances during video calling. Since this invention is not on the market yet, this will not be included in the demo, but for future use this aspect is very important. This method uses the same ideas as stereo matching, two cameras are used. However in advance to that, a depth image camera is also used, this is to calculate the occlusion region. With this information, an object mask for an image is created. The completed object mask is the way in which eye contact can be improved. Figure 7 shows an illustration of this. | |||
[[file:Eye_contact2.jpg]] | |||
Figure 7: Object mask | |||
'''Requirement b: Less force should be needed to move or turn the patient when loaded in the hoist.''' | |||
The patient loaded in the hoist should be easy to turn. In the interviews was mentioned that some nurses had trouble with turning the hoist in the right direction, while also making sure the hoist does not bump into something. The patient is turned by hand, which means all the applied force comes from the nurse. This could be made easier by also using an electromotor to turn the harness to which the sling is attached. For this user intention recognition will also be used, for the same reasons as mentioned above. To recognize the intention of the nurse the hoist needs a force control system. Usually force control is used in robots that have to pick up objects. It makes sure the robot does not squeeze anything. It does this by measuring the opposing force the object applies to the robot when the robot picks up the object. A feedback loop is used to ensure the robot responds in the correct way to the opposing force. This force control can be implemented in the hoist, so that the bigger force the nurse applies, the longer the robot continues this movement. To measure this force, force or strain sensors have to be implemented on every joint of the hoist. A computer measures this force and with the implemented logic determines the motion and velocities. Major motion patterns have to be identified and implemented in this computer, to ensure the hoist continues its movement in the same direction as the nurse applied the force in. | |||
'''Requirement c: Less force should be needed to push the hoist.''' | |||
The nurses mentioned in the interviews that they had trouble moving the hoist around in the rooms, because it was so heavy, especially when the patient was sitting inside the yoke. Sometimes the floors made it even more difficult to push the hoist forward. So it can be concluded that the improved hoist should have the ability to move without the nurse applying all the force. This is especially important when the hoist is used for larger distances, like moving the patient to the toilet or to another room. Our solution is to build in an electromotor to drive the wheels. This means the hoist requires a stronger battery. It was decided to not use a remote to steer the improved hoist, because that would add extra complexity to the hoist. The nurses would have to learn yet another thing. The learning curve needs to be kept short, so user intention recognition will be used to steer the hoist. This means the hoist anticipates on the intentions of the nurse by measuring how force is applied. For the nurse it means she can use the hoist the same way she was used to. More explanation of this can be found in requirement b. | |||
'''Requirement d: The hoist should be able to recognize anxiety in the patients.''' | |||
There are several ways a machine can recognize emotion in humans. One of the most obvious ways is of course the same as most humans do it, by reading a person's face. Software that is able do this already exists and is called facial expression recognition software. Reading the face by looking at the position of, for instance, the mouth and the eyes has proven to not work well enough, because every person is different. That is why these software analyze the relationship between points on the face. When somebody curls the corners of his/her mouth, the software registers that the point of the corner of the mounts moves. With a complex algorithm it concludes that the person expresses, to a certain amount, happiness. It is even possible for these software to recognize micro-expressions. Most of these software show the extent to which a person shows one of the seven basic emotions in percentages. The seven basic emotions these software uses are: joy, sadness, anger, fear, surprise, contempt, and disgust. Often a Neutral emotion is also added to the possible emotions. More complex emotions are always regarded as a combination of these seven emotions <ref>http://nordicapis.com/20-emotion-recognition-apis-that-will-leave-you-impressed-and-concerned/</ref>. It is therefore more difficult to recognize these emotions in the numbers the software generates. However, since the software only has to recognize fear, it could be accurate enough for the goal of this research. Of course there are also other ways to recognize a person's emotions. Other aspects researches often take into account are respiration and heart beating. MIT<ref>Zhao, M., Adib, F., & Katabi, D. (2016, October). Emotion recognition using wireless signals. In Proceedings of the 22nd Annual International Conference on Mobile Computing and Networking (pp. 95-108). ACM.</ref> has written a paper about a new technology that can detect the emotion of a person by analyzing reflecting radio frequency signals of a body, which means that no sensors need to be applied. The EQ-radio sends a RF signal through the room, recognizes the person from the other objects, analyzes its reflections and recognizes his emotional state. This all is done by a new underlying algorithm that extracts individual heartbeats from the wireless signal. The accuracy of the emotion recognition is comparable with state-of-the-art emotion recognition systems that need a person to be hooked to an ECG monitor. For the design the facial expression recognition software will be used. The main reason for this is that this technology is already more developed and many different software are available. This makes it easy to implement in the design. The only things needed for this are software, cameras and a computer. Since the computer is also needed for other aspects of our design a computer will be implemented anyway. The camera is also already implemented for making eye-contact with the nurse. It is decided to go with the facial expression recognition software of Noldus. After contacting them a trial version of their software was obtained. | |||
'''Requirement e: The hoist should be able to comfort the patient.''' | |||
It was already stated the hoist should be able to recognize fear in the patient, but the hoist should also be able to react on it. It was already mentioned that a screen is attached to the hoist on which the patient can keep contact with the nurse, when the patient is moved. This screen can also be used to comfort the patient. One thing that was concluded from the interview is that it is important to tell the patient what is happening to him. So a feature is implemented in the hoist that can tell, either with spoken words or written on the screen, what is happening to the patient at the moment he/she is scared. The nurse should be able to turn this feature on and off at any moment. Another thing that was learned from the interviews is that a lot of patients who have to be transported by a hoist have dementia. They do not understand what the nurse is saying to them. Therefore they will not understand the hoist either when words are spoken or written on the screen to explain the taken actions. An option for them could be, that the screen on the hoist shows an animation which can distract the patient. This should also be a feature that the nurses should be able to turn on and off at any moment. | |||
'''Requirement f: The hoist should give a better overview to the nurse during the transfer.''' | |||
This problem can be solved by the use of a camera, which is placed at the front of the lift and films in the moving direction of the lift. Transferring these images to the display of the nurse, he/she can easily see what is in front of the lift and if there are any obstacles that could be possibly dangerous. Another addition would be sensors that indicate how close the lift is to a certain object, for instance a wall, so the nurse has an even more complete overview. These sensors, often used in cars for parking assistance, use super sound to determine the distance between the sensor and an object. If a minimum distance is exceeded the nurse will get a signal on het screen and the hoist will break automatically to prevent collision. However, since this partly takes away the control the nurse has, it was decided to go with the cameras. Maybe in the future when nurses and patients are more familiar with automation and robot technology, parking sensors could still be implemented. | |||
'''Requirement g: Wheels that do not get stuck are used.''' | |||
A solution for this is to use solid spherical wheels, which are part of a ball bearing. Since these wheels can move freely in every direction they will not get stuck due to orientation and can as well move over surfaces which are rough. Since these wheels do not have an axis around which they turn, it is difficult to support them with an electromotor. Therefore these wheels are mainly useful as replacement for the front wheels of the patient hoist. | |||
Finally, in the interviews it was mentioned that the whalebones get lost easily. That is why a small adjustment will be added, besides the requirements. A pocket to the hoist to store the whalebones in will be attached. | |||
== Design 1 == | |||
[[File:DesignPassive.png|800px|Figure 8]] | |||
Figure 8: Design 1 | |||
[[File:InterfacesPatient.png|thumb|250px|Figure 9: Interface options for patient]] | |||
An optimized design for the hoist is made with the program Photoshop CS6 (fig. 8). In this design the requirements were taken into account and added to an adapted version of the 'Wendy' passive hoist. | |||
:1. (Following requirement a) | |||
:Screen display that is able to sustain a live connection between the caregiver and the patient by an implemented camera. The software on the display is able to show information about the patient in the hoist. | |||
:2. (Following requirement b) | |||
:Force sensors in handgrips that are able to measure how much force the caregiver is applying while pushing the hoist. | |||
:3. (Extra requirement) | |||
:Emergency stop button for the caregiver that will immediately shut down all the systems of the hoist when pressed. | |||
:4. (Following requirement c) | |||
:Electronic powered motor that, in combination with the force sensors, move the hoist by amplifying the force of the caregiver in a certain direction. | |||
:5. (Following requirement d) | |||
:Camera with a real-time connection pointed at the face of the patient, to sustain eye contact. The camera is also connected with the facial recognition software to detect the emotions of patients. | |||
:6. (Following requirement e) | |||
:Screen to comfort the patient and make eye contact with the care giver. | |||
:7. (Extra requirement) | |||
:Holder for the stiffeners. | |||
:8. (Following requirement f) | |||
:Camera to create a better view of the environment. The caregiver is more able to spot if there are object obstructing the path of the hoist. | |||
:9. (Following requirement g) | |||
:Spherical wheels for better manoeuvrability. | |||
1. | The improved patient hoist (I.P.H.) in our design 1 is equipped with two interfaces, that will now be evaluated further. There is one interface for the patient (nr. 6 in Design 1) and one for the caregiver (nr. 1 in Design 1). | ||
'''Interface patient:''' | |||
The interface for the patient is sketched in figure 9. This will be a display, like for example a tablet. To fill up this display three options can be chosen by the patient and caregiver. In this case they have both control over how they are supported by the added technology. | |||
The first option is that the caregiver is visible for the patient on the display so eye contact between them can be obtained. This is an improvement in comparison with the current patient hoist in which, like in scenario 2, there is no direct eye contact possible between patient and caregiver during the transportation. | |||
The second option consist of the first option with an extra window on the display. This window shows a short animated film clip with a speech function in which the actions of the lifting process are explained to the patient. This option is implemented, because results of the survey and interviews showed that patients like to be informed about what is happening and going to happen during the process. As the patient wishes this option can be switched on or off by the caregiver. | |||
A third option can be implemented to the first option in case the process is executed with for example a demented patient. In this case the display contains an extra window in which an animation is showed to distract the patient during the process. Consequently the process will go more smoothly and pleasant for both patient and caregiver. | |||
All options can in fact be put on or off by the caregiver in compliance with the patient leading to actually four options for the interface of the patient. | |||
[[File:InterfaceCaregiver.png|thumb|250px|Figure 10: Interface caregiver]] | |||
'''Interface caregiver:''' | |||
The interface for the caregiver is shown in figure 10. This will also be a display, like for example a tablet, which will be attached at the backside of the patient hoist at face/shoulder height of the caregiver (nr. 1 in Design 1). This display can be changed of position (up and down) so even a tall or a small caregiver can use it properly. On this display the patient lying in the yoke is visible for the caregiver, so eye contact between them can be accomplished. In another window an overview of the environment just in front of the hoist will also be visible on the interface. Due to this the caregiver can easily see what is in front of the hoist and if there are any obstacles that he cannot see for himself from behind the hoist. Further, on the right side of the interface a kind of traffic light system will be visible. This traffic light displays the well-being of the patient during the lifting and transport process. The traffic light is connected to the camera of the patient (nr. 5 in Design 1) which can due to the implemented software of Noldus recognize facial emotions of the patient. | |||
Green light shines when the patient is feeling good and comfortable. In this case the caregiver does not need to change his procedure, the patient is doing just fine in the yoke. Orange light lights up whenever the patient is a little uncomfortable, but the caregiver does not necessarily need to take any actions or alter the transport process for the patient. The caregiver just needs to be more alert, because the chance of changing from orange to red light is higher. The red light shines when the patient is not feeling good, he is scared or uncomfortable. In this situation the caregiver should give attention to the patient and figure out why he is feeling uncomfortable and take action to change this feeling. | |||
The distinction between which color light should shine when will be determined by the results of the test plan for the used facial recognition software of Noldus. | |||
== Noldus == | |||
In this section the facial expression recognition software 'FaceReader 7.0' from Noldus will be looked into. First a measurement plan is discussed, after which the results are presented after analysis. Lastly conclusions regarding this software will be drawn. | |||
===Measurement plan=== | |||
The goal of this measurement plan is to create a guideline for the two experiments that will be carried out. This will result in a smoother transition between acquiring the materials necessary for the set-ups, performing the experiments and exporting the data. | |||
With the first experiment it is possible to verify if the impact of different circumstances results in a deviant output. What will a difference in distance, angle or light/dark ratio do to the results? | |||
With the second experiment the performance of the Noldus software will be verified by testing a range of basic emotions, by using certain movie segments. Experimental participants (varying in age) are positioned in front of a camera, while being exposed to fragments of themed video material. Key is to execute the experiments with comparable circumstances. | |||
The specific steps that should be taken can be found in the linked file below. | |||
[[ Measurement plan ]] | |||
=== Validation of Noldus === | |||
After the experiments were executed the facial expressions had to be analyzed. How this is done is discussed in this section as well as the results of both experiments. | |||
====Method==== | |||
The recordings of the participants are analyzed using Noldus software and their feelings were asked and written down. By combining these two factors and the literature about the movies, it will be determined whether the Noldus software gives valid data about facial expressions. | |||
After the analysis is completed the data can be exported to a .txt file where for every time sample the intensity of every emotion is given. This intensity varies from 0, not present, to 1, fully present, whereas the sum of every emotion never exceeds 1. | |||
For every recording where one specific emotion should have been generated, a matlab script ([[File:Analysis.pdf]]) determines the mean intensity and maximum intensity. Next, the mean of these means as well as the mean of these maxima were calculated and the standard deviation is determined. | |||
Finally, both values for all emotions are plotted, with and without taking neutral intro account, leading to four figures (fig. 13-16). | |||
It can be concluded that the Noldus FaceReader software is valid if the highest mean and maximum emotion is the emotion that is expected from reporting of participants and from the literature. | |||
===Results=== | |||
====Experiment 1==== | |||
By daylight the software was able to detect the face of the participant until a distance of 2 meters between the webcam and the participants face. | |||
By daylight and 0.5 meter distance between the participant and the webcam the software was able to detect the face that was turned right until an angle of 45 degrees was reached. The same holds for turning the face to the left. Turning the face down the software was able to detect the face until an angle of 20 degrees, whereas the software kept on detecting the face when looking up until the neck of the participant was fully stretched. Increasing the distance led to an increase of allowable error in every direction. | |||
By changing the dark/light ratio is was observed that the software is very sensitive to light. By daylight there are no problems, however in a slightly darker room, where the curtains are closed, the maximum distance between the face and the webcam decreases rather fast, as well as the allowable angle. Turning light right into the camera has the same effect. | |||
==== Experiment 2 ==== | |||
First one has to note that the movies that are selected in the research show strong emotional responses, but not facial expression responses as these emotional responses were determined by measuring heart rate and respiration. So there is a chance that not much responses will be shown in the tests, but this does not mean that the software is not valid. Furthermore it is mainly focused on analyzing only the most important emotions for this project, meaning happy, sad and fear. | |||
Figure 13 shows the analysis of the sad movie. What stands out is that neutral is minimally twice as high as the other emotions. This can be due to the selected movie as not every moment was sad. When the neutral emotion is neglected it is shown that sad is indeed the main mean emotion. For this reason in the next analyses the focus lies on the graphs where neutral is filtered out. Happy is also quite high in the maximum emotion graph. This is a striking result, because it could mean that in the software a sad emotion is easily confused by a happy emotion. This could however also be due to a high intensity of happiness at some point, because the happiness in the mean graph is not that high at all. Also anger is somewhat higher than the other emotions, however none of the participants reported feelings of anger so this might be an error in the software. Nonetheless, sadness and anger are on the same side of arousal in the valence arousal model so this also is a very plausible observation. | |||
Figure 14 shows the analysis of the happy movie. It can be seen that the values of happy are high. The mean of happiness is even similar to the mean of neutral and the max is even higher. When neutral is neglected, a peak is visible in sad emotions, however happy still is twice as high. As in the previous figure sadness also was confused with happiness it can be stated that the recognition of Noldus needs some improvement. Happy and sad seem to be coherent in the software to some extent. Nonetheless, it can be concluded that the software of Noldus appropriately reports happiness as the main emotion when participants also report happiness. | |||
{| | |||
|- | |||
| [[File:Sad analysis.jpg|thumb|none|alt=ALT|800px|Figure 13: Analysis of sad movie]] | |||
| [[File:Happy analysis.jpg|thumb|none|alt=ALT|800px|Figure 14: Analysis of happy movie]] | |||
|} | |||
The most important emotion for improvement the hoist is scared. Therefore two analyses of this emotion were conducted. Scared 1 shows fearfulness over a longer period of time and Scared 2 shows a very brief moment of shock. As visualized in Figure 15, happy is the main mean emotion besides neutral. Furthermore, the second highest mean emotion is sad. This is not as expected. In Figure 16 the sudden shock is analyzed. This is another way of measuring fearfulness. Contrary to the scene of the shining, in this movie happy is not high. Neutral on the other hand is high, but this is neglected. Visible again is that sadness is high instead of the scared that was expected. Also disgusted is slightly higher than the other emotions. Disgust can be difficult to distinguish from fear, because jaw drops and eyebrow changes. The emotions on one side of the valence level are often somewhat confused, but there is little confusion between the negative of positive valence levels. | |||
= | {| | ||
|- | |||
| [[File:Scared1.jpg|thumb|none|alt=ALT|800px|Figure 15: Analysis of scared 1 movie (the shining)]] | |||
| [[File:Scared2 analysis.jpg|thumb|none|alt=ALT|800px|Figure 16: Analysis of scared 2 movie (sudden shock)]] | |||
|} | |||
===Conclusion=== | |||
By daylight and an angle between the face that should be detected (in the allowable range of left/right: 45 degrees, down:20 degrees and up: 60 degrees) and the webcam, the software is able to detect the face without any problems. As soon as more or less light is available the software’s performance is decreasing. A solution for this could be to attach a light near the camera that shines on the face of the patient in the patient hoist, so the software is able to detect the face, even when the room is dark | |||
What mainly can be concluded is that the Noldus Software did not always respond as expected. Reasons for this could be because small facial changes of, for example, fear are very hard to observe, the movie fragments were not good and long enough to arouse certain emotions or the participants were too much influenced by their environment to take the experiment seriously. However, something else is standing out. The software might not show the precise emotion accurately, because mainly happiness, sadness and neutral were reported, but the level of arousal on the other hand is quite precise. When Noldus reports neutral the level of arousal is 0, for negative emotions the level becomes negative and for positive emotions the level becomes positive. Negative arousal emotions are anger, sad and disgust while positive arousal emotions are happy and surprise. This can be seen from the valence arousal model of Russell. In the analysis it can be seen that the emotions on one side of the valence level are often somewhat confused, but there is little confusion between the negative and positive valence levels. For this reason, and also due to the fact that the received software only exports data from which valence can be determined, the “traffic light” system mentioned above will be based on the level of valence instead of the specific emotion. The next section will more elaborate on this. | |||
===Emotion detection=== | |||
As explained above, distinguishing different specific emotions lead to complications, which are undesirable. So, instead of focusing on these specific emotions and whether this one emotion exceeds a certain intensity, valence is used to determine the state of a patient’s emotion. (Arousal is not taken into account, since the software received from Noldus is not able to output the activity of the Action Units, which are needed to be able to calculate arousal). To calculate valence the intensity of positive emotions, like happy, as well as negative emotions, like anger, fear, sad and disgust, are needed for every time sample (surprise is not taken into account since it can be positive and negative).<ref>Loijens, L. and Krips, O. FaceReader: Methodology Note, Retrieved from http://www.noldus.com/files/file_manager/downloads/whitepaper/FaceReader_Methodology.pdf</ref> Consequently, valence is the subtraction of the intensity of happy and the highest negative intensity, leading to a range for valence from -1 to 1, where -1 is purely negative and 1 purely positive. Using this, the idea of a traffic light system on the nurses display can now be realized, as can be seen in the figure below. The matlab script is given in this file: [[File:Trafficlight.pdf]] | |||
The traffic light given in Figure 17 is green when the valence is higher than 0.3, red if it is less than -0.3 and yellow when the valence is in between. This treshold can be varied for every patient personally. | |||
{| | |||
|- | |||
| [[File:Trafficlight.PNG|thumb|400px|Figure 17: The traffic light system]] | |||
|} | |||
== Demonstration == | |||
The purpose of the demonstration is to form a clear image of the future vision of the improved hoist. The invented adjustments that have been examined in the last few weeks are also implemented. | |||
Here a link to the created short film clip of the demonstration is given: https://www.youtube.com/watch?v=r1jxQCQQBQQ&feature=youtu.be | |||
== | == Feedback == | ||
To verify whether the implemented adjustments on the passive patient hoist shown in Design 1 are successful enough, feedback has been gathered from several caregivers who are acquainted with this hoist. Two of these caregivers have also taken part in the interviews at the beginning of our research, so they were a little bit more informed about the project already and three new caregivers were asked for feedback. | |||
The feedback was gathered by first briefly explaining to the caregivers what our research is about and how our arranged requirements are implemented in our first design. Secondly Design 1 with the several invented interfaces were shown to the caregivers and per adjustment was explained why it has been implemented. The caregivers were asked to give their opinion about the adjustments and whether they would adjust or add anything to the design. | |||
The results per feedback interview are listed below and a general conclusion from these feedback interviews is concluded. | |||
==== Feedback 1 ==== | |||
From this feedback interview can be concluded that our adjusted design of the passive patient hoist is indeed a good improvement. The bigger wheels actuated by a motor are very convenient as it reduces the required power of the caregiver to move the hoist, because it is not an easy task to push the current hoist with a patient in the yoke. The solid spherical wheels in the front of the hoist are also considered as handy since they make it easier to turn the hoist in another direction. The emergency stop is already implemented on the current hoist, however the position of this button is too low. The one shown in the design has a better position in the working space of the caregiver. The camera for navigating the hoist is regarded as a good adjustment. Especially with for example cables lying underneath beds etc. it is a fine implementation that can make spots visible for the caregiver and it can prevent collisions. This camera can be of good use for distances in one small busy room as well as for the transportation process. The addition of a holder for the whalebones of the lifting mat is considered very clever, even though it is such a simple adjustment it is really a good one, because the whalebones are now in no way connected to the hoist. The interface of the caregiver can support the caregiver in his tasks, although the caregiver should be able to open or close windows however he prefers. The traffic light system makes the caregiver extra alert which is therefore an advantage to provide good care. The options for the interface of the patient should all be possible as every patient is different and it should again be possible to switch options on or off. The control over these options should be given to both caregiver and patient, as long as patients are able to use these digital methods. An extra improvement for this design could be a kind of peg adjusted on the hoist so the lifting mat can be hung up on. Now the lifting mat is just thrown over the hoist which makes it easier to be worn out and whenever there is just a small hole in the mat it may not be used anymore because of safety aspects. The overall impression of the design is therefore positive and it will be an advantage for both patient and caregiver. | |||
==== Feedback 2 ==== | |||
The feedback from this interview is quite similar to the first one. The motorized wheels are considered as a real advantage for the caregiver. It can prevent back pain for the caregiver as it reduces their needed strength to push the hoist. The spherical wheels are just as in feedback 1 found very handy so turning the hoist in the desired direction will not be an issue anymore. It is found strange that those spherical wheels are not implemented yet or in more other equipment like for example a wheelchair. The position of the safety button in the design is more suitable than the current position, especially when more electronics are implemented it is important to be able to switch the hoist off. The camera for navigation and the holder for the whalebones are considered as a good addition just like in feedback 1. For the interface of the caregiver again the same good feedback was provided, however now the question arose whether it was possible for the used software of Noldus to determine the emotions of patients who have a facial paralysis or a defacement. Further the approach of a traffic light system to warn the caregiver is just fine, however instead of different light colors also smileys could have been used or something similar considering caregivers that are colorblind. The options for the interface of the patient are a good implementation to ease them when they are not feeling comfortable or scared. It depends on the patient which option will be chosen and this should be chosen by the patient if possible. Option three for demented or retarded patients is good, because an animation can distract them, however the animation should be chosen with care, because some subjects are sensitive. | |||
1 a | |||
==== Feedback 3 ==== | |||
The overall impression about the improved design was stated as positive during this interview. The motorized wheels are a good idea, however they should be carefully tested especially in small rooms. The motorized hoist and the strength by which the caregiver pushes the hoist should be well adjusted to each other, so the hoist does not react jerky or moves to fast and risks to bump into things. The spherical wheels, the emergency button, the camera for navigation and the holder for the whalebones are all considered as good adjustments in the current design of the passive hoist. Option one (visible caregiver), three (visible caregiver and a short film clip for distraction) and four (different options combined or switched on and off) for the interface of the patient are useful supplements and can either improve the interaction between caregiver and patient or comfort the patient more during the lifting process. Option two (visible caregiver and a short film with instruction) is on the other hand not necessary. Not all patients will understand these kind of instruction film and as a caregiver you provide these instructions yourselves to the patients verbally. The interface of the caregiver is also a good adjustment to improve the interaction between patient and caregiver and it can smoothen the whole process by giving feedback about a patient’s condition with the traffic light system and by giving information about the badly visible surroundings just in front of the hoist. However questions arose whether the used software to detect facial emotions will be useful for patients with for example Parkinson’s disease and whether caregivers will not focus too much on the interface instead of the whole hoist so the risk of collisions will increase while moving the hoist. | |||
At the end another option for a more future design for the interface of the caregiver and the control of the hoist was given. Instead of pushing the hoist by the caregiver himself, it should be driven by using something like a IPad by the caregiver. In this case the caregiver can walk next to the hoist and the patient while stirring the hoist from the IPad. Interaction between caregiver and patient will be improved by reducing the distance between them and the workload for the caregiver will decrease as he does not need to push the hoist manually anymore. | |||
==== Feedback 4 ==== | |||
From this interview can be concluded that the made adjustments in the current hoist are good and useful to improve the lifting process. Especially the motorized wheels in combination with the spherical wheels in front of the hoist are a very big improvement. The turning and pushing of the hoist is now experienced as hard and even more difficult then moving a full and heavy shopping cart. The motorized and spherical wheels will make this process a lot easier by reducing the workload of the caregiver. The emergency button, the camera for navigation, the holder for the whalebones and the interface of the caregiver are considered equally as in feedback 3. The options for the interface of the patient is also evaluated the same as in feedback 3 where option two should be omitted. Option three is a good option for comforting and distracting the patient, but no animation should be used. Instead a short film clip about nature with waterfalls or woods should be used to entice their attention. | |||
==== Feedback 5 ==== | |||
Just like the other feedback interviews the overall impression of design 1 is considered positive and with real advantages in comparison with the current hoist. Just as stated in feedback 4, the motorized wheels and spherical wheels are very handy as turning will not be an issue anymore and less physical power of the caregiver is needed. This adjustment will reduce the workload of the patient and their back pain which is obtained by frequently using the hoist. The emergency button and the holder for the whalebones are considered equally as in feedback 3. The camera for navigation will also be of good use. Especially for managing the hoist under beds and chairs where cables or attributes like shoes can be avoided now and it is not necessary for the caregiver to get down on his knees anymore to see what is interfering with the hoist. Therefore the interface of the caregiver is well equipped especially with the window of the surrounding just in front of the hoist. Option three for the interface of the patient can be of good use for demented patients. A short film clip as mentioned in feedback 4 should be used or perhaps a little bit of music could be added to it. It is probably good that the caregiver is also visible on the interface of the patient as it is more comforting to see a matching face from the caregiver who is talking to the patient from behind the hoist. | |||
=== Conclusion feedback === | |||
From all the gathered feedback can be concluded that design 1 is indeed an improvement of the current passive patient hoist. The bigger motorized wheels are a very good adjustment to the current hoist. They reduce the workload of the caregiver to move the hoist and be doing so they can prevent back pain for the caregiver by frequently use of the hoist. However this motorized system including the force sensors (nr. 2 in design 1) should be tested very properly, because the motorized hoist and push load of the caregiver should be well adjusted to each other so no jerky reactions or collisions by too fast movements are obtained. In all the feedback interviews was stated that the spherical solid wheels are actually a must for the improved design of the hoist. They make it easier to turn the hoist in a desired direction and in combination with the motorized wheels they will make the lifting process a lot easier by reducing the workload of the caregiver so less physical power of the caregiver is needed. The position of the emergency stop in design 1 is more suitable than the lower current position on the hoist, because it is positioned in the working space of the caregiver. Especially when more electronics are implemented it is important that the hoist can be turned off right away. The camera for navigation is regarded as another good adjustment to the current design. Especially for managing the hoist underneath beds and chairs where cables and other attributes can be avoided. It is a fine implementation that can make spots visible for the caregiver and it can prevent collisions. It can be of good use in small busy rooms as well as for the transportation process. Although simple yet a very handy adjustment has proven to be the addition of a holder for the whalebones of the lifting mat as they are now in no way connected to the hoist and they are often lost. The interface of the caregiver can support the caregiver in his tasks. It improves the interaction between patient and caregiver by making eye contact possible form behind the hoist, it smoothens the process by giving feedback about a patient’s condition by use of the traffic light system and it provides information about the surroundings just in front of the hoist. The traffic light system extra alerts the caregiver which is therefore an advantage to provide good care, but questions arose whether the used software to detect facial emotions can be used for patients with facial paralysis or defacements and whether caregivers will not focus too much on the interface so the risk of collisions will increase while moving the hoist. Options one, three and four for the interface of the patient are useful adjustments and can either improve the interaction between caregiver and patient or comfort the patient more during the lifting process. Option three is a good option for comforting and distracting patients when both caregiver and short film clips about the nature are visible to entice their attention. Option two is not necessary, because not all patients will understand the given instructions. The caregiver provides these instructions himself verbally to the patient during the process. The control over these options which can be turned on or off should be given to both caregiver and patient, as long as the patient is capable to do so. | |||
Other adjustments like a peg for the lifting mat and another kind of control system for the hoist by using an IPad have been stated in the gathered feedback. These can perhaps be incorporated in a final or future design. | |||
== Final Design == | |||
Based on the gathered feedback about design 1, it can be concluded that most of the made adjustments on the current hoist are useful and should indeed be implemented in the new design. To create a final design of the passive patient hoist a few changes in design 1 will be made which will be explained further. | |||
An extra improvement which is stated in feedback interview 1 for design 1 is that a kind of peg should be adjusted on the hoist so the lifting mat, which is now just thrown over the hoist, can be hung up on. This adjustment is implemented in the final design as it is proven that the current manner at which the lifting mat is hung up is bad for the mat as it is easier worn out which reduces the safety of its use. | |||
Another addition to the design is a small light source next to camera for navigation (nr. 8 in design 1). This will improve the visibility of the environment of the camera as it has been stated in the feedback interviews that the legs of the hoist will be shoved underneath beds and chairs. | |||
Requirement d (“The hoist should be able to recognize anxiety in the patients”) is satisfied in design 1 by using facial expression recognition software of Noldus. However, the software cannot detect facial emotions by patients with facial paralysis or defacements. Therefore the previously proposed software of MIT in which emotions of persons are detected by taking respiration and heart beat into account will be implemented in the final design besides the software of Noldus. The output of the MIT software will also be connected to the traffic light system just like the output of the Noldus software so the caregiver can be alerted whenever the patient is feeling uncomfortable. This way more patients, even patients with facial paralysis or defacements can be taken into account for the improved design. | |||
To make the implemented traffic light system in the interface of the caregiver also functional for colorblind caregivers as stated in feedback interview 2, symbols inside the red, yellow and green light are used like in figure 10. These symbols will be visible whenever the red, yellow or green light shines. | |||
Due to the feedback about the interface of the patient the following changes are made for the final design of the hoist. Firstly, the second option for the interface of the patient in which the caregiver and a short film clip about the actions of the lifting process are explained is removed. This is done because not all patients will understand the given instructions and the caregiver prefers to give these instructions himself verbally to the patient during the process. Secondly, the third option for the interface of the caregiver in which the caregiver and an animation for distracting the patient is showed is adapted. This change consists of showing a different short film clip, like one about nature with waterfalls or woods to entice the attention of patients with for example dementia as these sort of films are more comforting for them. | |||
Finally the control over all options for the interface of the patient which can be turned on or off is given to both patient and caregiver. The patient can choose from the different options on his own interface (nr. 6 in design 1) and the caregiver from his interface (nr. 1 in design 1). Normally the patient will have full control over the given options, but whenever the patient is no longer capable of controlling these options, the caregiver will do it for him. | |||
All the above mentioned changes lead to the final design of the I.P.H. | |||
== Discussion == | |||
A design for an improved hoist was obtained. Although this design well-founded, there are also several limitations to the research done. Some of these problems can be solved in further research. | |||
First of all, it was not possible to interview patients and a limited amount of surveys were filled in by patients. This is due to the fact that patients who have experience with the hoist, are a very fragile group. Often they are old and have dementia. Most nursing homes would not let us ask questions to this patients, because that could upset them or they would not understand us anyway. Nurses could tell us a lot of what they thought to be the desires of the patients, but it would be better if the patients were asked themselves. Some of our solutions might have been rejected or patient could have had very specific problems with hoist the nurses did not know about. The improvements in our design are therefore mainly based on the view of nurses on the problems of patients. This can be different from the problems the patients experience themselves. | |||
Secondly, there were a couple of problems with the Noldus Facial expression recognition that was used. For instance, the version that was obtained did not have the possibility to export the data real-time. This meant that it was only possible to export and analyze the data at the end of recording. It was possible to see the data in the program itself real-time, but for using it for the interface of the nurse, it needed to be exported it to the script that was written, in real-time. The traffic light system that was designed could only work afterwards. This problem, however can be easily solved for anyone who would like to implement our design by obtaining the right software. | |||
Another problem that was encountered was that the software was not able to export the data on arousal, only on valence. The script for the lights of the traffic light could be more accurate with this data. At the moment it only uses valence, which means that every negative emotion can change the traffic light. Ideally the traffic light would only respond to fear, but for that data on arousal is needed. This problem could also be solved by obtaining the right software. | |||
Furthermore, an important limitation of the research is that the software was not tested on people who are partly paralyzed or have a disfiguration in the face. It is possible that the software does not work well on these kind of patients, which can lead to false signals towards the nurse. This problem can be solved however by measuring heart beat or respiration as mentioned in the requirements. The technology using radio frequency signals (see requirements) that MIT has invented can also work for this, but this technology is rather new and needs to be developed further, before it is possible to implement it in the hoist. | |||
== Conclusion == | |||
The goal of this project and the experiments was to improve the current passive patient hoist in ways that would result in more convenience for the primary users, thus for the caregiver and the patient. In literature hardly any research is found about the use of patients hoists in hospitals and nursing homes. | |||
Considering the fact that there has been little research done about the passive patient hoist, it was stimulating to start a new experiment in which the current hoist could be improved, whereby two main hypotheses were formulated: ‘Caregivers need to be supported by the patient hoist’ and ‘Patients and caregivers attach value to interaction during the process of lifting’. Based on the results of the interviews and the survey of the first hypothesis can be concluded that there is a need for care givers to be supported by cameras for navigating the patient hoist and that the caregiver would like to be warned by the hoist whenever the patient is feeling anxious. From the second hypothesis can be concluded that both caregivers and patients prefer eye contact more during the interaction than speech and physical contact. | |||
Based on the results of the interviews and the survey seven requirements to improve the current passive hoist were made and implemented in the first design. Two of these requirements, which are more elaborated in the experiment, are ‘During the whole process eye contact between the patient and the nurse is guaranteed’ and ‘The hoist should be able to recognize anxiety in the patients’. To satisfy these two requirements cameras are implemented in the first design and software of Noldus was used to test the facial expressions of the patient. Additionally a traffic light system is implemented on the interface of the caregiver which is connected to the camera of the patient. Due to the implemented software of Noldus it could recognize facial emotions of the patient. This traffic light system had been tested and works sufficiently. | |||
As the overall impression about the gathered feedback of design 1 is positive, it can be concluded that the implemented adjustments of design 1 are indeed an improvement of the current passive patient hoist. Due to this feedback some little adaptations have been done leading to the final design of the passive hoist. This all has resulted in the creation of two different end products, namely one new hoist design that consists of all adjustments, portrayed in figure 18, and another one that will function as an add-on for the current hoist, portrayed in figure 19. | |||
{| | |||
|- | |||
| [[File:DesignPassive.png|thumb|none|alt=ALT|600px|Figure 18: New hoist with the list of improvements implemented ]] | |||
| [[File:Add-on.png|thumb|none|alt=ALT|700px|Figure 19: Current hoist with the Add-on]] | |||
|} | |||
==Future research== | |||
Finally possibilities for future research will be examined. The most important follow-up research that needs to be done is research on the actual implementation of the improved hoist. It needs to be researched in what extent the design improves the comfort for the patient and nurse and the effectiveness of the nurse. This can be done by actually producing the hoist and testing it in a nursing home under standard circumstances. | |||
Furthermore, a lot of other aspects need to be taken into account before the design can be implemented. For this research, only the primary users were considered, but before implementation takes place it is important to look into the requirements for secondary and tertiary users, too. For instance, the costs of the design are still unclear just like the regulation concerning the improvements. These aspects are beyond the scope of this research, but it should be investigated in future research. | |||
The patients and nurses could also be more directly involved with the implementation. In further research it would be recommended to include the users in the research group. | |||
Lastly, in the proposed design the nurse is still present during the transfer. However the proposed design can be a stepping stone towards full automation, because some of the needed technology for full automation is already implemented in our design. Thus it can make the caregivers and nurses become more familiar with robotics. | |||
== References == | |||
<references /> | |||
== Appendix == | |||
== | === Planning === | ||
==== Short version planning ==== | |||
* Gathering information (week 1-3) | |||
1) '''Interviews (week 2-4)''' | |||
Making interview (week 2) (1h) | |||
Conducting interviews (week 3-4) (10h) | |||
Processing results interviews and conclusion (week 4) (4h) | |||
2) '''Surveys (week 2-4)''' | |||
Making survey (week2-3) ( | |||
https://docs.google.com/forms/d/e/1FAIpQLScinjbrL8rMoxs1CQOP0JCgIO3u_tavH2K1LGRcKIa9q_bFVA/viewform ) | |||
Conducting survey (week 3) (8h) | |||
Processing results survey and conclusion (week 4) (4h) | |||
3) '''Literature research (week 2-4)''' | |||
State-of the-art (9h) | |||
Human-Robot interaction (9h) | |||
Specific (...h) | |||
4) '''1st design (week 4-5)''' | |||
Design/sketch (perhaps 3D-model) (week 5-6) (4h) | |||
Description (week 5) (10h) | |||
5) '''Potentially prototype (week 5)''' | |||
Reading in(4h) | |||
Programming (7h) | |||
6) '''Feedback (autorative) (week 4-6) (6h)''' | |||
7) '''Potentially testing prototype (week 6) (10h)''' | |||
8) '''Final design (week 7) (5h)''' | |||
9) '''Wiki''' | |||
Week 2-6 (Every member 1 hour per week for adding and restoring information etc) | |||
Week 7 (each member 2 hours) | |||
==== [[ Extensive version planning ]] ==== | |||
=== [[ Weekly meetings ]] === | |||
Latest revision as of 22:41, 30 October 2016
Group members
Marissa Damink 0858700 (M)
Jochem Meijer 0899769 (JO)
Nicky Alexander 0886116 (N)
Jesse van Kempen 0907453 (JE)
Jasmijn Kleij 0906848 (JA)
Abstract
The goal of this project was to improve the current passive patient hoist by making adjustments to enhance the convenience for primary users. In literature hardly any research was found about the use of passive patients hoists in hospitals and nursing homes. The first step of this research was to gain information from the users of the hoist by taking interviews and conducting a survey. Based on the results of the interviews and the survey seven requirements to improve the current passive hoist were made and implemented in the first design. Due to the feedback some alternations of the first design have been executed which resulted in the final design of the patient hoist. This final design consists of two different end products, one new patient hoist design that consists of all adjustments and one which is functioning as an add-on for the current patient hoist.
Introduction
Our current society is facing the societal dilemma of ageing, given that the ratio of care takers and caregivers is out of balance and will be expanded even more in the future.
Technological advancements in health care are taking place, such as better treatment for diseases, and those also contribute to the increase of elderly people, because their lifespan is extended.
Due to this, there will be a lack of caregivers in the future and therefore it will almost be inevitable that robots are partially taking over tasks. These tasks cannot be of great complexity of course, as robots are unable to think autonomous like humans. From this point of view, we have come up with a good use for robotics in which the relatively few human caregivers left in the future can focus on important and risky care tasks which should not be given in the hands of robots, like for instance the use of robots in operating theatres.
Our idea will be realized by improving the current patient hoist in hospitals and nursing homes, in which patients who are not able to relocate themselves anymore, are transferred by lifting them. The patients can be transferred between for instance a bed and a chair or to places like restrooms and sitting rooms etc.
However, unlike already existing patient lifts, our improved patient hoist (I.P.H.) can work partially autonomous and will be equipped with an interaction device. Due to this, the new patient hoist is able to detect emotions of patients. The USE-centered design method will play a significant role in our design cycle so the I.P.H. can be beneficial for all sorts of groups.
Hypothesis
To guide the research several hypotheses have been set up. These are divided in main hypotheses with several sub-hypotheses. Some of these will be investigated through surveys and others will become clear from interviews.
Caregivers need to be supported by the patient hoist
- Caregivers need to be supported by cameras for navigating the patient hoist.
- Caregivers need a patient hoist that can navigate itself and avoid obstacles.
- The caregiver would like to be warned by the patient hoist whenever the patient is anxious.
- Patients appreciate it when they are reassured by the patient hoist whenever they are anxious.
- Caregivers need a patient hoist that can provide information about the weight or the 'BMI' of the patient.
Patients and caregivers attach value to interaction during the process of lifting.
- Patients need a certain level of interaction with the caregiver during the process of lifting. (So more need for touch/eye contact/speech, or no need?) (Survey)
- During the interaction between patient and caregiver eye contact is more important than speech for a pleasant interaction. (Survey)
- During the interaction between patient and caregiver eye contact is more important than physical contact for a pleasant interaction. (Survey)
- Patients do not mind if the caregiver is absent for a certain part of the lifting process.
Objectives and approach
The main objective of the project is to improve the current passive patient hoist. The passive instead of the active patient hoist is chosen, because a human-robot interaction adjustment can be of good use for this hoist. The interaction between patient and caregiver by using a passive hoist is not constant during the process as the distance between caregiver (behind the hoist) and patient (in the yoke of the hoist) is much larger than with an active hoist. To be able to determine the shortcomings and disadvantages of the current passive patient hoist it is important to get enough inside information. This information will be gathered by literature research, taking interviews and conducting a survey of the primary users of the hoist. After analysis of all this collected information the hypotheses stated above can either be confirmed or disconfirmed. The answers of the hypotheses are, next to the now known shortcomings and problems, used to set up requirements for the new design of the passive hoist. The new design will be sketched and a demonstration film will be made to illustrate/clarify the meanings of the made adjustments in the design. At the end feedback will be gathered to verify whether the adjustments in the new design are successful and a final design will be proposed by taking the feedback into account.
Scenarios
To give you all a proper view about the current use of the passive patient hoist, the current working method will be described in the next two scenarios:
Scenario 1: - Inside one room -
“Transporting from bed to chair inside a room with the passive patient hoist”
Mr. A is a 75 year old inhabitant of Parc Imstenrade, a home for the elderly. Mr. A, who cannot stand up by himself and therefore not able to relocate himself anymore, lies in his bed in room 23. Caregiver Lilly is going to put Mr. A in his chair near the window so he can see the nearby public garden. She will use the passive patient hoist to do so.
Lilly takes a lifting mat of the proper size for Mr. A and puts 2 whalebones in the backside of the lifting mat for better support for Mr. A’s back during the lifting process. She brings the bed to the right working height so she can work more easily without risking back problems. Lilly explains to Mr. A. what she is doing and is going to do at every step of the lifting process so he will not be surprised by any actions. First she turns Mr. A to his left side and pushes the lifting mat underneath him. Then she turns him to his right side so the mat can be equally divided underneath him. As soon as Mr. A lies back on his back again, Lilly lowers the bed, because the working height is too high for the patient hoist to lift Mr. A from his bed. Now the bed is at proper height and Mr. A lies correctly in the lifting mat, the patient hoist is called over. Lilly pushes the legs of the hoist beneath Mr. A.’s bed and guides the yoke of the hoist to the right position above Mr. A. By using the remote control of the hoist Lilly lowers the yoke so it can be attached to the lifting mat. The yoke is attached between Mr. A.’s legs and along both sides at shoulder height to the mat. The arms of Mr. A will stay inside the yoke and the mat during the lifting process. Once the mat is well attached to the yoke, Lilly lifts the yoke by using the remote control again. During the lifting Mr. A. is brought from a lying position to a sitting position in the mat. This is not very comfortable for Mr. A. because the lifting mat cuts a little bit between his legs. Once free from the bed, Lilly can move the patient hoist with Mr. A. towards his chair near the window. Note that this is not an easy task for her, because she has to push hard enough to get the hoist into motion, mind the environment of the hoist to prevent bumping up against things and hold one hand at the yoke so it will not shake too much, so Mr. A. will not get motion sick or scared due to the trembling. As they arrive at the chair, Lilly brings the hoist to the right position in front of the chair and moves the legs of the hoist from each other with the remote control so the hoist can be placed around the chair. She places the yoke with Mr. A .inside exactly above his chair so his back and the back of the chair are exactly in the same position. When chair and yoke are in the right position Lilly presses the remote control again to lower the yoke. Mr. A. is then gently lowered into his chair with the lifting mat underneath him. Once Mr. A. sits in his chair the yoke is released from the mat and the hoist is slowly driven away from the chair by Lilly while preventing a collision between the yoke and Mr. A. The whalebones in the backside of the lifting mat are removed, because they are not comfortable for Mr. A.’s back while sitting. Lilly asks Mr. A. whether he wants the lifting mat to stay underneath him or not. He does not want it underneath him, therefore Lilly pulls the mat from between his legs to the outside of his hips towards his back to remove it underneath him. Now Mr. A. can enjoy his sightseeing.
Scenario 2: - Transportation -
“Transporting from bed to general living room with the passive patient hoist”
It is morning in ‘De Tulp’, a home for the elderly and the 70 year old Mrs. B. who suffers from paraplegia lies in bed. She is ready for nurse Jane to transport her to the general living room where she can sit next to her close friend Mrs. C. to gossip about the cute Mr. D of next door. Due to her illness Mrs. B. is not able to replace herself anymore so she will be transferred from her bed to the chair in de living room next to Mrs. C. by the passive patient hoist. Nurse Jane will use the same method as caregiver Lilly to bring Mrs. B. from her bed in the yoke as was done with Mr. A. in scenario 1. When this is done and Mrs. B. hangs above her bed in the yoke, Jane will drive the hoist out of Mrs. B.’s room over the corridor to the living room. Just like Lilly, Jane will explain what she is doing to Mrs. B. during the lifting and transfer process so Mrs. B. will be at ease and not surprised by any actions during her transfer. Jane will need to coordinate the whole process very carefully, because she needs to exert enough force to push the patient hoist. She has to take into account the surroundings of the hoist to prevent accidents during the transfer. She also frequently has to keep the yoke steady with one hand during the process so Mrs. A will not get motion sick or scared due to the trembling of the yoke. Before the transportation process of Mrs. B. with the hoist really can start Jane has to turn the yoke with Mrs. B. inside manually into the right direction. Due to this Mrs. B.’s face points forward, while the hoist and Jane are behind her. Mrs. B. is now able to see in what direction she is pushed by Jane. Jane can now start the transportation by pushing the hoist towards the room door. At the door Jane needs to be extra careful and make sure that she does not bump into something. This is necessary, because her sight about what is happening directly outside the door is not sufficient enough. She also needs to push the hoist with more power to drive over the little threshold. Once outside Mrs. B.’s room, Jane needs to focus again extra carefully to provide Mrs. B. a safe ride and to prevent any collisions with other humans or items in the hallway. Keep in mind that Jane and Mrs. B. cannot make any eye contact during the transportation process so Jane has to observe very attentively (as far as possible) whether something is going wrong with Mrs. B. The use of speaking is now the only solution for any interaction between them. Once arrived at the door of the living room, the threshold situation repeats itself and precise coordination of Jane is required. Jane puts Mrs. B. in the chair next to Mrs. C. by using the remote control to open the legs of the hoist and to lower the yoke just like was done to put Mr. A. in his chair in scenario 1. Mrs. B. en Mrs. C. can now finally continue their discussion about Mr. D.
Literature study
State-of-the-art
A patient hoist is a mechanical device for lifting a patient out of bed into a (wheel)chair. There are two kinds of hoists, the active and the passive one. The active hoist is meant for patients who still can stand up, but cannot move very well. It lifts the patient from a bed to a standing-up position on the hoist, after which the patient can be moved to a chair. The passive hoist is used for patients who are too weak to stay standing up. It moves the patient in a sitting position.[1]
Most passive hoists consist of a frame with a sling attached to it. The patient gets secured in the sling by the nurse and the hoist lifts the patient upwards. Next the hoist can be moved by the nurse towards the bed or chair and afterwards the hoist lowers the patient onto the bed or chair. Finally, the nurse releases the patient from the sling. There are lots of different models for passive hoists. Most hoists move the patient along a vertical axis, after which the whole device can be moved by the nurse. Some work with a rail which can transport the patient over a horizontal axis, after the patient has been lifted up. These rails can be integrated into the room, or can be moved from bed to bed. An active hoist does not move the patient from a lying position to a sitting position like the passive lift, but moves the patient from a sitting to a standing position. It can be used to transport the patient, but sometimes the active hoist is only used to help the patient to stand after which he/she can walk by him/herself, possibly with the help of a caregiver. This helps patients to maintain their mobility.[2]
A lot of research has been done about the use of patient hoists in hospitals and nursing homes. Johnsson et al. (2004)[3] proposed a model that simulated the balance between the nurse and the patient during a transfer task. The movement between the patient and the nurse should be harmonious, otherwise it may cause injuries. Research has proven that a lot of difficulties exist with the current patient hoists. Even when a hoist is available nurses do not always use it. Several reasons are: “(..) lack of time and availability, difficulty of use, space constraints, and patient preferences.”.[4] By including the nurses in the buying process and buying a powered lift instead of a mechanical one, a nursing home can improve the chance of the hoist actually being used. Furthermore a hoist cannot decrease the risk coming with lifting, but it can still reduce it significantly.[4] Despite several researches it is not clear what patients prefer. Some studies show that patients prefer a mechanical hoist, while other studies concluded that patients were more comfortable with a ceiling lift.[3]
There have been several attempts to improve the passive hoists with help of robotics. One of the earliest attempts was in the period 1990-1992 in a study of Patrick A. Finlay.[5] In this study it was recognized that several specification were needed. First the robot should be able to move the patient without causing injuries. Of course, every patient is different and especially patients that have to be moved with the hoist can have numerous of physical problems the robot has to take into account. The robot should also be able to collect the patient from a lot of different positions and move them to lots of other possible positions. Third, the robot should be able to move through a hospital without accidents. Finally, the robot should not work too slow, because nurses and patients otherwise find the waiting time not worth to use the robot. The decision was made to make it a nurse controlled device, to get the patients and nurses to slowly get used to it. A initial design for the robot, which was called the Patient Assistant for Mobility (PAM) was already made up: “The patient surface of PAM is made up of an array of slats or tines which, using a patented method of deployment, are able to be insinuated gently under the patient to support his/her weight and draw him/her onto the trolley surface. The patient surface has a Z-axis to adjust its height, is additionally articulated at the hip and knee joints, and can thus move to set the patient into a seated or other intermediate pose. (…) Sensors are used to monitor the stability of the platform, and as a useful by-product these are processed to provide a readout of patient weight. For patients with special nursing needs, selected tines can be disabled so that no contact is made with the corresponding part of the body. The patient surface has an autonomous acquisition capability, so that a single command enables a patient to be collected from a bed once the PAM is parked in approximately the correct orientation at the bedside. Articulation of the patient surface is normally in telemanipulator mode, but the PAM also contains a memory enabling details of patients and furniture to be stored, so that a collection and placement sequence can be played back whenever required.”[5]
Although this project started the demonstrator phase in 1992, it is unclear what happened with PAM after that.
Another attempt to improve the patient hoist was in 2007, in a project led by Lakshitha Dantanarayana.[6] In this project the author developed a smart hoist in collaboration with the resident and carers of the residential care facility. Some adaptions they found to be useful were weight measurement, rear view mirrors, ability to monitor the environment and assisted manoeuvering. The researchers equipped a standard patient hoist with cameras in the front, just above the floor to provide information about the part of the environment that is blocked from view by the hanging patient and implemented strain gauges into the design to measure the weight of patients. Other improvements were cameras to monitor the environment behind the carers and robotic wheels. The patient hoist also had a navigation assistance algorithm implemented. The main change however was that the patient hoist was motor driven, but still moved by applying forces to the handles. The force was measured by the hoist and a similar movement was applied by the motors. This ensured the hoist could be used intuitively, and the learning curve was short. Several users trials were executed, and the researchers implemented the feedback in the final design. There was no clear conclusion whether the smart hoist was better than the traditional hoist, but several points for improvement were found.
Besides the hoist other solutions for lifting patients are researched, like the HAL exoskeleton and the Japanese lifting robot RIBA, but those projects are beyond the scope of our research.
USE-aspects
This subject is in many ways related to USE-aspects. First of all there are many different stakeholders and users. The primary users are of course the patients and the nurses. The secondary users are the people who pay the hoist, in this case the hospital management and the government and the tertiary users are the maintenance people. The preferences of all these users have to be taken into account. For instance, the patients want the hoist to be comfortable, while the nurses want it to be easy to use. The hospital management wants the hoist to be made as cheap as possible and the maintenance people prefer that the important components are easy to repair or to replace. This can lead to conflicts since it can be difficult to take all these preferences into account at the same time. The focus of this project is therefore mainly on the preferences of the primary users. The main question is how the hoist can be improved so that it is less uncomfortable for both patient and nurse. An important aspect that will be taken into account in this research is the interaction between patient, hoist and nurse. The patients are a vulnerable group and being transferred with a hoist can be terrifying. The process however can also be bothersome for the caregiver. So important questions are: 'How does a patient want to be comforted?', 'Does this differ between different groups of patients?' and 'What does the nurse want?'. These are the kind of questions that will be answered in the research. The hoist however is not only a technical problem. A lot of these problems are actually more related to social or use aspects.
Research
Interviews
Interview questions
Before the interviews were taken a list with questions was made to ask about the desired information which could be obtained from the nurses and patients. After that several interviews were taken and the list was adapted a little (version 2) to answer new questions that had arisen during the research.
Questions for caregiver and patient
Collected interviews
In total five interviews were taken. All of them were with nurses who had experience with the passive patient hoist. Unfortunately no interviews with patients have been taken as this group was unapproachable.
The first two interviews were taken with Petra and Lianne, both nurses from Buurtzorg, which is a private care institution. Another two interviews were taken with Linda and Rachelle, both interns in their last year of their nurse education. The last interview was taken with Lisan who works in a nursing home with patients who suffer from dementia.
A link for the full versions of the collected interviews: Collected interviews
Results of interviews
Several problems emerged from the interviews. Here the most important points that were made clear in the interviews are summarized per interview.
Interview 1
This interview states that interaction between patient and caregiver is very important to establish good collaboration and trust between them. Everybody should feel safe and comfortable while using the passive patient hoist. Whenever the patient feels scared or not secure a good explanation about the taken actions should be provided, so trust and feeling safe can be created within the patient. Therefore it is a good idea to implement a device that can recognize emotions of the patient to assist the caregiver at his work. The hoist is not always experienced suitable for both patient and caregiver. The patient often dislikes for example the lifting mat, because it can cut in the patient’s legs. The caregiver on the other hand finds it difficult to move the hoist over a unsmooth floor or in small rooms. Further, the caregiver does not stand very close to the patient while operating the hoist.
Interview 2
From this interview can be concluded that the use of the passive patient hoist is an improvement in comparison with lifting of patients manually by the caregiver in which for example back pain can be reduced or prevented. However the hoist is not perfect and consists flaws. Maneuverability of the hoist has proven to be a main issue. When working with demented patients interaction between them and caregiver is a bit different than with not demented patients. Direct commands and explanation about the taken actions are given to the demented patients to reassure them, but sometimes an explanation has no use for them, because they do not understand it. Therefore they are sometimes distracted with a stuffed animal to smoothen the lifting process. At the same time these patients do not always express whether they are feeling uncomfortable or scared. Caregivers try to make something out/read the facial gesticulation of the patients to estimate how they are feeling. A device that could determine their emotions and one that could distract or reassure them during the process would be of good use.
Interview 3
This interview shows that using the passive patient hoist is not an easy task in nursing homes. In these homes are often small doorsteps present which makes it difficult for the caregiver to drive over. During the transport process the visibility for the caregiver is deficient due to the post of the hoist. To prevent this limited view the caregiver walks alongside the hoist. However, this is also not very convenient, because it makes it more difficult to push the hoist with sufficient power. A device that improves this navigation process is reflected as a good idea. Another practical aspect is the lifting mat. This mat is not very pleasant for patients, because it sometimes cuts in the legs of the patient during the lifting process. Further, during the process these mats are provided with whalebones at the backside for extra support for the patient. This whalebones need to be inserted before the process starts and removed by the caregiver whenever the patient sits, because it is not comfortable for the backbone while sitting. A big issue with these whalebones is that they get lost very easily, because they do not have a fixed place at the hoist. During the lifting process interaction is again important. Whenever a patient feels uncomfortable he is asked what is wrong and all actions are explained extensively. It depends on the patient, whether they are comfortable with more interaction or less.
Interview 4
Social interaction between patient and caregiver remains a crucial element during the lifting process. A lot of eye contact is made between them and they converse during the process. Whenever a patient is not acquainted with the hoist or if the patient is scared the caregiver will communicate more and try to make more eye contact as well to reassure the patient. When the patient is familiar with the hoist less interaction between him and the caregiver is needed to put the patient at ease. A technical aspect of the hoist is that the battery is heavy and it’s lifespan is very short. Another hoist like the ceiling hoist would be more suitable in smaller rooms and steering is much easier. However it is not a practical solution for existing care homes, because rails need to be constructed all over the nursing home.
Interview 5
The main point that can be concluded from this interview is that interaction is an important, but also a difficult point. Especially since the patients are suffering from dementia they do not really understand what you are saying. Still it is important to keep communicating about what you are doing and to comfort the patient. This is also possible by touching the patient, by eye contact or by distracting them with a stuffed animal. Over time you learn to recognize whether the patient is uncomfortable, because you get to know them. It is very important for nurses to get to know their patients. The main problems with the hoist are that you have to do several things at the same time and it is heavy to turn and move the hoist when it is loaded with a patient. It is especially difficult to navigate the hoist safely through small spaces while watching the patient.
Survey
Design of survey
Hypotheses:
- - Both patients and caregivers prefer eye contact most in the process of caregiving during transportation in the hoist.
- - Patients like to be comforted by voice interaction between patient and caregiver or between patient and someone else during the process of caregiving during transportation in the hoist.
- - Patients like to be comforted by physical contact in the process of caregiving during transportation in the hoist and also caregivers prefer to have some extent of body contact during care giving.
Design of the survey
Link to survey: https://docs.google.com/forms/d/e/1FAIpQLScinjbrL8rMoxs1CQOP0JCgIO3u_tavH2K1LGRcKIa9q_bFVA/viewform
Method
The code in Stata can be found by this link: Stata code.
In the previous week (week 3) some data for the survey was already gathered and a power analysis was conducted. Since the standard deviation at that moment was around 0.7, this value is used for the power analysis, together with a power of 0.8 and an alpha level of 0.05.
This showed that 24 to 32 respondents are needed to be able to see a significant result in the data. A mean difference of 0.5 points difference on the Likert-scale is used. The Likert-scale is the scale of 0 to 5 that was used in the survey.
Then data was collected again, especially of patients, because there was not enough data of this group. A sample size of 29 participants for each group was gathered.
The data was prepared for analysis, for example by giving proper names to the variables i.e. After that, the new standard deviation is determined.
The following hypotheses were analyzed.
- - What way of interaction receives most preference?
- - H0: There is no difference in the need for interaction between patients and caregivers
- - H0: There is no difference in preference for eye contact between patients and caregivers
- - H0: There is no difference in preference for voice interaction between patients and caregivers
- - H0: There is no difference in preference for body contact between patients and caregivers
Results
Using the new standard deviation (again 0.7), the sample size (29 participants per group) and again an alpha level of 0.05, the power is calculated. The value of the power is 0.76, this value is all right. In an ideal case 5 to 10 more patient participants should have been collected, but the analysis is continued anyway as the power has proven to be good enough.
Code: power twomeans 2 2.5, sd(0.7) n(58) alpha(0.05) //to compute power with given sample size -> 29 participants per group
The results, shown in figure 1, are:
Total mean for eye contact is 2.21, for voice interaction 2.24 and for body contact/interaction 2.75. The difference between patient and caregiver in eye contact is 0.05, for voice interaction it is around 0.5 and for physical contact it is 0.75.
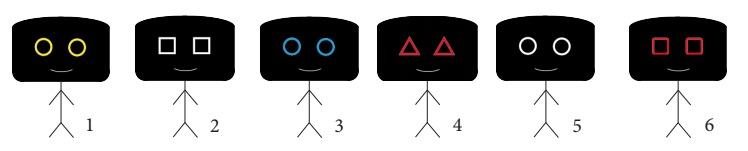 Figure 2: T-test of interaction
Figure 2: T-test of interaction
For the t-test of interaction by role of patient of caregiver, the t-value is 2.49 (fig. 2). There are 37 degrees of freedom and the p-value is 0.009.
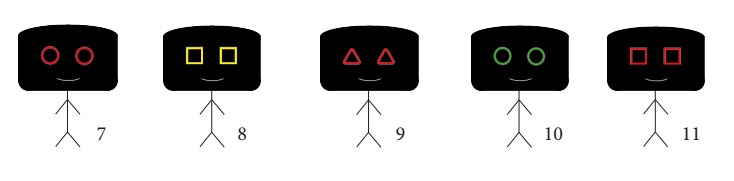 Figure 3: T-test of eye contact
Figure 3: T-test of eye contact
For the t-test of eye contact by role of patient of caregiver, the t-value is 0.17 and there are 37 degrees of freedom (fig. 3).
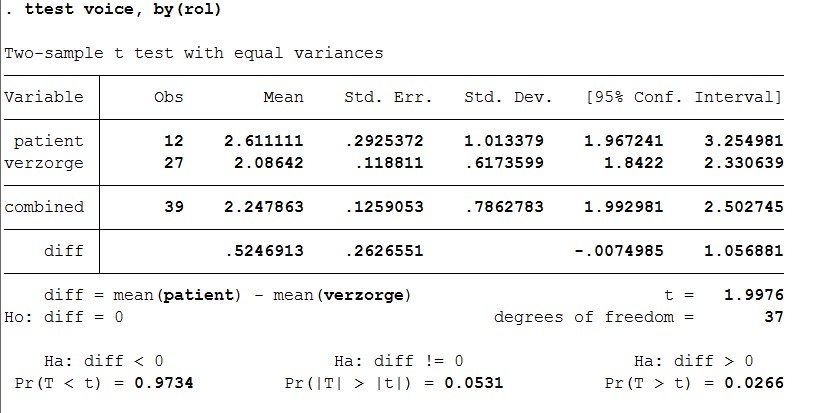 Figure 4: T-test of voice interaction
Figure 4: T-test of voice interaction
For the t-test of voice interaction by role of patient of caregiver, the t-value is 2.0 (fig. 4). There are 37 degrees of freedom and the p-value is 0.027.
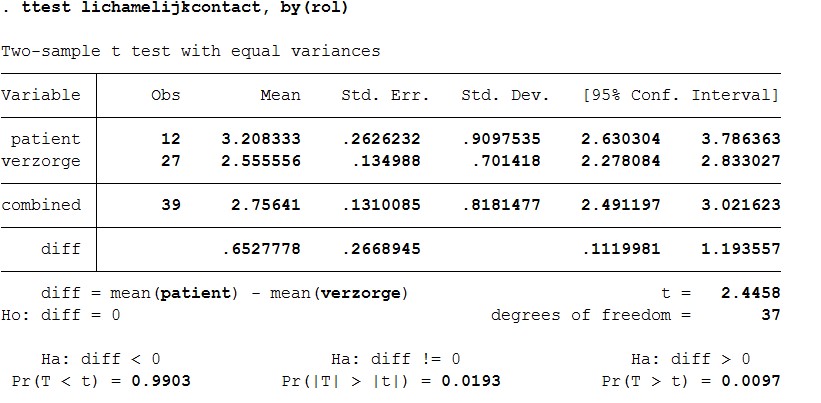 Figure 5: T-test of physical contact
Figure 5: T-test of physical contact
For the t-test of physical contact by role of patient of caregiver, the t-value is 2.45 (fig. 5). There are 37 degrees of freedom and the p-value is 0.01.
Discussion and conclusion of survey
The results mean:
What way of interaction receives most preference?
- Command: tabstat oog voice lichamelijkcontact, by(rol)
Eye contact receives most preference. With body contact you see that patients do not really like it. The value of preference is higher, which means their preference is lower. Also, the difference with preference of body contact between patients and caregivers is quite high.
What also turns out is that the preference for voice interaction is a little less for patients than for caregivers. This means that caregivers like talking to their patients more than patients prefer to talk to their caregivers. This is not what was hypothesized so further research will be done by using interviews and a t-test on voice interaction.
H0: There is no difference in the need for interaction between patients and caregivers
- Command: t-test interactie, by(rol)
There is a significant result, which means the preference for interaction between patients and caregivers is not the same. The p-value is significant, so H0 is rejected.
H0: There is no difference in preference for eye contact between patients and caregivers.
- Command: t-test oog, by(rol)
A t-test is conducted where the preference for eye contact is compared between patients and caregivers. There is no significant result because the p-value is not significant. This means that H0 cannot be rejected, so there is no difference in preference for eye contact between patients and caregivers.
H0: There is no difference in preference for voice interaction between patients and caregivers
- Command: t-test voice, by(rol)
A t-test is conducted where the resulting p-value is 0.03. This value is below 0.05 which means that H0 can be rejected, so there actually is a significant difference in preference for voice interaction between patients and caregivers. However, this resulting p-value is not very far below 0.05, therefore it is not completely sure whether this difference is significant.
H0: There is no difference in preference for body contact between patients and caregivers
- Command: t-test lichamelijkcontact, by(rol)
This final t-test shows a large significant result, a significant p-value. This means H0 can be rejected and there is a difference in preference for body contact between patients and caregivers. Patients prefer this way less than caregivers.
Noldus company for face detection software is contacted for a free trial software. Via telephonic contact Noldus promised to send this trial version as soon as possible.
Analysis
From both the survey and the interviews several things can be concluded. First a answer the question whether our hypotheses were true or not will be provided.
Caregivers need to be supported by the patient hoist
From the interviews can be concluded that caregivers do not really need to be supported by the patient hoist, they can manage without, but it could help much. Nurses have indicated that especially a hoist that helps with navigating through small spaces would be of great help. Thus the hypothesis that nurses would need to be supported by cameras for navigating can be confirmed. It is less clear whether the second sub-hypothesis, “Caregivers need a patient hoist that can navigate itself and avoid obstacles” can be confirmed. Nurses have mentioned that they would like to have help with navigating, but none of them mentioned they would like the hoist to move by itself. At least one of them, Lisan, has mentioned an aversion for a self-moving hoist. She was convinced a nurse should always be present. So it can be concluded that this sub-hypothesis is untrue. Not much consensus was found on the third sub-hypothesis: “The caregiver would like to be warned by the patient hoist whenever the patient is anxious”. Some nurses mentioned that it could be handy, but other nurses mentioned that this is the task of the caregiver and by getting to know the patient a caregiver could identify by herself whether the patient was anxious. So this hypothesis can neither be confirmed nor rejected. The fourth sub-hypothesis “Patients appreciate it when they are reassured by the patient hoist whenever they are anxious” can also neither be confirmed nor rejected, because it was not possible to interview a patient. As patients a very vulnerable group, the nurses did not want them to be interviewed. The last sub-hypothesis was: ”Caregivers need a patient hoist that can provide information about the weight or the 'BMI' of the patient”. One nurse mentioned it would not be necessary, because they weigh the patient already once a month. However, the other nurses never gave a clear answer to this question and therefore it can neither be confirmed nor rejected.
Patients and caregivers attach value to interaction during the process of lifting.
This hypothesis was examined by a survey. From this survey and the interviews can be concluded that most patients and caregivers do indeed attach much value to interaction during the lifting process. In the interviews it was mentioned as one the most important aspects of the tilling process. From the survey can be concluded that both patients and caregivers prefer eye contact most during the process of caregiving. This is also what was hypothesized. Results of the survey show also that both caregivers and patients like to have voice interaction to some extent. However, the preference for voice interaction is significantly larger for caregivers than for patients. Patients do prefer voice interaction, but to a much lesser extent than caregivers do, and also to a much lesser extent than was hypothesized. For body contact there is a large significant difference in preference for caregivers and patients. Patients actually dislike body contact during the process which was not hypothesized. From these results it can be concluded that eye contact is the most important factor of interaction during caregiving. This will be used to optimize interaction in the process of caregiving during transportation in the patient hoist. Voice interaction is less important for patients, but this can also be taken into consideration in the design for optimizing the patient hoist.
Problems
As the hypotheses are now answered, the main problems of the current design can be identified and requirements that the improved design must meet can be proposed.
A lot of nurses have mentioned that they have trouble with moving the hoist. A lot of these problems were caused by wheels that got stuck. The swivel caster wheels, which are currently used, do not roll as smoothly as hoped. This is caused by a rough surface or the orientation of the wheels. Therefore the first requirement for the new design is that wheels are used that do not get stuck.
Another problem that many nurses encountered was that the hoist was heavy to push when loaded with a patient. It was also very difficult to turn the patient or the arm of the hoist when also focusing on the wellbeing of the patient. That is why the following two requirements were set up: Less force should be needed to push the hoist and less force should be needed to move or turn the patient when loaded in the hoist.
From the hypotheses can also be concluded that nurses do have trouble with moving the hoist around in small spaces and would like some assistance with that. It is difficult for the nurse to keep an eye on everything, mainly because the patient is blocking a significant part of the field of sight of the nurse. This leads to the fourth requirement: The hoist should give a better overview to the nurse during the transfer.
A conclusion that was drawn from the survey was that patient and nurses value eye contact during the transfer for a great deal. However, on longer distances where the patient is facing towards the moving direction of the hoist there is no eye contact at all. This can lead to a less comfortable experience for the patient, that is why another requirement holds that during the whole process eye contact between the patient and the nurse is guaranteed.
Another problem that was examined was whether the nurses would like assistance with recognizing whenever the patient is uncomfortable. Although some mentioned that a nurse would learn this by time, for inexperienced nurses recognizing anxiety can be a challenge, because the patients are not always able to express their feelings. That is why it is likely that the following requirement still can be an improvement to the hoist: The hoist should be able to recognize anxiety in the patients.
The last requirement is: The hoist should be able to comfort the patient. It was not possible to examine whether the patients would like this, but especially since the design could be a bridge between the current lift and full automated one, it is likely that it can add something important to the hoist.
Requirements
In this section the best solutions for the earlier stated requirements will be discussed.
Requirement a: During the whole process eye contact between the patient and the nurse is guaranteed.
One way to realize this is by the use of cameras and displays. A patient, who is sitting in the lift, can be filmed by a camera. This images are transferred to a display that is attached to the back of the lift where the nurse is standing, who is also filmed. The patient also should have a display in sight, so eye contact can be established at all time. However, when you look at a screen, you do not look in the camera. This is because they are at two different places. For this reason, eye contact via videos is difficult. However, there has been a lot of research on improving video-mediated communication. As stated in “eye contact and video-mediated communication: a review”[7] video-conferencing has become a popular video technology because it improves real-time communication. Video-conferencing is a richer form of communication than email or telephone, however, the authors says that video-conferencing is not quite as informative as face-to-face communication. Some research was done about ways to improve video-conferencing and eye contact during the use of webcams. Franc Solina and Robert Ravnik proposed a method related to the mona lisa effect.[8] This method establishes eye contact during video calling and it used big screens and cameras mounted above the screen.[9] However, a still better method must be possible. Stereo matching method, shown in figure 6, is a method that could solve our problem. With stereo matching a color image is used in a stereo camera as an input. This is configured by two cameras, they create a reference point.[10] However there is a problem with stereo matching, since most of the stereo matching methods only consider paired images in specific orders. To treat video images of stereo matching as a static image causes flickerings.[11]
Figure 6: Stereo matching method
Recently, a patent for “Method and apparatus for providing eye contact function to multiple points of attendance using stereo image in video conference system” has been proposed.[10] The patent presents an invention to improve eye contact. It improves eye contact images between remote attendances during video calling. Since this invention is not on the market yet, this will not be included in the demo, but for future use this aspect is very important. This method uses the same ideas as stereo matching, two cameras are used. However in advance to that, a depth image camera is also used, this is to calculate the occlusion region. With this information, an object mask for an image is created. The completed object mask is the way in which eye contact can be improved. Figure 7 shows an illustration of this.
Figure 7: Object mask
Requirement b: Less force should be needed to move or turn the patient when loaded in the hoist.
The patient loaded in the hoist should be easy to turn. In the interviews was mentioned that some nurses had trouble with turning the hoist in the right direction, while also making sure the hoist does not bump into something. The patient is turned by hand, which means all the applied force comes from the nurse. This could be made easier by also using an electromotor to turn the harness to which the sling is attached. For this user intention recognition will also be used, for the same reasons as mentioned above. To recognize the intention of the nurse the hoist needs a force control system. Usually force control is used in robots that have to pick up objects. It makes sure the robot does not squeeze anything. It does this by measuring the opposing force the object applies to the robot when the robot picks up the object. A feedback loop is used to ensure the robot responds in the correct way to the opposing force. This force control can be implemented in the hoist, so that the bigger force the nurse applies, the longer the robot continues this movement. To measure this force, force or strain sensors have to be implemented on every joint of the hoist. A computer measures this force and with the implemented logic determines the motion and velocities. Major motion patterns have to be identified and implemented in this computer, to ensure the hoist continues its movement in the same direction as the nurse applied the force in.
Requirement c: Less force should be needed to push the hoist.
The nurses mentioned in the interviews that they had trouble moving the hoist around in the rooms, because it was so heavy, especially when the patient was sitting inside the yoke. Sometimes the floors made it even more difficult to push the hoist forward. So it can be concluded that the improved hoist should have the ability to move without the nurse applying all the force. This is especially important when the hoist is used for larger distances, like moving the patient to the toilet or to another room. Our solution is to build in an electromotor to drive the wheels. This means the hoist requires a stronger battery. It was decided to not use a remote to steer the improved hoist, because that would add extra complexity to the hoist. The nurses would have to learn yet another thing. The learning curve needs to be kept short, so user intention recognition will be used to steer the hoist. This means the hoist anticipates on the intentions of the nurse by measuring how force is applied. For the nurse it means she can use the hoist the same way she was used to. More explanation of this can be found in requirement b.
Requirement d: The hoist should be able to recognize anxiety in the patients.
There are several ways a machine can recognize emotion in humans. One of the most obvious ways is of course the same as most humans do it, by reading a person's face. Software that is able do this already exists and is called facial expression recognition software. Reading the face by looking at the position of, for instance, the mouth and the eyes has proven to not work well enough, because every person is different. That is why these software analyze the relationship between points on the face. When somebody curls the corners of his/her mouth, the software registers that the point of the corner of the mounts moves. With a complex algorithm it concludes that the person expresses, to a certain amount, happiness. It is even possible for these software to recognize micro-expressions. Most of these software show the extent to which a person shows one of the seven basic emotions in percentages. The seven basic emotions these software uses are: joy, sadness, anger, fear, surprise, contempt, and disgust. Often a Neutral emotion is also added to the possible emotions. More complex emotions are always regarded as a combination of these seven emotions [12]. It is therefore more difficult to recognize these emotions in the numbers the software generates. However, since the software only has to recognize fear, it could be accurate enough for the goal of this research. Of course there are also other ways to recognize a person's emotions. Other aspects researches often take into account are respiration and heart beating. MIT[13] has written a paper about a new technology that can detect the emotion of a person by analyzing reflecting radio frequency signals of a body, which means that no sensors need to be applied. The EQ-radio sends a RF signal through the room, recognizes the person from the other objects, analyzes its reflections and recognizes his emotional state. This all is done by a new underlying algorithm that extracts individual heartbeats from the wireless signal. The accuracy of the emotion recognition is comparable with state-of-the-art emotion recognition systems that need a person to be hooked to an ECG monitor. For the design the facial expression recognition software will be used. The main reason for this is that this technology is already more developed and many different software are available. This makes it easy to implement in the design. The only things needed for this are software, cameras and a computer. Since the computer is also needed for other aspects of our design a computer will be implemented anyway. The camera is also already implemented for making eye-contact with the nurse. It is decided to go with the facial expression recognition software of Noldus. After contacting them a trial version of their software was obtained.
Requirement e: The hoist should be able to comfort the patient.
It was already stated the hoist should be able to recognize fear in the patient, but the hoist should also be able to react on it. It was already mentioned that a screen is attached to the hoist on which the patient can keep contact with the nurse, when the patient is moved. This screen can also be used to comfort the patient. One thing that was concluded from the interview is that it is important to tell the patient what is happening to him. So a feature is implemented in the hoist that can tell, either with spoken words or written on the screen, what is happening to the patient at the moment he/she is scared. The nurse should be able to turn this feature on and off at any moment. Another thing that was learned from the interviews is that a lot of patients who have to be transported by a hoist have dementia. They do not understand what the nurse is saying to them. Therefore they will not understand the hoist either when words are spoken or written on the screen to explain the taken actions. An option for them could be, that the screen on the hoist shows an animation which can distract the patient. This should also be a feature that the nurses should be able to turn on and off at any moment.
Requirement f: The hoist should give a better overview to the nurse during the transfer.
This problem can be solved by the use of a camera, which is placed at the front of the lift and films in the moving direction of the lift. Transferring these images to the display of the nurse, he/she can easily see what is in front of the lift and if there are any obstacles that could be possibly dangerous. Another addition would be sensors that indicate how close the lift is to a certain object, for instance a wall, so the nurse has an even more complete overview. These sensors, often used in cars for parking assistance, use super sound to determine the distance between the sensor and an object. If a minimum distance is exceeded the nurse will get a signal on het screen and the hoist will break automatically to prevent collision. However, since this partly takes away the control the nurse has, it was decided to go with the cameras. Maybe in the future when nurses and patients are more familiar with automation and robot technology, parking sensors could still be implemented.
Requirement g: Wheels that do not get stuck are used.
A solution for this is to use solid spherical wheels, which are part of a ball bearing. Since these wheels can move freely in every direction they will not get stuck due to orientation and can as well move over surfaces which are rough. Since these wheels do not have an axis around which they turn, it is difficult to support them with an electromotor. Therefore these wheels are mainly useful as replacement for the front wheels of the patient hoist.
Finally, in the interviews it was mentioned that the whalebones get lost easily. That is why a small adjustment will be added, besides the requirements. A pocket to the hoist to store the whalebones in will be attached.
Design 1
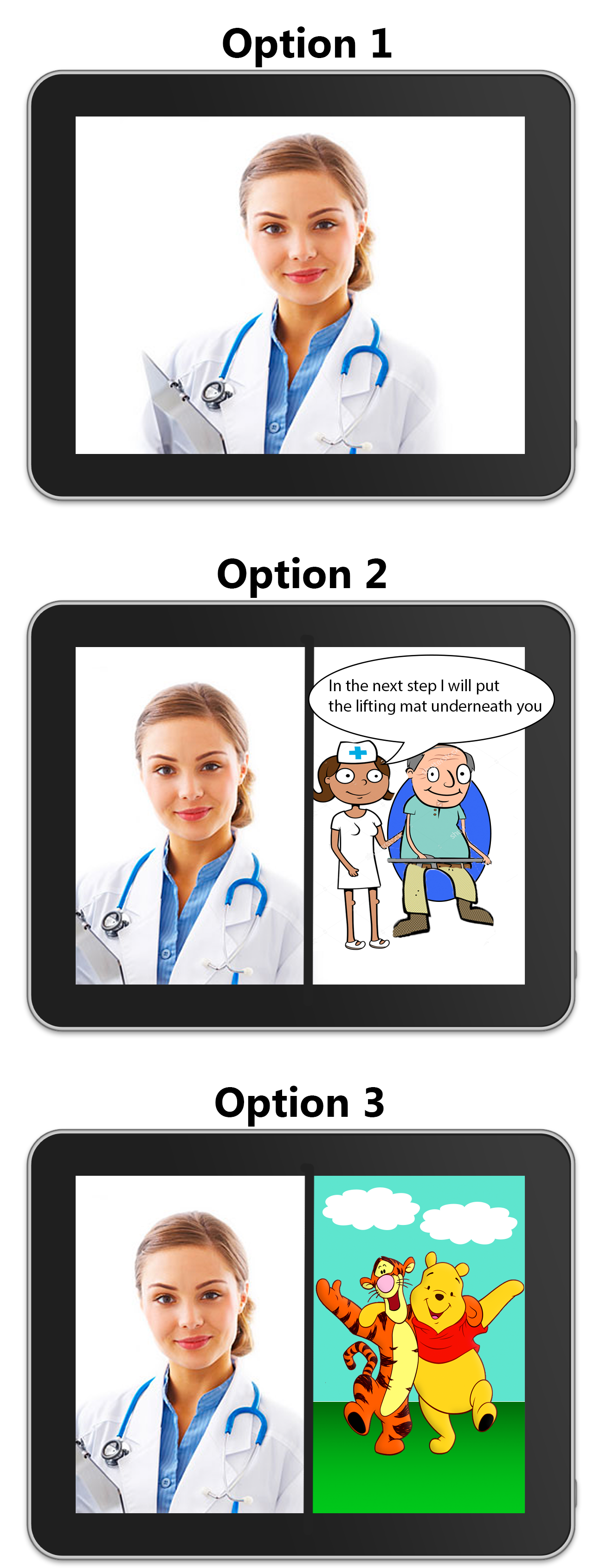
An optimized design for the hoist is made with the program Photoshop CS6 (fig. 8). In this design the requirements were taken into account and added to an adapted version of the 'Wendy' passive hoist.
- 1. (Following requirement a)
- Screen display that is able to sustain a live connection between the caregiver and the patient by an implemented camera. The software on the display is able to show information about the patient in the hoist.
- 2. (Following requirement b)
- Force sensors in handgrips that are able to measure how much force the caregiver is applying while pushing the hoist.
- 3. (Extra requirement)
- Emergency stop button for the caregiver that will immediately shut down all the systems of the hoist when pressed.
- 4. (Following requirement c)
- Electronic powered motor that, in combination with the force sensors, move the hoist by amplifying the force of the caregiver in a certain direction.
- 5. (Following requirement d)
- Camera with a real-time connection pointed at the face of the patient, to sustain eye contact. The camera is also connected with the facial recognition software to detect the emotions of patients.
- 6. (Following requirement e)
- Screen to comfort the patient and make eye contact with the care giver.
- 7. (Extra requirement)
- Holder for the stiffeners.
- 8. (Following requirement f)
- Camera to create a better view of the environment. The caregiver is more able to spot if there are object obstructing the path of the hoist.
- 9. (Following requirement g)
- Spherical wheels for better manoeuvrability.
The improved patient hoist (I.P.H.) in our design 1 is equipped with two interfaces, that will now be evaluated further. There is one interface for the patient (nr. 6 in Design 1) and one for the caregiver (nr. 1 in Design 1).
Interface patient:
The interface for the patient is sketched in figure 9. This will be a display, like for example a tablet. To fill up this display three options can be chosen by the patient and caregiver. In this case they have both control over how they are supported by the added technology.
The first option is that the caregiver is visible for the patient on the display so eye contact between them can be obtained. This is an improvement in comparison with the current patient hoist in which, like in scenario 2, there is no direct eye contact possible between patient and caregiver during the transportation.
The second option consist of the first option with an extra window on the display. This window shows a short animated film clip with a speech function in which the actions of the lifting process are explained to the patient. This option is implemented, because results of the survey and interviews showed that patients like to be informed about what is happening and going to happen during the process. As the patient wishes this option can be switched on or off by the caregiver.
A third option can be implemented to the first option in case the process is executed with for example a demented patient. In this case the display contains an extra window in which an animation is showed to distract the patient during the process. Consequently the process will go more smoothly and pleasant for both patient and caregiver.
All options can in fact be put on or off by the caregiver in compliance with the patient leading to actually four options for the interface of the patient.
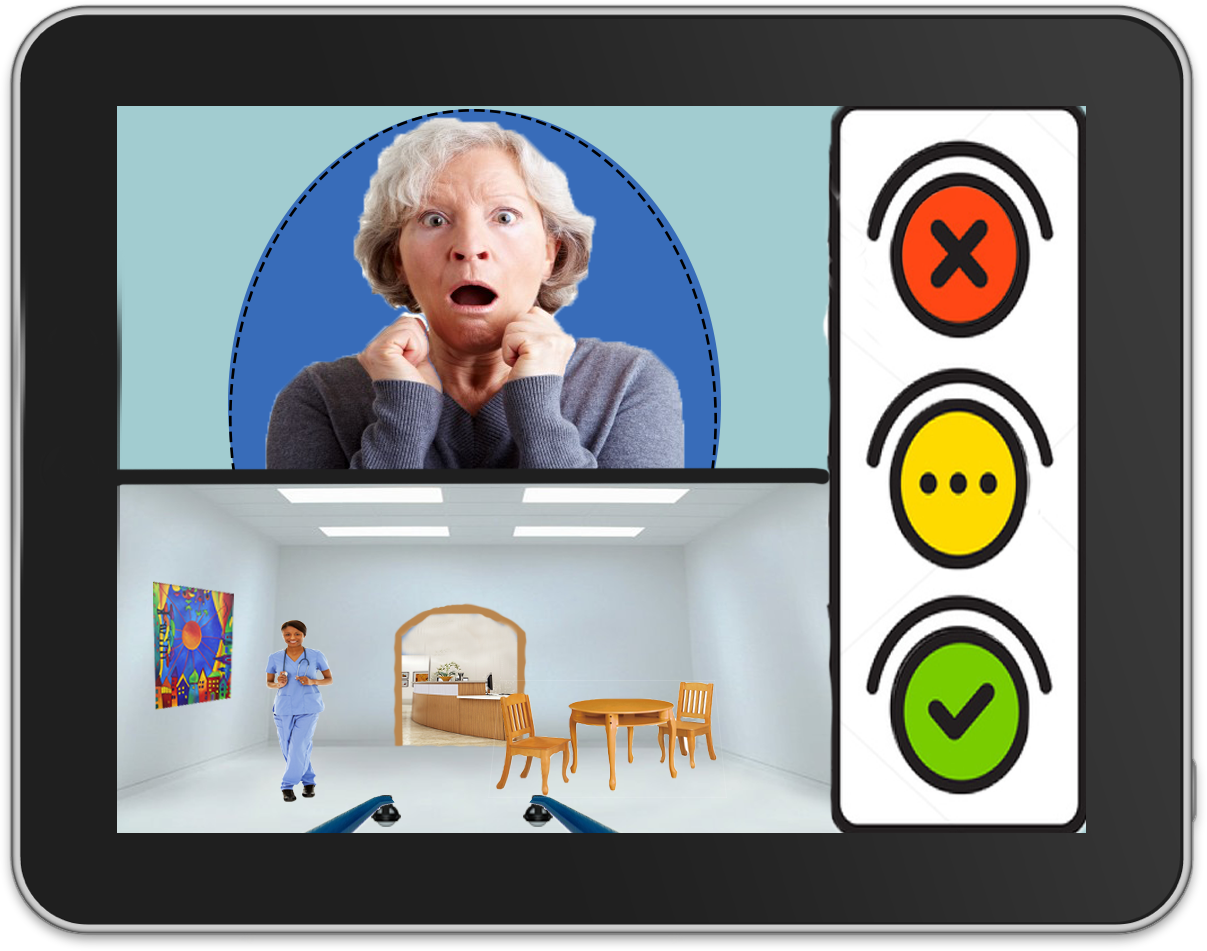
Interface caregiver:
The interface for the caregiver is shown in figure 10. This will also be a display, like for example a tablet, which will be attached at the backside of the patient hoist at face/shoulder height of the caregiver (nr. 1 in Design 1). This display can be changed of position (up and down) so even a tall or a small caregiver can use it properly. On this display the patient lying in the yoke is visible for the caregiver, so eye contact between them can be accomplished. In another window an overview of the environment just in front of the hoist will also be visible on the interface. Due to this the caregiver can easily see what is in front of the hoist and if there are any obstacles that he cannot see for himself from behind the hoist. Further, on the right side of the interface a kind of traffic light system will be visible. This traffic light displays the well-being of the patient during the lifting and transport process. The traffic light is connected to the camera of the patient (nr. 5 in Design 1) which can due to the implemented software of Noldus recognize facial emotions of the patient.
Green light shines when the patient is feeling good and comfortable. In this case the caregiver does not need to change his procedure, the patient is doing just fine in the yoke. Orange light lights up whenever the patient is a little uncomfortable, but the caregiver does not necessarily need to take any actions or alter the transport process for the patient. The caregiver just needs to be more alert, because the chance of changing from orange to red light is higher. The red light shines when the patient is not feeling good, he is scared or uncomfortable. In this situation the caregiver should give attention to the patient and figure out why he is feeling uncomfortable and take action to change this feeling.
The distinction between which color light should shine when will be determined by the results of the test plan for the used facial recognition software of Noldus.
Noldus
In this section the facial expression recognition software 'FaceReader 7.0' from Noldus will be looked into. First a measurement plan is discussed, after which the results are presented after analysis. Lastly conclusions regarding this software will be drawn.
Measurement plan
The goal of this measurement plan is to create a guideline for the two experiments that will be carried out. This will result in a smoother transition between acquiring the materials necessary for the set-ups, performing the experiments and exporting the data.
With the first experiment it is possible to verify if the impact of different circumstances results in a deviant output. What will a difference in distance, angle or light/dark ratio do to the results?
With the second experiment the performance of the Noldus software will be verified by testing a range of basic emotions, by using certain movie segments. Experimental participants (varying in age) are positioned in front of a camera, while being exposed to fragments of themed video material. Key is to execute the experiments with comparable circumstances.
The specific steps that should be taken can be found in the linked file below.
Validation of Noldus
After the experiments were executed the facial expressions had to be analyzed. How this is done is discussed in this section as well as the results of both experiments.
Method
The recordings of the participants are analyzed using Noldus software and their feelings were asked and written down. By combining these two factors and the literature about the movies, it will be determined whether the Noldus software gives valid data about facial expressions.
After the analysis is completed the data can be exported to a .txt file where for every time sample the intensity of every emotion is given. This intensity varies from 0, not present, to 1, fully present, whereas the sum of every emotion never exceeds 1. For every recording where one specific emotion should have been generated, a matlab script (File:Analysis.pdf) determines the mean intensity and maximum intensity. Next, the mean of these means as well as the mean of these maxima were calculated and the standard deviation is determined.
Finally, both values for all emotions are plotted, with and without taking neutral intro account, leading to four figures (fig. 13-16).
It can be concluded that the Noldus FaceReader software is valid if the highest mean and maximum emotion is the emotion that is expected from reporting of participants and from the literature.
Results
Experiment 1
By daylight the software was able to detect the face of the participant until a distance of 2 meters between the webcam and the participants face. By daylight and 0.5 meter distance between the participant and the webcam the software was able to detect the face that was turned right until an angle of 45 degrees was reached. The same holds for turning the face to the left. Turning the face down the software was able to detect the face until an angle of 20 degrees, whereas the software kept on detecting the face when looking up until the neck of the participant was fully stretched. Increasing the distance led to an increase of allowable error in every direction. By changing the dark/light ratio is was observed that the software is very sensitive to light. By daylight there are no problems, however in a slightly darker room, where the curtains are closed, the maximum distance between the face and the webcam decreases rather fast, as well as the allowable angle. Turning light right into the camera has the same effect.
Experiment 2
First one has to note that the movies that are selected in the research show strong emotional responses, but not facial expression responses as these emotional responses were determined by measuring heart rate and respiration. So there is a chance that not much responses will be shown in the tests, but this does not mean that the software is not valid. Furthermore it is mainly focused on analyzing only the most important emotions for this project, meaning happy, sad and fear.
Figure 13 shows the analysis of the sad movie. What stands out is that neutral is minimally twice as high as the other emotions. This can be due to the selected movie as not every moment was sad. When the neutral emotion is neglected it is shown that sad is indeed the main mean emotion. For this reason in the next analyses the focus lies on the graphs where neutral is filtered out. Happy is also quite high in the maximum emotion graph. This is a striking result, because it could mean that in the software a sad emotion is easily confused by a happy emotion. This could however also be due to a high intensity of happiness at some point, because the happiness in the mean graph is not that high at all. Also anger is somewhat higher than the other emotions, however none of the participants reported feelings of anger so this might be an error in the software. Nonetheless, sadness and anger are on the same side of arousal in the valence arousal model so this also is a very plausible observation.
Figure 14 shows the analysis of the happy movie. It can be seen that the values of happy are high. The mean of happiness is even similar to the mean of neutral and the max is even higher. When neutral is neglected, a peak is visible in sad emotions, however happy still is twice as high. As in the previous figure sadness also was confused with happiness it can be stated that the recognition of Noldus needs some improvement. Happy and sad seem to be coherent in the software to some extent. Nonetheless, it can be concluded that the software of Noldus appropriately reports happiness as the main emotion when participants also report happiness.
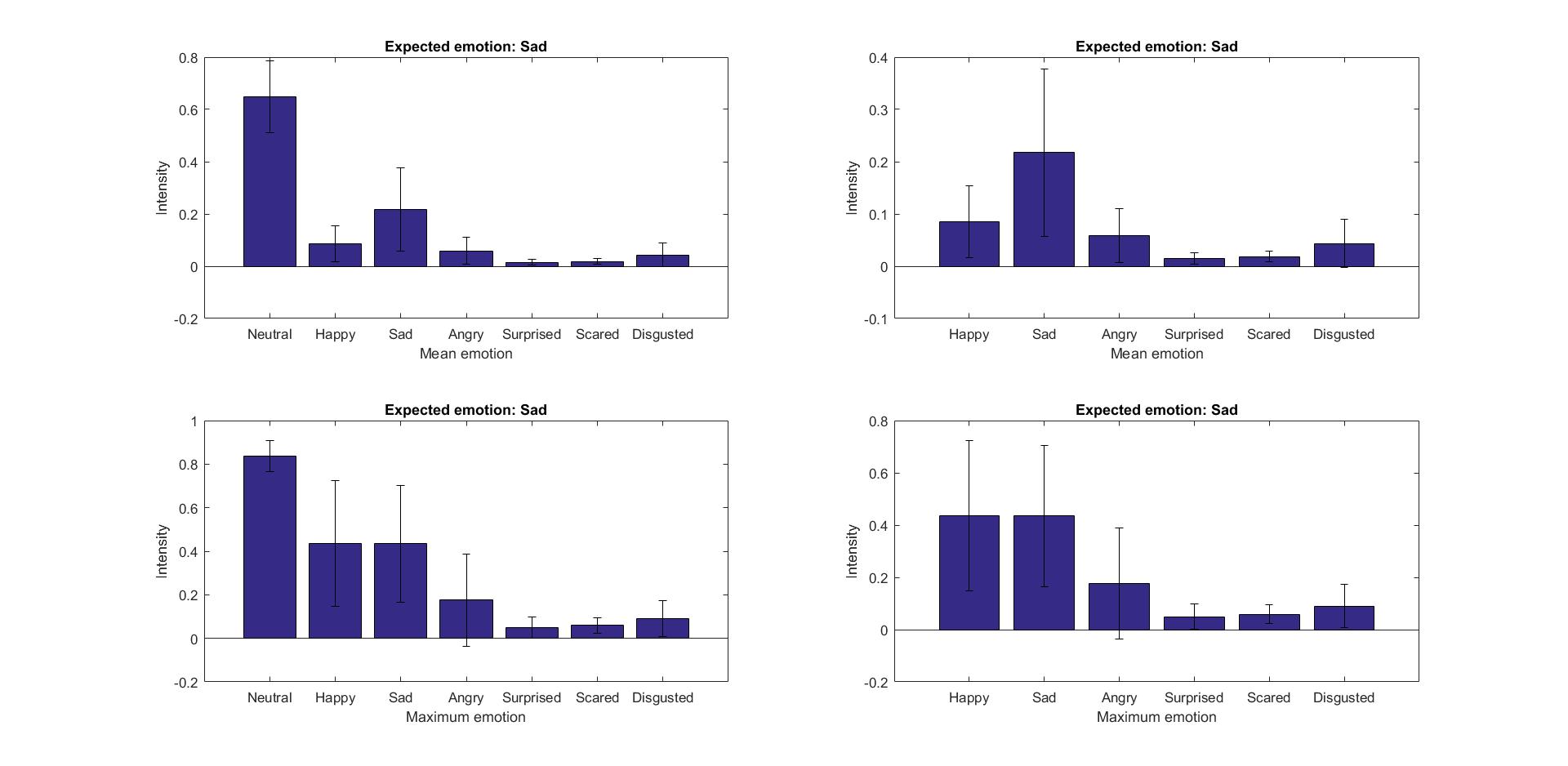 |
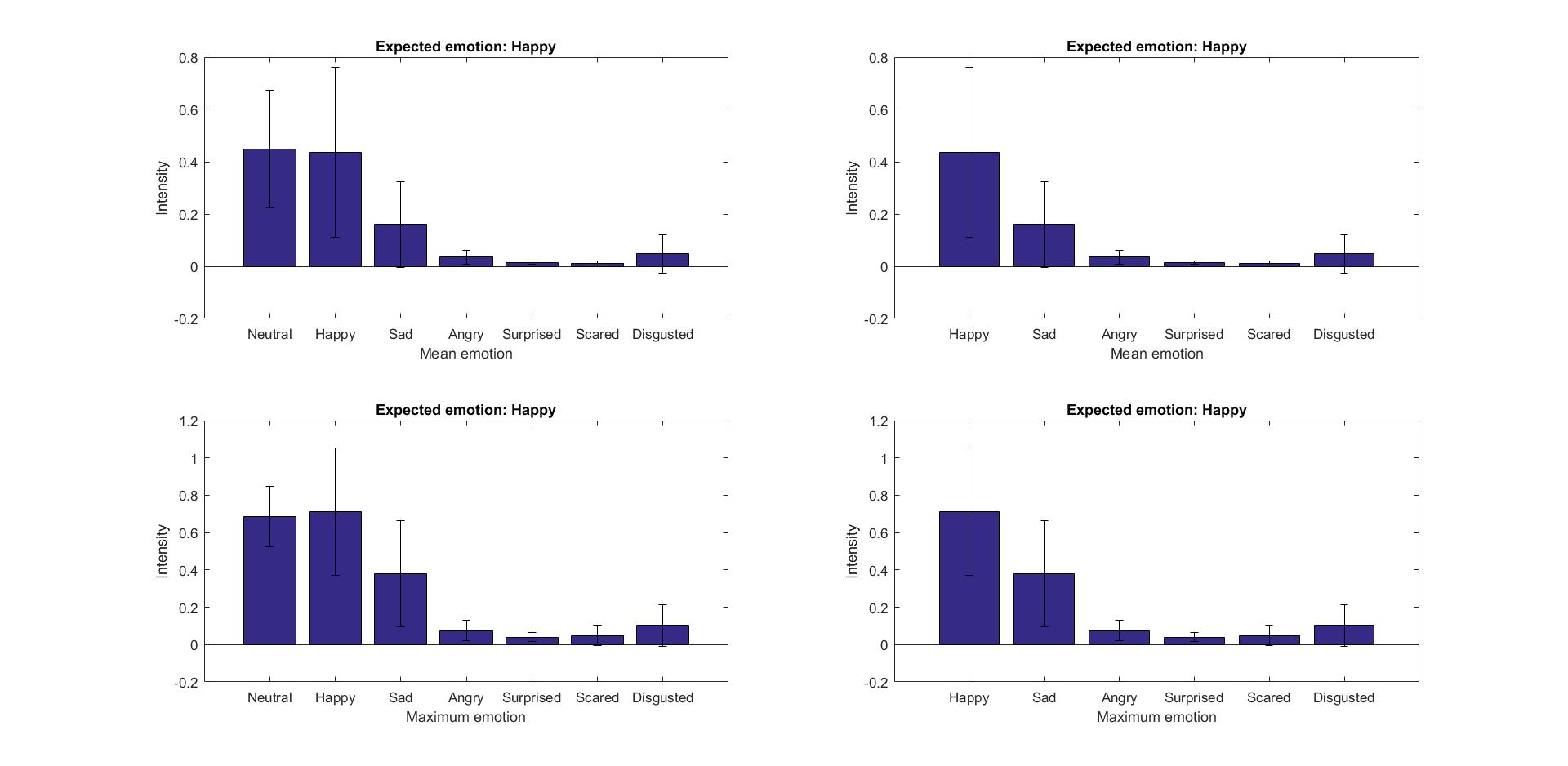 |
The most important emotion for improvement the hoist is scared. Therefore two analyses of this emotion were conducted. Scared 1 shows fearfulness over a longer period of time and Scared 2 shows a very brief moment of shock. As visualized in Figure 15, happy is the main mean emotion besides neutral. Furthermore, the second highest mean emotion is sad. This is not as expected. In Figure 16 the sudden shock is analyzed. This is another way of measuring fearfulness. Contrary to the scene of the shining, in this movie happy is not high. Neutral on the other hand is high, but this is neglected. Visible again is that sadness is high instead of the scared that was expected. Also disgusted is slightly higher than the other emotions. Disgust can be difficult to distinguish from fear, because jaw drops and eyebrow changes. The emotions on one side of the valence level are often somewhat confused, but there is little confusion between the negative of positive valence levels.
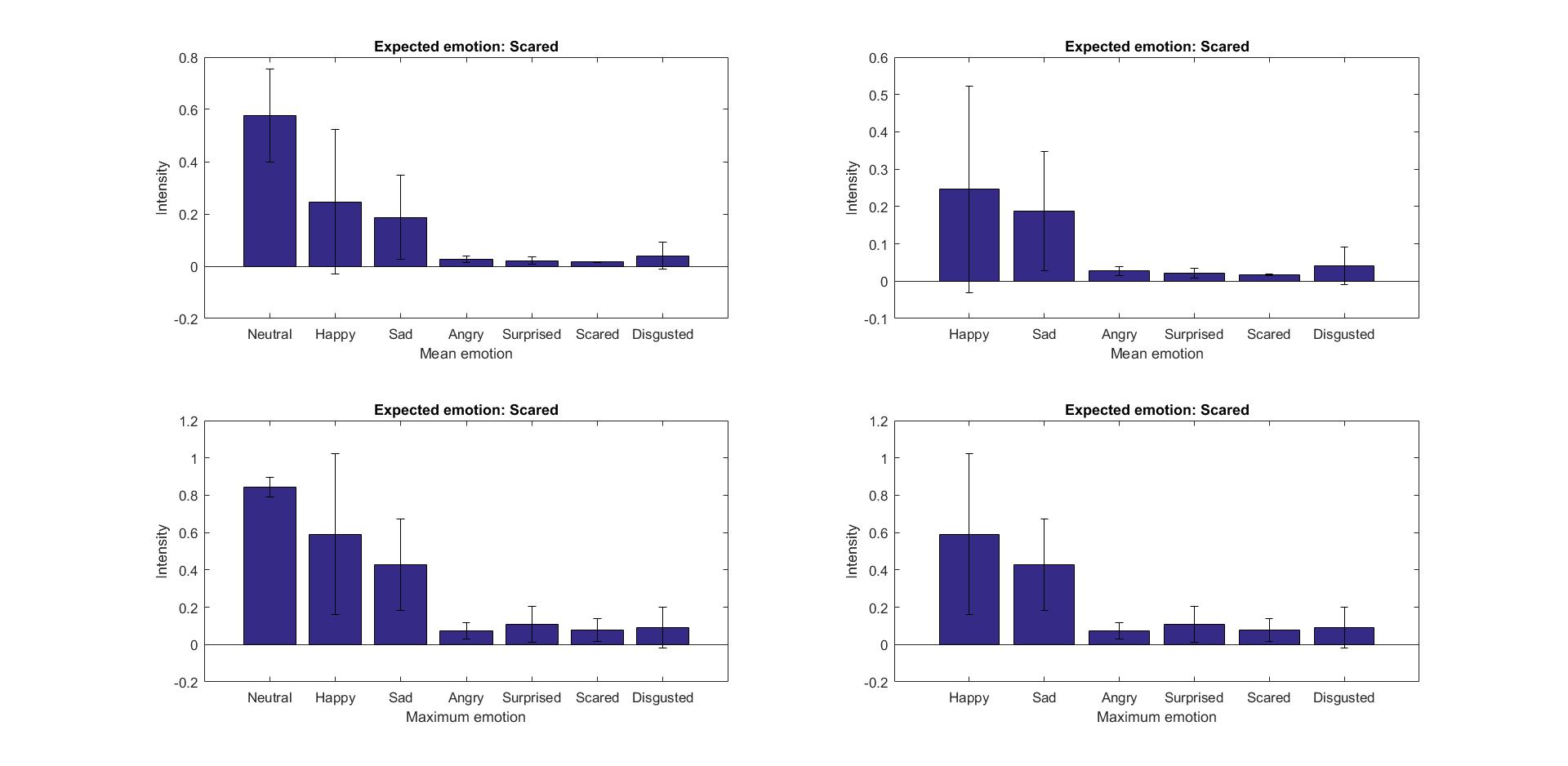 |
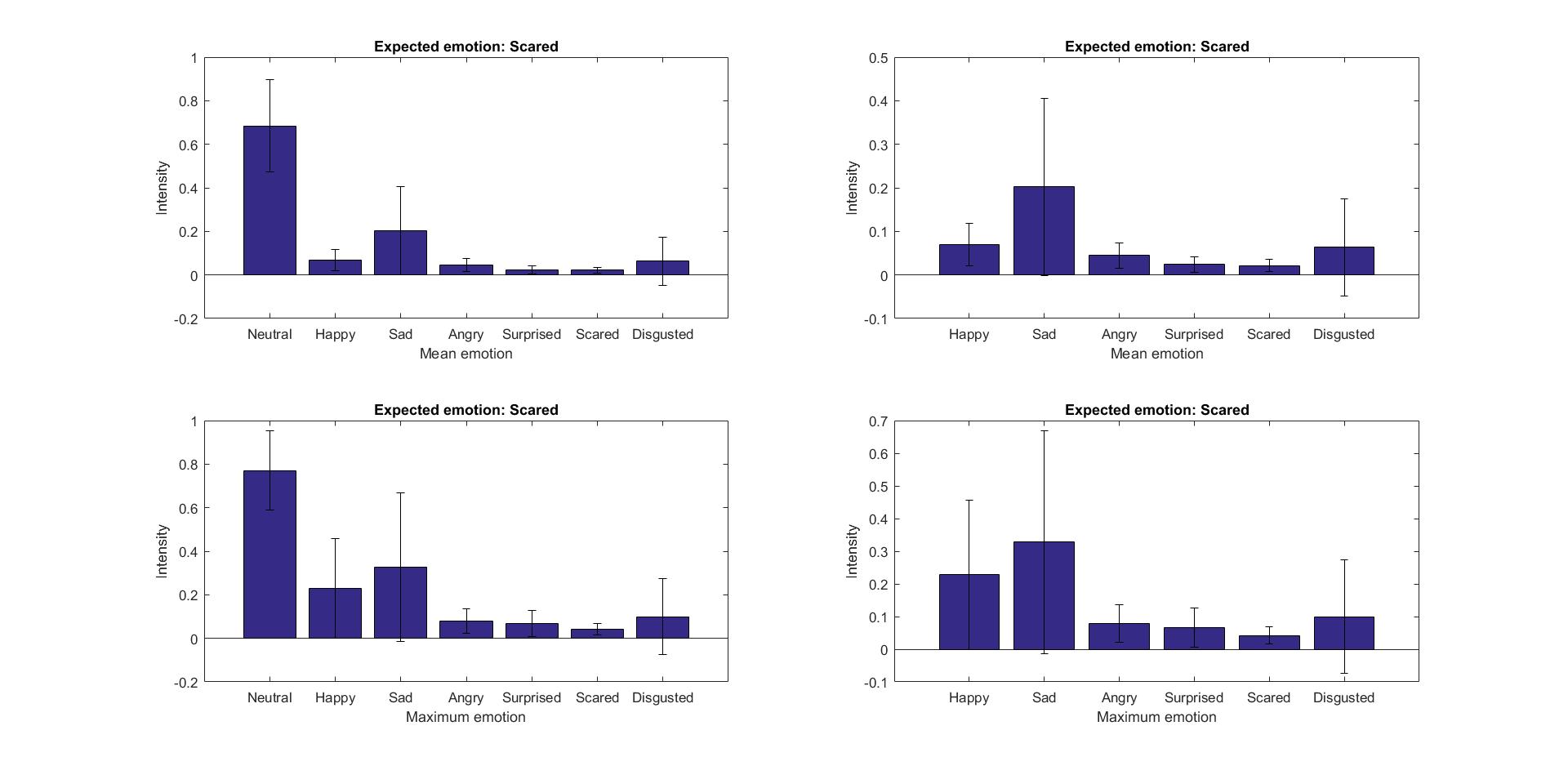 |
Conclusion
By daylight and an angle between the face that should be detected (in the allowable range of left/right: 45 degrees, down:20 degrees and up: 60 degrees) and the webcam, the software is able to detect the face without any problems. As soon as more or less light is available the software’s performance is decreasing. A solution for this could be to attach a light near the camera that shines on the face of the patient in the patient hoist, so the software is able to detect the face, even when the room is dark
What mainly can be concluded is that the Noldus Software did not always respond as expected. Reasons for this could be because small facial changes of, for example, fear are very hard to observe, the movie fragments were not good and long enough to arouse certain emotions or the participants were too much influenced by their environment to take the experiment seriously. However, something else is standing out. The software might not show the precise emotion accurately, because mainly happiness, sadness and neutral were reported, but the level of arousal on the other hand is quite precise. When Noldus reports neutral the level of arousal is 0, for negative emotions the level becomes negative and for positive emotions the level becomes positive. Negative arousal emotions are anger, sad and disgust while positive arousal emotions are happy and surprise. This can be seen from the valence arousal model of Russell. In the analysis it can be seen that the emotions on one side of the valence level are often somewhat confused, but there is little confusion between the negative and positive valence levels. For this reason, and also due to the fact that the received software only exports data from which valence can be determined, the “traffic light” system mentioned above will be based on the level of valence instead of the specific emotion. The next section will more elaborate on this.
Emotion detection
As explained above, distinguishing different specific emotions lead to complications, which are undesirable. So, instead of focusing on these specific emotions and whether this one emotion exceeds a certain intensity, valence is used to determine the state of a patient’s emotion. (Arousal is not taken into account, since the software received from Noldus is not able to output the activity of the Action Units, which are needed to be able to calculate arousal). To calculate valence the intensity of positive emotions, like happy, as well as negative emotions, like anger, fear, sad and disgust, are needed for every time sample (surprise is not taken into account since it can be positive and negative).[14] Consequently, valence is the subtraction of the intensity of happy and the highest negative intensity, leading to a range for valence from -1 to 1, where -1 is purely negative and 1 purely positive. Using this, the idea of a traffic light system on the nurses display can now be realized, as can be seen in the figure below. The matlab script is given in this file: File:Trafficlight.pdf
The traffic light given in Figure 17 is green when the valence is higher than 0.3, red if it is less than -0.3 and yellow when the valence is in between. This treshold can be varied for every patient personally.
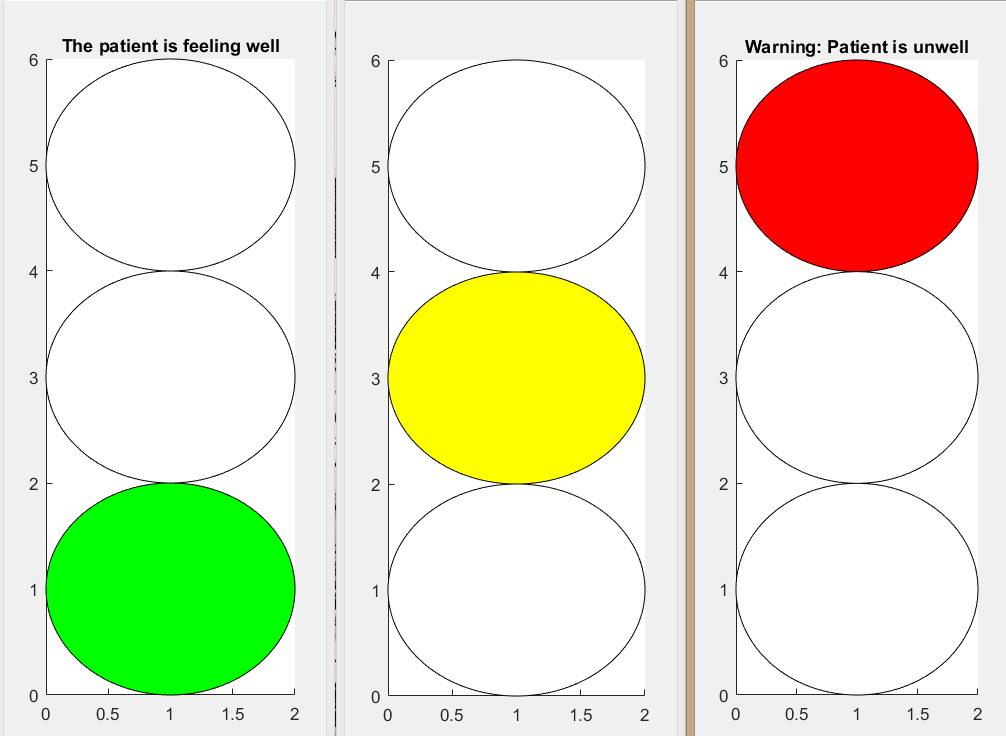 |
Demonstration
The purpose of the demonstration is to form a clear image of the future vision of the improved hoist. The invented adjustments that have been examined in the last few weeks are also implemented.
Here a link to the created short film clip of the demonstration is given: https://www.youtube.com/watch?v=r1jxQCQQBQQ&feature=youtu.be
Feedback
To verify whether the implemented adjustments on the passive patient hoist shown in Design 1 are successful enough, feedback has been gathered from several caregivers who are acquainted with this hoist. Two of these caregivers have also taken part in the interviews at the beginning of our research, so they were a little bit more informed about the project already and three new caregivers were asked for feedback.
The feedback was gathered by first briefly explaining to the caregivers what our research is about and how our arranged requirements are implemented in our first design. Secondly Design 1 with the several invented interfaces were shown to the caregivers and per adjustment was explained why it has been implemented. The caregivers were asked to give their opinion about the adjustments and whether they would adjust or add anything to the design.
The results per feedback interview are listed below and a general conclusion from these feedback interviews is concluded.
Feedback 1
From this feedback interview can be concluded that our adjusted design of the passive patient hoist is indeed a good improvement. The bigger wheels actuated by a motor are very convenient as it reduces the required power of the caregiver to move the hoist, because it is not an easy task to push the current hoist with a patient in the yoke. The solid spherical wheels in the front of the hoist are also considered as handy since they make it easier to turn the hoist in another direction. The emergency stop is already implemented on the current hoist, however the position of this button is too low. The one shown in the design has a better position in the working space of the caregiver. The camera for navigating the hoist is regarded as a good adjustment. Especially with for example cables lying underneath beds etc. it is a fine implementation that can make spots visible for the caregiver and it can prevent collisions. This camera can be of good use for distances in one small busy room as well as for the transportation process. The addition of a holder for the whalebones of the lifting mat is considered very clever, even though it is such a simple adjustment it is really a good one, because the whalebones are now in no way connected to the hoist. The interface of the caregiver can support the caregiver in his tasks, although the caregiver should be able to open or close windows however he prefers. The traffic light system makes the caregiver extra alert which is therefore an advantage to provide good care. The options for the interface of the patient should all be possible as every patient is different and it should again be possible to switch options on or off. The control over these options should be given to both caregiver and patient, as long as patients are able to use these digital methods. An extra improvement for this design could be a kind of peg adjusted on the hoist so the lifting mat can be hung up on. Now the lifting mat is just thrown over the hoist which makes it easier to be worn out and whenever there is just a small hole in the mat it may not be used anymore because of safety aspects. The overall impression of the design is therefore positive and it will be an advantage for both patient and caregiver.
Feedback 2
The feedback from this interview is quite similar to the first one. The motorized wheels are considered as a real advantage for the caregiver. It can prevent back pain for the caregiver as it reduces their needed strength to push the hoist. The spherical wheels are just as in feedback 1 found very handy so turning the hoist in the desired direction will not be an issue anymore. It is found strange that those spherical wheels are not implemented yet or in more other equipment like for example a wheelchair. The position of the safety button in the design is more suitable than the current position, especially when more electronics are implemented it is important to be able to switch the hoist off. The camera for navigation and the holder for the whalebones are considered as a good addition just like in feedback 1. For the interface of the caregiver again the same good feedback was provided, however now the question arose whether it was possible for the used software of Noldus to determine the emotions of patients who have a facial paralysis or a defacement. Further the approach of a traffic light system to warn the caregiver is just fine, however instead of different light colors also smileys could have been used or something similar considering caregivers that are colorblind. The options for the interface of the patient are a good implementation to ease them when they are not feeling comfortable or scared. It depends on the patient which option will be chosen and this should be chosen by the patient if possible. Option three for demented or retarded patients is good, because an animation can distract them, however the animation should be chosen with care, because some subjects are sensitive.
Feedback 3
The overall impression about the improved design was stated as positive during this interview. The motorized wheels are a good idea, however they should be carefully tested especially in small rooms. The motorized hoist and the strength by which the caregiver pushes the hoist should be well adjusted to each other, so the hoist does not react jerky or moves to fast and risks to bump into things. The spherical wheels, the emergency button, the camera for navigation and the holder for the whalebones are all considered as good adjustments in the current design of the passive hoist. Option one (visible caregiver), three (visible caregiver and a short film clip for distraction) and four (different options combined or switched on and off) for the interface of the patient are useful supplements and can either improve the interaction between caregiver and patient or comfort the patient more during the lifting process. Option two (visible caregiver and a short film with instruction) is on the other hand not necessary. Not all patients will understand these kind of instruction film and as a caregiver you provide these instructions yourselves to the patients verbally. The interface of the caregiver is also a good adjustment to improve the interaction between patient and caregiver and it can smoothen the whole process by giving feedback about a patient’s condition with the traffic light system and by giving information about the badly visible surroundings just in front of the hoist. However questions arose whether the used software to detect facial emotions will be useful for patients with for example Parkinson’s disease and whether caregivers will not focus too much on the interface instead of the whole hoist so the risk of collisions will increase while moving the hoist. At the end another option for a more future design for the interface of the caregiver and the control of the hoist was given. Instead of pushing the hoist by the caregiver himself, it should be driven by using something like a IPad by the caregiver. In this case the caregiver can walk next to the hoist and the patient while stirring the hoist from the IPad. Interaction between caregiver and patient will be improved by reducing the distance between them and the workload for the caregiver will decrease as he does not need to push the hoist manually anymore.
Feedback 4
From this interview can be concluded that the made adjustments in the current hoist are good and useful to improve the lifting process. Especially the motorized wheels in combination with the spherical wheels in front of the hoist are a very big improvement. The turning and pushing of the hoist is now experienced as hard and even more difficult then moving a full and heavy shopping cart. The motorized and spherical wheels will make this process a lot easier by reducing the workload of the caregiver. The emergency button, the camera for navigation, the holder for the whalebones and the interface of the caregiver are considered equally as in feedback 3. The options for the interface of the patient is also evaluated the same as in feedback 3 where option two should be omitted. Option three is a good option for comforting and distracting the patient, but no animation should be used. Instead a short film clip about nature with waterfalls or woods should be used to entice their attention.
Feedback 5
Just like the other feedback interviews the overall impression of design 1 is considered positive and with real advantages in comparison with the current hoist. Just as stated in feedback 4, the motorized wheels and spherical wheels are very handy as turning will not be an issue anymore and less physical power of the caregiver is needed. This adjustment will reduce the workload of the patient and their back pain which is obtained by frequently using the hoist. The emergency button and the holder for the whalebones are considered equally as in feedback 3. The camera for navigation will also be of good use. Especially for managing the hoist under beds and chairs where cables or attributes like shoes can be avoided now and it is not necessary for the caregiver to get down on his knees anymore to see what is interfering with the hoist. Therefore the interface of the caregiver is well equipped especially with the window of the surrounding just in front of the hoist. Option three for the interface of the patient can be of good use for demented patients. A short film clip as mentioned in feedback 4 should be used or perhaps a little bit of music could be added to it. It is probably good that the caregiver is also visible on the interface of the patient as it is more comforting to see a matching face from the caregiver who is talking to the patient from behind the hoist.
Conclusion feedback
From all the gathered feedback can be concluded that design 1 is indeed an improvement of the current passive patient hoist. The bigger motorized wheels are a very good adjustment to the current hoist. They reduce the workload of the caregiver to move the hoist and be doing so they can prevent back pain for the caregiver by frequently use of the hoist. However this motorized system including the force sensors (nr. 2 in design 1) should be tested very properly, because the motorized hoist and push load of the caregiver should be well adjusted to each other so no jerky reactions or collisions by too fast movements are obtained. In all the feedback interviews was stated that the spherical solid wheels are actually a must for the improved design of the hoist. They make it easier to turn the hoist in a desired direction and in combination with the motorized wheels they will make the lifting process a lot easier by reducing the workload of the caregiver so less physical power of the caregiver is needed. The position of the emergency stop in design 1 is more suitable than the lower current position on the hoist, because it is positioned in the working space of the caregiver. Especially when more electronics are implemented it is important that the hoist can be turned off right away. The camera for navigation is regarded as another good adjustment to the current design. Especially for managing the hoist underneath beds and chairs where cables and other attributes can be avoided. It is a fine implementation that can make spots visible for the caregiver and it can prevent collisions. It can be of good use in small busy rooms as well as for the transportation process. Although simple yet a very handy adjustment has proven to be the addition of a holder for the whalebones of the lifting mat as they are now in no way connected to the hoist and they are often lost. The interface of the caregiver can support the caregiver in his tasks. It improves the interaction between patient and caregiver by making eye contact possible form behind the hoist, it smoothens the process by giving feedback about a patient’s condition by use of the traffic light system and it provides information about the surroundings just in front of the hoist. The traffic light system extra alerts the caregiver which is therefore an advantage to provide good care, but questions arose whether the used software to detect facial emotions can be used for patients with facial paralysis or defacements and whether caregivers will not focus too much on the interface so the risk of collisions will increase while moving the hoist. Options one, three and four for the interface of the patient are useful adjustments and can either improve the interaction between caregiver and patient or comfort the patient more during the lifting process. Option three is a good option for comforting and distracting patients when both caregiver and short film clips about the nature are visible to entice their attention. Option two is not necessary, because not all patients will understand the given instructions. The caregiver provides these instructions himself verbally to the patient during the process. The control over these options which can be turned on or off should be given to both caregiver and patient, as long as the patient is capable to do so. Other adjustments like a peg for the lifting mat and another kind of control system for the hoist by using an IPad have been stated in the gathered feedback. These can perhaps be incorporated in a final or future design.
Final Design
Based on the gathered feedback about design 1, it can be concluded that most of the made adjustments on the current hoist are useful and should indeed be implemented in the new design. To create a final design of the passive patient hoist a few changes in design 1 will be made which will be explained further.
An extra improvement which is stated in feedback interview 1 for design 1 is that a kind of peg should be adjusted on the hoist so the lifting mat, which is now just thrown over the hoist, can be hung up on. This adjustment is implemented in the final design as it is proven that the current manner at which the lifting mat is hung up is bad for the mat as it is easier worn out which reduces the safety of its use.
Another addition to the design is a small light source next to camera for navigation (nr. 8 in design 1). This will improve the visibility of the environment of the camera as it has been stated in the feedback interviews that the legs of the hoist will be shoved underneath beds and chairs.
Requirement d (“The hoist should be able to recognize anxiety in the patients”) is satisfied in design 1 by using facial expression recognition software of Noldus. However, the software cannot detect facial emotions by patients with facial paralysis or defacements. Therefore the previously proposed software of MIT in which emotions of persons are detected by taking respiration and heart beat into account will be implemented in the final design besides the software of Noldus. The output of the MIT software will also be connected to the traffic light system just like the output of the Noldus software so the caregiver can be alerted whenever the patient is feeling uncomfortable. This way more patients, even patients with facial paralysis or defacements can be taken into account for the improved design.
To make the implemented traffic light system in the interface of the caregiver also functional for colorblind caregivers as stated in feedback interview 2, symbols inside the red, yellow and green light are used like in figure 10. These symbols will be visible whenever the red, yellow or green light shines.
Due to the feedback about the interface of the patient the following changes are made for the final design of the hoist. Firstly, the second option for the interface of the patient in which the caregiver and a short film clip about the actions of the lifting process are explained is removed. This is done because not all patients will understand the given instructions and the caregiver prefers to give these instructions himself verbally to the patient during the process. Secondly, the third option for the interface of the caregiver in which the caregiver and an animation for distracting the patient is showed is adapted. This change consists of showing a different short film clip, like one about nature with waterfalls or woods to entice the attention of patients with for example dementia as these sort of films are more comforting for them.
Finally the control over all options for the interface of the patient which can be turned on or off is given to both patient and caregiver. The patient can choose from the different options on his own interface (nr. 6 in design 1) and the caregiver from his interface (nr. 1 in design 1). Normally the patient will have full control over the given options, but whenever the patient is no longer capable of controlling these options, the caregiver will do it for him.
All the above mentioned changes lead to the final design of the I.P.H.
Discussion
A design for an improved hoist was obtained. Although this design well-founded, there are also several limitations to the research done. Some of these problems can be solved in further research.
First of all, it was not possible to interview patients and a limited amount of surveys were filled in by patients. This is due to the fact that patients who have experience with the hoist, are a very fragile group. Often they are old and have dementia. Most nursing homes would not let us ask questions to this patients, because that could upset them or they would not understand us anyway. Nurses could tell us a lot of what they thought to be the desires of the patients, but it would be better if the patients were asked themselves. Some of our solutions might have been rejected or patient could have had very specific problems with hoist the nurses did not know about. The improvements in our design are therefore mainly based on the view of nurses on the problems of patients. This can be different from the problems the patients experience themselves.
Secondly, there were a couple of problems with the Noldus Facial expression recognition that was used. For instance, the version that was obtained did not have the possibility to export the data real-time. This meant that it was only possible to export and analyze the data at the end of recording. It was possible to see the data in the program itself real-time, but for using it for the interface of the nurse, it needed to be exported it to the script that was written, in real-time. The traffic light system that was designed could only work afterwards. This problem, however can be easily solved for anyone who would like to implement our design by obtaining the right software. Another problem that was encountered was that the software was not able to export the data on arousal, only on valence. The script for the lights of the traffic light could be more accurate with this data. At the moment it only uses valence, which means that every negative emotion can change the traffic light. Ideally the traffic light would only respond to fear, but for that data on arousal is needed. This problem could also be solved by obtaining the right software.
Furthermore, an important limitation of the research is that the software was not tested on people who are partly paralyzed or have a disfiguration in the face. It is possible that the software does not work well on these kind of patients, which can lead to false signals towards the nurse. This problem can be solved however by measuring heart beat or respiration as mentioned in the requirements. The technology using radio frequency signals (see requirements) that MIT has invented can also work for this, but this technology is rather new and needs to be developed further, before it is possible to implement it in the hoist.
Conclusion
The goal of this project and the experiments was to improve the current passive patient hoist in ways that would result in more convenience for the primary users, thus for the caregiver and the patient. In literature hardly any research is found about the use of patients hoists in hospitals and nursing homes.
Considering the fact that there has been little research done about the passive patient hoist, it was stimulating to start a new experiment in which the current hoist could be improved, whereby two main hypotheses were formulated: ‘Caregivers need to be supported by the patient hoist’ and ‘Patients and caregivers attach value to interaction during the process of lifting’. Based on the results of the interviews and the survey of the first hypothesis can be concluded that there is a need for care givers to be supported by cameras for navigating the patient hoist and that the caregiver would like to be warned by the hoist whenever the patient is feeling anxious. From the second hypothesis can be concluded that both caregivers and patients prefer eye contact more during the interaction than speech and physical contact.
Based on the results of the interviews and the survey seven requirements to improve the current passive hoist were made and implemented in the first design. Two of these requirements, which are more elaborated in the experiment, are ‘During the whole process eye contact between the patient and the nurse is guaranteed’ and ‘The hoist should be able to recognize anxiety in the patients’. To satisfy these two requirements cameras are implemented in the first design and software of Noldus was used to test the facial expressions of the patient. Additionally a traffic light system is implemented on the interface of the caregiver which is connected to the camera of the patient. Due to the implemented software of Noldus it could recognize facial emotions of the patient. This traffic light system had been tested and works sufficiently.
As the overall impression about the gathered feedback of design 1 is positive, it can be concluded that the implemented adjustments of design 1 are indeed an improvement of the current passive patient hoist. Due to this feedback some little adaptations have been done leading to the final design of the passive hoist. This all has resulted in the creation of two different end products, namely one new hoist design that consists of all adjustments, portrayed in figure 18, and another one that will function as an add-on for the current hoist, portrayed in figure 19.
 |
 |
Future research
Finally possibilities for future research will be examined. The most important follow-up research that needs to be done is research on the actual implementation of the improved hoist. It needs to be researched in what extent the design improves the comfort for the patient and nurse and the effectiveness of the nurse. This can be done by actually producing the hoist and testing it in a nursing home under standard circumstances. Furthermore, a lot of other aspects need to be taken into account before the design can be implemented. For this research, only the primary users were considered, but before implementation takes place it is important to look into the requirements for secondary and tertiary users, too. For instance, the costs of the design are still unclear just like the regulation concerning the improvements. These aspects are beyond the scope of this research, but it should be investigated in future research. The patients and nurses could also be more directly involved with the implementation. In further research it would be recommended to include the users in the research group. Lastly, in the proposed design the nurse is still present during the transfer. However the proposed design can be a stepping stone towards full automation, because some of the needed technology for full automation is already implemented in our design. Thus it can make the caregivers and nurses become more familiar with robotics.
References
- ↑ http://www.domicare.nl/tilliften-badliften-verrijdbaar/
- ↑ http://www.arjohuntleigh.nl/producten/transfer-oplossingen/actieve-tilliften/
- ↑ 3.0 3.1 Johnsson C., Kjellberg K. & Lagerstrom M. (2004) A direct observation instrument for assessment of nurses’ patient transfer technique (DINO). Applied Ergonomics35 (6), 591–601.
- ↑ 4.0 4.1 http://ovidsp.tx.ovid.com.dianus.libr.tue.nl/sp-3.22.0a/ovidweb.cgi?QS2=434f4e1a73d37e8ce55b227ffaae5fa148541856cb5686bfad9f6431240b98c07524237e1720f34b02eb8fa2b88b7b97cae33df7331783914f69c8dde4ca12d06569431bde95318885c0300c9e4cb854a6adb57292dc4b9d5d515362ffaf06f20e36f3c9460a88b948e9e5dcf4c00bab436508a09afdce5366e7c719263f67d40a206676fd0c0a5686e4e1da71239e75c2ce0637418cb6107561917b1c775b62b2deac9baf23bbafabe516e9e595ddb3711a24619f5e9fff0b6524d61d8e55df726a6944468052b4402c3d9ae720be38f03cb8a56190a0535e3fa712b6c3423a74b470672b139464e79db6d185645a45cb60d8e15bd92bcee10aa989a2dfbadeef09927167e35fcee3135359c01e825083f314bc5221e7c8644d3bbcbe868deccbffbe8e7109265789c479c547d2e3fdb26a430178a76903ff214576e1d05cdf304d7473261f3c184d70eea1d98c1e23e9483a61fdd973d2af33538480ec1aee29fd33ec82224c9b14f035663bed6db11254245dfcda166d7bd10d7e687e549e4d066e920b3493fb}}
- ↑ 5.0 5.1 Finlay, P. A. (1992). PAM: a robotic solution to patient handling. Industrial robot, 19(3), 13-15.
- ↑ Griffiths, H. (2012). Adverse risk: a ‘dynamic interaction model of patient moving and handling’. Journal of nursing management, 20(6), 713-736.
- ↑ Leanne S. Bohannon a,⇑ , Andrew M. Herbert b , Jeff B. Pelz c , Esa M. Rantanen, Eye contact and video-mediated communication: A review., file:///C:/Users/s130798/Documents/School/Year%203/Robots%20everywhere/Literatuuronderzoek%203-10/1-s2.0-S0141938212001084-main.pdf
- ↑ Todorović D. Geometrical basis of perception of gaze direction. Vision Research 46:3549-3562, 2006
- ↑ Franc Solina, Robert Ravnik, Fixing Missing Eye-Contact in Video Conferencing Systems, http://ieeexplore.ieee.org.dianus.libr.tue.nl/stamp/stamp.jsp?arnumber=5974027
- ↑ 10.0 10.1 Hwang et al. method and apparatus for providing eyecontact function to multiple points of attendance using stereo image in video conference system, 2016, http://www.freepatentsonline.com/20160150182.pdf Cite error: Invalid
<ref>tag; name "Hwang" defined multiple times with different content - ↑ Jinglin Zhang Cong Bai Jean-Francois Nezan Jean-Gabriel Cousin, Joint motion model for local stereo video-matching method,2015, http://opticalengineering.spiedigitallibrary.org.dianus.libr.tue.nl/article.aspx?articleid=2478969
- ↑ http://nordicapis.com/20-emotion-recognition-apis-that-will-leave-you-impressed-and-concerned/
- ↑ Zhao, M., Adib, F., & Katabi, D. (2016, October). Emotion recognition using wireless signals. In Proceedings of the 22nd Annual International Conference on Mobile Computing and Networking (pp. 95-108). ACM.
- ↑ Loijens, L. and Krips, O. FaceReader: Methodology Note, Retrieved from http://www.noldus.com/files/file_manager/downloads/whitepaper/FaceReader_Methodology.pdf
Appendix
Planning
Short version planning
- Gathering information (week 1-3)
1) Interviews (week 2-4)
Making interview (week 2) (1h)
Conducting interviews (week 3-4) (10h)
Processing results interviews and conclusion (week 4) (4h)
2) Surveys (week 2-4)
Making survey (week2-3) ( https://docs.google.com/forms/d/e/1FAIpQLScinjbrL8rMoxs1CQOP0JCgIO3u_tavH2K1LGRcKIa9q_bFVA/viewform )
Conducting survey (week 3) (8h)
Processing results survey and conclusion (week 4) (4h)
3) Literature research (week 2-4)
State-of the-art (9h)
Human-Robot interaction (9h)
Specific (...h)
4) 1st design (week 4-5)
Design/sketch (perhaps 3D-model) (week 5-6) (4h)
Description (week 5) (10h)
5) Potentially prototype (week 5)
Reading in(4h)
Programming (7h)
6) Feedback (autorative) (week 4-6) (6h)
7) Potentially testing prototype (week 6) (10h)
8) Final design (week 7) (5h)
9) Wiki
Week 2-6 (Every member 1 hour per week for adding and restoring information etc)
Week 7 (each member 2 hours)