PRE2016 3 Groep8
Student Numbers of group 8 members
- 0957735 Ainse Kokkelmans
- 0895428 Joris Veens
- 0955135 Jolien van der Thiel
- 0957168 Joris Verhagen
- 0960769 Ineke Kil
- 0959019 Bjorn van Rixtel
Problem definition
More than 1.2 million people in the Netherlands have diabetes. That is about one out of every fourteen people and everyday about 169 people are newly diagnosed. [1] Although it is treatable with medicines or insulin, it is a chronically disease you are confronted with everyday. Depending on the type of diabetes, people have to insert insulin three times a day, around every meal. A diabetes patient always has to keep track of the number of grams of carbohydrates that have been consumed. On the basis of a formula, it can be calculated how much insulin is needed to keep ones blood sugar level on healthy terms. However, this is a standard formula for everyone and throughout your own life it also differs how much extra insulin is needed for every gram of carbohydrates. This formula should actually differ for every person and change from time to time. It is also quite some work to always keep track of the food or carbohydrates you have eaten, especially for a plate full of hot steaming food...
State of the Art
Artificial Intelligence in Diabetes
Currently the most known AI approach in diabetes is the approach from PEPPER [8] (patient empowerment through predictive personalized decision support). PEPPER is a newly launched three-year research project, funded by the EU Horizon 2020 Framework. It’s goal is to create a portable personalized decision support system to empower individuals on insulin therapy to self-manage their condition. PEPPER employs CaseBased Reasoning to advise about insulin bolus doses, drawing on various sources of physiological, lifestyle, environmental and social data. It also uses a Model-Based Reasoning approach to maximise users’ safety.
Case-Based Reasoning (CBR) is a consolidated artificial intelligence technique, extensively applied in medicine, that tries to solve newly encountered problems by applying solutions learned from similar problems encountered in the past.
The system will be integrated with an unobtrusive insulin patch pump and has a patient-centric development approach in order to improve patient self-efficacy and adherence to treatment.
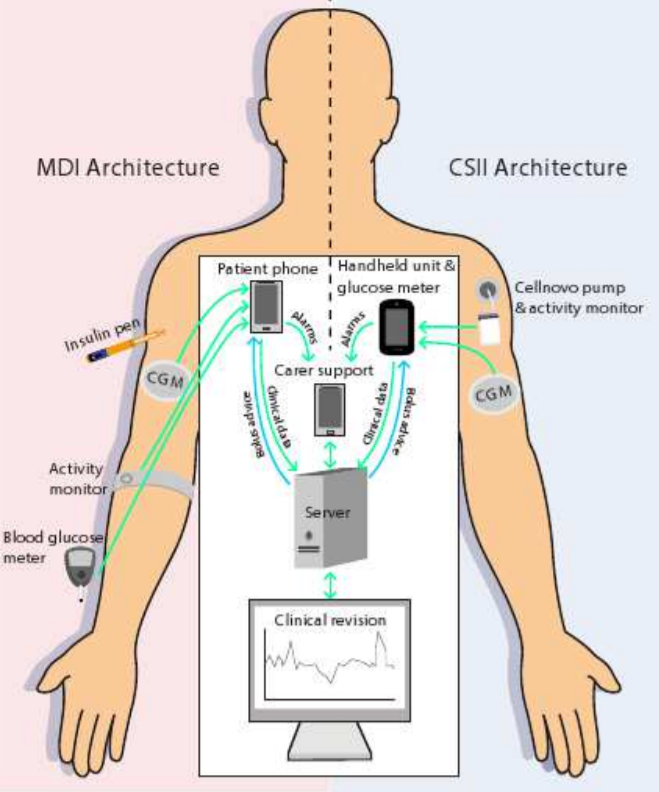
In the figure below, two architectures can be seen. These methods principally don’t differ quite much. In a nut shell, the PEPPER systems provide a portable personalised decision support system for insulin dosing that combines data from multiple sources such as body-worn sensors and manual inputs. These body-worn sensors for instance are the activity monitors that can be seen in the picture above. The manual inputs are given to the system by making use of a phone or handheld and consist of personal inputs like for instance the time someone sported, the amount and kind of food someone ate or the whether or not consumption of alcohol. The CaseBased Reasoning module is designed to provide a personalised insulin dose which adapts over time.
Our Solution
All-in-one Userfriendly Diabetes Application
As can be read in the paragraph about the state of the art of this topic, the user still needs to do a lot to get the correct insulin output. For instance, the user has to wear some sensors like the activity monitor all day long and they still have to fill in some details about their daily behavior on their smartphones. Altogether, this method requires still a lot of the users what’s very unpleasant for them of course. Therefore we found a new solution, which has to make it easier for diabetes patients to get a suited personal insulin dose.
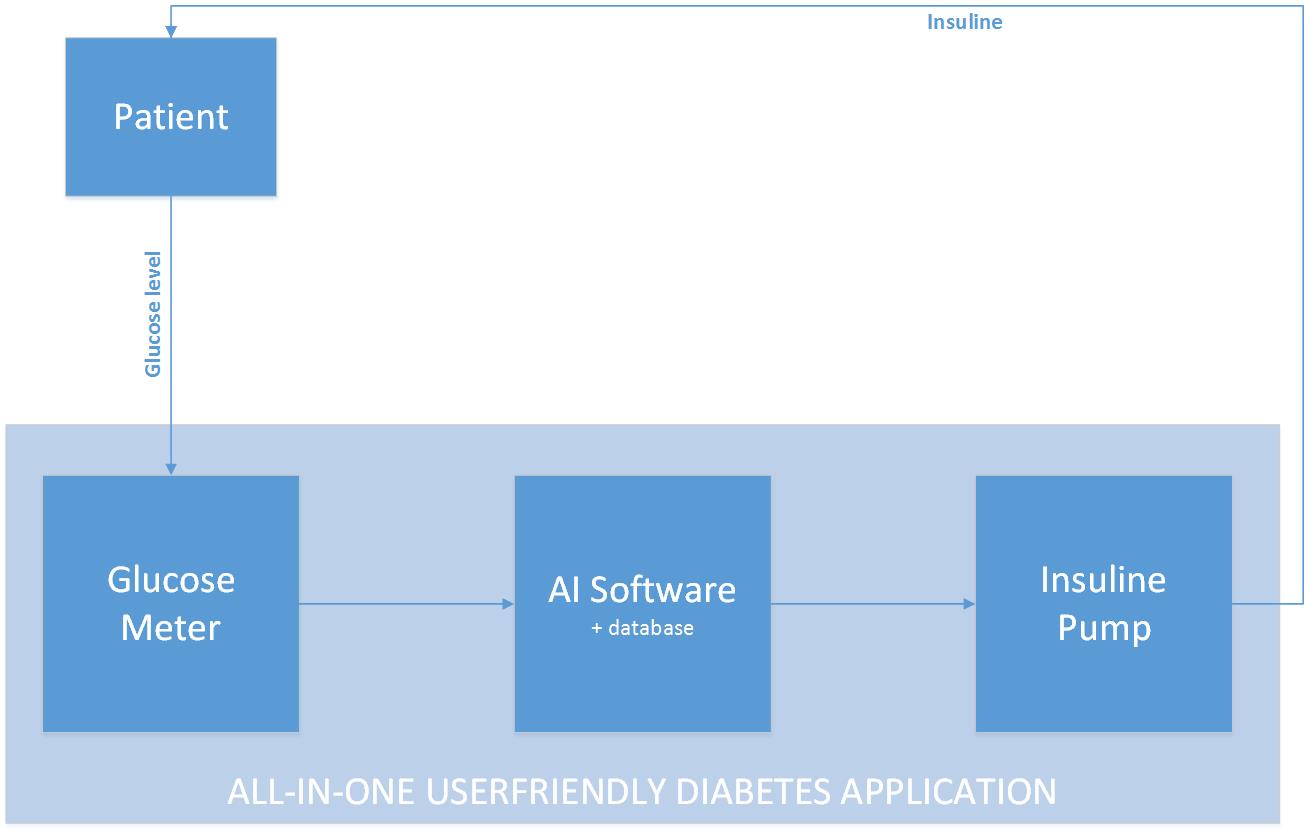
Our concept idea can be visualized in the figure below. We want to create an all-in-one userfriendly diabetes application which enables a patient to get a right personalized dose of insulin in an easy way. Instead of monitoring a patient all day long, we want to develop an algorithm that is based on and learns from the feedback it gets.
Because of most people have a kind of a fixed day rhythm, an algorithm could recognize this after some time and adapt to this. The adaption is based on the feedback that the software will get. This is the glucose level of the blood, after a period when insulin was injected. The glucose values always have to be in a certain range. And by coupling the data from the amount of insulin injected and the glucose level afterwards, the algorithm could learn to “know” somebody, because not everyone reacts the same on a certain amount of injected insulin. By receiving feedback over a longer period, the algorithm learns to recognize someone’s behavior too. Because of most people have a weekly fixed day schedule and for instance mostly sport on Monday, the algorithm could learn by making use of the feedback it will always need to give more insulin on Monday.
However, there are some exceptions. Surely not every day is the same in every week, but still some behavioral patterns keep existing. But always there might be some days that are totally different from the others. Therefore the “activity monitor” comes to live. This could be in the form of a ‘+’ and ‘-‘ button for if the patient surely knows by itself he or she definitely will need more or less insulin then the algorithm normally will give.
This piece of artificial intelligent learning software, has the possibility to be for instance implemented in an insulin pump, which is something a patient definitely has to wear all the time. Because of the fact that the algorithm learns to know it’s patient by receiving feedback in the form of training data it will calculate a personalized and therefore better and healthier dose of insulin that has to be given by the pump. The only thing the user has to do is measure it’s glucose level and eventually indicate a deviate day. So this isn’t a big change for the user, but this new software may be a big and better change towards his or her healthcare!
To test the developed software we’ll make a smartphone app and “train” it with the year data of one of our group members. For us it is not possible to implement this for instance in a real insulin pump, but by making the app, we could have I look if it works or not. Furthermore we could investigate more in opportunities and possibility’s the implement our solution in real live existing and user friendly systems.
USE Aspects
For evaluating and comparing several solutions to the problem stated above, the following three key actors play an important role: the user, the society and the enterprise. A good solution is always evaluated upon its relevance to both the users and the society, and its contribution to a viable revenu model for the enterprises. Each of these three individual actors have their own interests and concerns when it comes to derriving an appropriate solution, and it is of utmost importance to study those interests.
User Both our problem and our solution are aimed at a very specific user: patiënts with type 1 diabetes. Ofcourse, the solution will reach a wider target than just that. People with type 2 diabetes or even people generally interested in improving their health by watching their blood sugar levels. In the users interest are several design guidelines, such as easy useage, privacy, accuracy/usefullness of the advice given, etcetera.
Society The societal benefit will mostly consist of reduced costs in the healthcare industry. Furthermore it could also be of interest too some semi-government institutions such as "Het Voedingscentrum". Their interest could lie in the accuracy and reliability of the advice or who is to be held accountable for bad advice,etcetera.
Enterprise Now a days
Idea
Goal
Our goal is to develop a diabetes application that helps a patient with the problems mentioned above. The most important part of the application is an algorithm that learns from the user and optimizes the formula accordingly. At the start of using the application you have to fill in what you have eaten on a day and your blood glucose level for a longer period. From this information the algorithm learns what your blood glucose level will be depending only on what you have eaten on a day. This information will be used to let the user know how much insulin must be inserted. Additionally, the input of what you have eaten should be simple. This can be done with text or a picture. The program also remembers what you often eat at a certain time of the day, so if you want to fill in what you have eaten you receive suggestions of specific meals or snacks. As extra help the application can be linked to a kitchen scale with Bluetooth. If you scoop up dinner on your plate while it is on the scale the application immediately knows how much grams of a certain kind of food you are going to eat. What the food that the user is weighing is, can be selected on the smartphone application.
Target group
The current state of the treatment
Diabetes patient try to regulate their blood sugar with insulin. For this they use a basal insulin replacement and separate carbohydrate covering and correcting insulin replacement. For patients that are treated with insulin pens these insulin replacements are slow working insulin, insulin that is absorbed during a period of 24 hours, and fast working insulin that is used for correcting and covering carbohydrates in food and drinks. For pump users the situation is a bit different, the basal replacement is fast working insulin that is delivered to the body in small doses over the whole day, and a (usually) bigger dose of fast working insulin distributed over a few hours for carbohydrate covering and correcting.
Currently the carbohydrate covering and correcting dosages are calculated by a linear formula, with as inputs the amount of consumed carbohydrates and the current blood sugar value. The food coverage part of the insulin dose, is an insulin to carbohydrate ratio. This ratio represents how many grams of carbohydrate are covered by 1 unit of insulin. The correcting part of the dose is how much one unit of fast working insulin will drop the blood sugar. Both factors differ from person to person, and can also vary for one person over time, as the reaction to insulin is affected by stress, activity level and posture.
The final calculation of a dose of insulin is as follows:
#Units= (Grams of carbohydrates)/(CarboHydrates disposed per unit) + (Current blood sugar-Target blood sugar)/(Drop in blood sugar by 1 unit insulin)
This formula is built into most blood sugar meters and insulin pumps. But as the reaction to insulin can change over time, this formula may result into wrong dosages, resulting in an unstable blood sugar level. So new factors have to be “guessed” to correct the formula. We want to research if it is possible to automatically adapt the formula with data from the user. This can be done by estimating new factors over time, or a whole new method of determining the dosage, using techniques from the field of Artificial Intelligence.
This is especially useful for kids and young adults, as their bodies and activities are changing over time.
Investigation in the existing research in formula optimalization
Proposed Ideas
Some ideas we have for calculating the dosage are:
- Linear regression on data patient
- Other forms of regression on data patient
- Neural network that tries to learn and predict outcome of insulin dosage based on previous data of the patient.
User Data
- Blood sugar values
- Activity level
- Amount of carbohydrates
- Previous doses of insulin
Existing Measuring Techniques
Test App for the software and formula
Userfriendly
Week planning
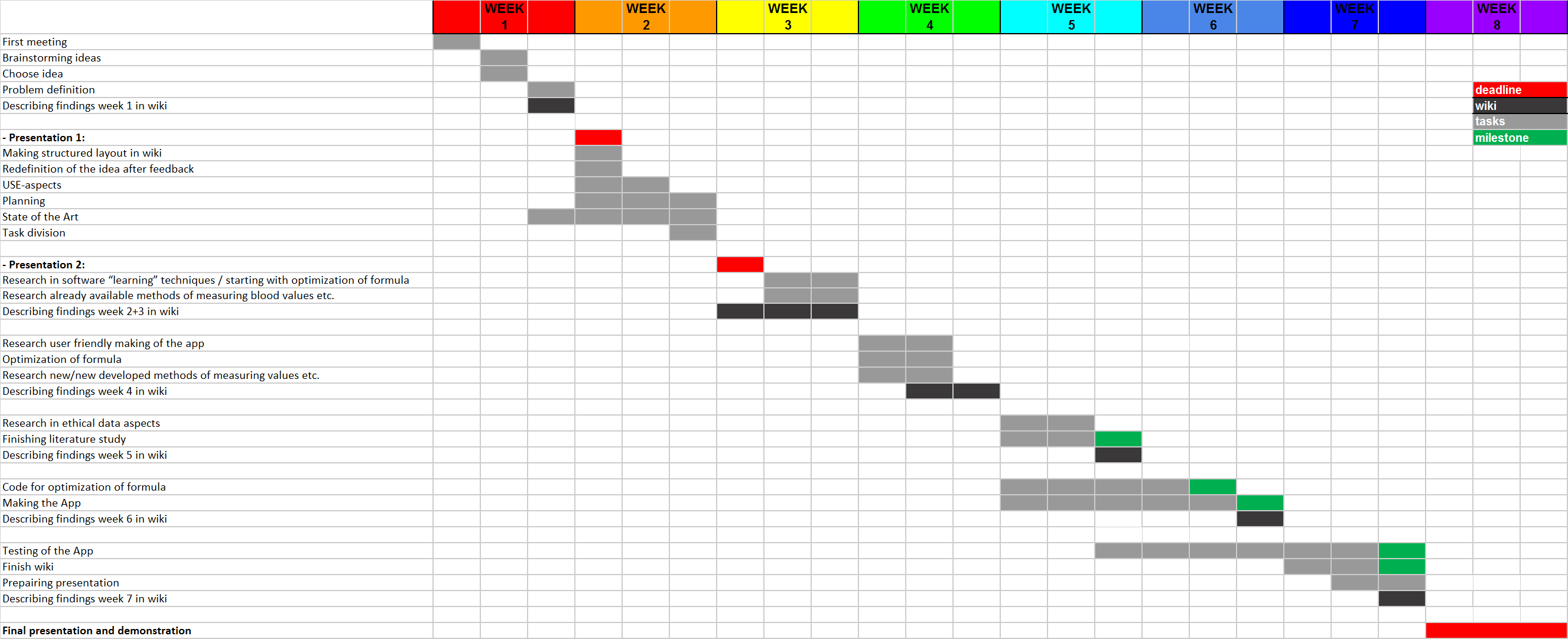
Week 1:
- First meeting
- Brainstorming ideas
- Chose idea
- Problem definition
Week 2:
- Presentation 1:
o Chosen project challenge
- USE-aspects
- Planning
- State of the Art
- Task division
- Redefinition of the idea after feedback
- Describing findings week 1 in wiki
- Making structured layout in wiki
Week 3:
- Presentation 2:
o Plan of execution for the chosen project challenge
§ Definition of tasks
§ Deliverables
§ Milestones
§ Gantt chart
§ Resource allocation
- Resource in software “learning” techniques / starting with optimization of formula
- Research already available methods of measuring blood values etc.
- Describing findings week 2+3 in wiki
Week 4
- Optimization of formula
- Research new/new developed methods of measuring values etc. (in which our software possibly could be implemented)
- Describing findings week 4 in wiki
Week 5
- Research in ethical data aspects
- Code for optimization of formula [milestone]
- Describing findings week 5 in wiki
Week 6
- Start at making of the App
- Describing findings week 6 in wiki
Week 7
- Making the App
- Research user friendly making of the app
- Start at conclusion and recommendation
- Describing findings week 7 in wiki
Week 8
- Finish wiki [milestone]
- Finishing the App [milestone]
- Final presentation and demonstration
Case scenario
Users
Current solutions to the problem
Most patients today use the manual calculation method for determining the necessary insulin dose. This is a time-consuming and, mainly in the beginning, a complex process, since 40-50% of the total daily insuline dose is to replace insulin overnight, when you are faston or between meals and the other 50-60% is for carbohydrate coverage and high blood sugar. [3]
Many of the diabetes patients find this process less than ideal. The weight and the amount of carbohydrates per certain amount of all the foods that the patient is going to eat needs to be known to calculate an insulin dose. There are, however, apps that take away some of the calculations from the patient. These apps will be explained in 'State of the art'.
State of the art
Two existing technologies to ease the insulin dose calculations are apps and insulin pumps. These technologies will be explained in this chapter.
Apps:
Current insulin calculating apps work on simple calculations. In general, the user enters their current blood sugar level and the amount of carbohydrates that the user is going to consume. The app will calculate the necessary dose of insulin for the user. Almost every application has the feature of saving the calculated insulin dose to a log. This log is able to provide insight over the user's glucose level throughout the day [4]. The app which is regarded by its users as the most useful on AppCrawlr, is the $1.99 Glucose Companion app. Since this is regarded as most useful, it can also be regarded as state-of-the-art concerning diabetes applications. The special feature that this app offers is that it can keep a better track on the glucose levels and insulin doses and that it gives advice on certain diet options [5]
Insulin pumps:
An insulin pump, which is shown on the image below, is connected to the patient by a cathether placed under the skin. When the pump is connected, the patient can receive short-acting insulin. The patient can increase the dose with buttons on the pump itself. This is to compensate the carbohydrates from a meal. The pump can also treat high blood glucose levels by taking a bolus. This is also determined by the patient him- or herself. It is important to note that the pump does not automatically correct the dose for everthing that the patient undergoes (such as meals and activities). The dose calculation is still done by the patient itself. The insulin pump has some advantages and disadvantages with respect to normally getting your insulin. These are stated below:
Advantages
The website from the American Diabetus Society gives multiple advantages [6]. The main one is that the patient does not have to bother with individual insulin injections which can really interfere with the patients life. Other advantages are:
- Insulin pumps deliver insulin more accurately than injections do.
- Insulin pumps result in fewer large swings in your blood glucose level since the doses are applied in a constant way.
- Insulin pumps allows the patient to be flexible about when and what he or she eats since ????????
- Insulin pumps allows the patient to excercise without having to eat large amounts of carbohydrates.
Disadvantages
The insulin pump does come with some disadvantages however. These are also given by the American Diabetus Society [7].
- Insulin pumps can cause weight gain to the patient.
- Insulin pumps can be expensive (and certainly are when they are not included in the patient's insurance).
- The insulin pump is connected to the patient most of the time. This can be bothersome.
In short, although the insulin pump solves some of the problems for the patient, it does not solve the biggest one which is manually increasing the insulin dose.
File:21235 large Insulin-Pump.jpg
Sources
[1] https://www.diabetesfonds.nl/home
[2] http://www.avdweb.nl/arduino/hardware-interfacing/scale-interface.html
[4] http://appcrawlr.com/ios-apps/best-apps-insulin-calculator
[5] http://appcrawlr.com/ios/glucose-companion#authors-description
[8] http://www.ecai2016.org/content/uploads/2016/08/W7-AID-2016.pdf