PRE2023 3 Group5
Medical Robot
Group Members
| Name | Student ID | Department |
|---|---|---|
| Yuting Dong | 1546104 | Computer Science |
| Jie Liu | 1799525 | Computer Science |
| Zhiyang Zhang | 1841734 | Mechanical Engineering |
| Samir Saidi | 1548735 | Computer Science |
| Feiyang Yan | 1812076 | Computer Science |
| Nikola Mitsev | 1679759 | Computer Science |
Introduction
Problem Statement
Nowadays, there is an increasing amount of people who are sick, elderly or have disabilities which prevent them from taking care of themselves. For some people, travelling constantly to hospitals or clinics for a regular health test is always a struggle. The caretaker is thus a necessary role that must be present in our society to ensure the well-being and quality of life for individuals facing these challenges. However, contemporary families often face the dual dilemma of struggling to allocate time for caregiving responsibilities and encountering financial barriers that hinder their ability to engage professional caregivers. Consequently, a significant portion of the population in need is left without the essential care they require.
Objectives
Considering the current situation that the society is facing regarding health care, we've decided to design a home robot with a primary focus on remote healthcare that is easily accessible to individuals. The robot should be able to cover the basic needs of the patients, such as dispensing pills, conducting tests and establishing connections with healthcare institutes. The main goal of the robot is to bridge the gap between the patients and their caregivers or doctors. On one hand, the robot closely monitors the individual's health on a daily basis and ensure that the necessary health-related tasks are performed seamlessly. On the other hand, it acts as a channel for communication, facilitating regular updates and consultations with healthcare professionals.
The design of the robot should cover these features:
1. Customizable Functionality: We recognize that the needs for healthcare can vary greatly from one individual to another and our product is designed to cater to a diverse range of users. Therefore, our robot should be highly customizable, allowing users to tailor its functions to their specific requirements. The functions may include but not limited to dispensing medication, temperature monitoring, blood pressure test, etc.
2. Health Monitoring: The robot should be able to analyze basic medical conditions based on test results of the user and continuously monitor the vital signs, such as blood pressure, temperature, and blood glucose levels. The analysis data will be stored for further reference. Relevant health suggestions will be available from time to time to keep both the user and the caregiver informed about health conditions.
3. Communication bridge: The robot will facilitate communication between users, healthcare professionals, and caregivers. It should be able to send test results directly to health institutes, help users schedule appointments, and even assist in ordering medications.
4. User-Friendly Interface: The robot should be equipped with a user-friendly interface, considering the potential challenges that elderly and disabled individuals might face when operating the device. For example, a touchscreen and voice-activated controls are preferred.
State-of-the-art
Literature review
Dementia is a syndrome primarily defined by the deterioration of one's cognitive ability beyond what would be expected of biological aging, affecting one's learning and memory, attention, executive function, language, motor perception and social function (Shin, 2022[1]). As a result, this condition can make it difficult, or even impossible, for one with dementia to live independently, often requiring the assistance of a professional caretaker or an informal caretaker (family) in the later stages of the condition. As one would expect, this puts strain on a country's healthcare system, both in terms of personnel and finances; in 2023, the WHO (World Health Organization) estimated that 55 million people worldwide were living with dementia, and they expect this number to nearly triple to 155 million by 2050 (World Health Organization, 2023[2]). The WHO (2023[2]) additionally estimated that the cost of dementia care in 2019 amounted to $1.9 trillion. That is why there is currently a growing demand for robotic caretakers, with a wide range of assistive functionalities, for example, keeping the patient company, reminding them of various tasks, or calling emergency services or other trusted people when the need arises. In 2023, the market for elderly care assistive robots was valued at $2.5 billion, and was projected to grow at a rate of 12.4% to $8.1 billion by 2033 (Saha, 2023[3]).
The increasing aging population faces many challenges, but people with dementia in particular, due to their deteriorating cognitive function, often have difficulties identifying fall risks and can accidentally trip and fall over objects in their home (Canadian Institute for Health Information, n.d.[4], Dementia UK, n.d.[5], Fernando et al., 2017[6]) It is well known that falling is a high danger to elderly people, presenting risk of injury, hospitalization, and can even lead to death. In fact, such accidental falls are one of the leading causes of hospitalization and death in elderly populations (Stinchcombe et al., 2014[7], Kakara, 2023[8], Centers for Disease Control and Prevention, n.d.[9]). Moreover, there are challenges involving emergency response coordination, which can lead to delays in the patient being given treatment after falling (Hesselink et al., 2019[10]). Therefore, there is certainly a need to protect elderly people living alone at home from such risks, both via proactive measures involving identifying fall risks and notifying the user (and possibly removing fall risks autonomously, with a sufficiently advanced robot design), but also, by notifying emergency services and the caretaker(s) of the patient if they have fallen and need assistance or hospital care. Since it has been shown that slower EMS responses is associated with increased mortality (Adeyemi et al., 2023[11]), a robot capable of preventing falls would help relieve some of the burden on the healthcare system, caretaker(s), and allow the patient to live more independently.
Naturally, a user-centered approach must be taken when designing solutions, with focus on making the human-computer interaction as user-friendly as possible. In fact, one of the major challenge impeding the large-scale adoption of elderly care social robots into care homes and in cases of independent living is the complexity of many current robots causing more trouble for caregivers and patients rather than relieving them of it; according to Koh (2021[12]), the multiple visual, auditory and tactile interaction of social robots presents challenges and confusion for people with dementia. This makes the focus on user-friendly HCI even more important. Part of this disconnect between the expected and actual relief of burden seems to stem from how current solutions focus on too many things at once and attempt to make a general care robot, rather than specializing in one area. Furthermore, having a complex user interface is a pitfall, as previously discussed, increased complexity creates added confusion for people living with dementia. Despite these pitfalls and challenges, many case studies and state-of-the-art reviews have shown the effectiveness of a variety of elderly care robots (Carros et al., 2020[13], Raß et al., 2023[14], D'Onofrio et al., 2017[15], Søraa et al., 2023[16], Johnson et al. 2014[17], Vercelli et al., 2018[18]). Therefore, by identifying the needs of our user and the stakeholders, it should be possible to create a simple-to-use, yet effective, robot that addresses our problem.
Due to gaps in the literature, existing solutions can also fall short. As shown below, many solutions ...
As such, there are many opportunities for improvement, and our robot should aim to be such an improvement. ...
Despite the evidence supporting the effectiveness of such robotics in the field of elderly care, papers have also shown its benefits to be overstated. For example, Broekens et al. (2009[19]) showed that although there is some evidence that companion type robots have positive effects in healthcare for elderly people with respect to at least mood, loneliness and social connections with others, the strength of this evidence is limited, due to a variety of factors.
As a result of the above, we highlight the need for our proposed solution, because ...
Current products
USE analysis
The design of the robot must be taken in coordination with a variety of stakeholders, and not just our target user (who we have defined to be elderly people with mild memory loss due to dementia, living alone at home). Examples of such stakeholders are: formal/professional caregivers, informal caregivers (such as family members), and doctors. Each of these stakeholders have different needs and priorities regarding the care of our target user, and thus, will have different perspectives that will ultimately influence how we design our robot.
Users
Society
Enterprise
Ethical analysis
Approach
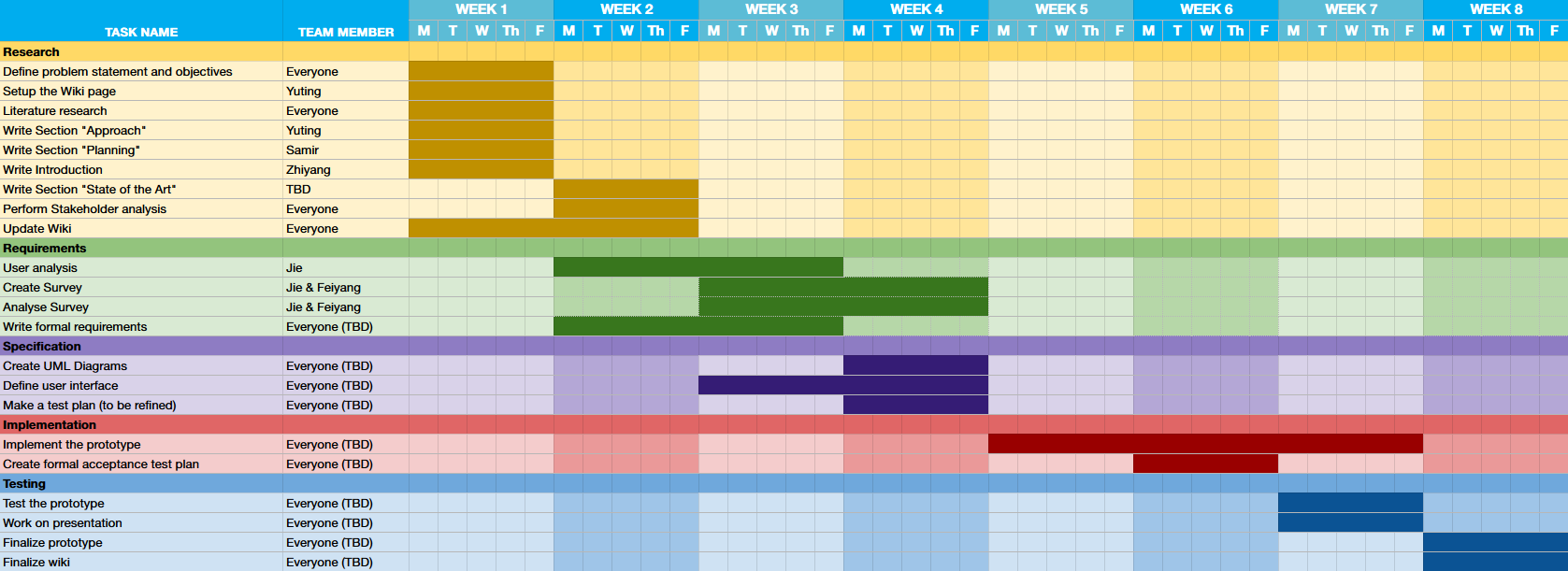
In order to reach the objectives, we split the project into 5 stages. The five stages are distributed into 8 weeks with some overlaps. Everyone in the team is responsible for some tasks in these stages.
- Research stage: In week 1 and 2, we mainly focus on the formulation of problem statements, objectives, and research. We first need to make a plan for the project. The direction of this project is fixed by defining the problem statement and objectives. Doing literature research helps us to gather information of state-of-the-art, the advantages and limitations of current solutions.
- Requirements stage: From week 2 to week 4 we will do user analysis to further determine the goal and requirements of our product. We will collect information about user needs by surveys and interviews. The surveys and interviews can contain information found in the research stage. For example, how does the user think about the current solution, what improvements can be made.
- Specification stage: This stage is in week 3 and 4, in which we create the specification of our product using techniques such as UML diagrams and drawing user interface. From the user analysis and the research, we can create the specification in more detail. After this, a test plan will be made so that the product can be tested to see whether it meets the requirements and the specification.
- Implementation stage: The prototype of our product will be implemented in this stage from week 5 to week 7. We plan to only create the digital part of the product due to time constraints. Also, a more formal test plan will be constructed for later use.
- Testing stage: In week 7 and 8, the prototype will be tested by the test plan and we can examine whether the product reaches our goal and solves the problem. The finalization on the prototype, presentation and wiki page will be done in this stage.
Planning
We created a plan for the development process of our product based off of the previously described approach. This plan is shown in the Gantt chart below:
Task Division
We subdivided the tasks amongst ourselves as follows:
| Research | Requirements | Specification | Implementation | Testing | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Task | Group member | Task | Group member | Task | Group member | Task | Group member | Task | Group member | ||||
| Define problem statement and objectives | Everyone | User Analysis | Jie | Create UML Diagrams | Everyone (TBD) | Implement the prototype | Everyone (TBD) | Test the prototype | Everyone (TBD) | ||||
| Setup the Wiki page | Yuting | Create Survey | Jie & Feiyang | Define user interface | Everyone (TBD) | Create formal acceptance test plan | Everyone (TBD) | Work on presentation | Everyone (TBD) | ||||
| Literature research | Everyone | Analyse Survey | Jie & Feiyang | Make a test plan | Everyone (TBD) | Finalize prototype | Everyone (TBD) | ||||||
| Write Section "Approach" | Yuting | Write Formal Requirements | Everyone (TBD) | Finalize wiki | Everyone (TBD) | ||||||||
| Write Section "Planning" | Samir | ||||||||||||
| Write Introduction | Zhiyang | ||||||||||||
| Write Section "State of the Art" | Samir & Nikola | ||||||||||||
| Perform Stakeholder Analysis | Everyone | ||||||||||||
| Update Wiki | Everyone | ||||||||||||
Milestones
By the end of Week 1 we should have a solid plan for what we want to make, a brief inventory on the current literature, and a broad overview of the development steps required to make our product.
By the end of Week 3 we should have analysed the needs of our users and stakeholders, formalized these needs as requirements according to the MoSCoW method, and have a clear state-of-the-art.
By the end of Week 4 we should have specified the requirements as UML diagrams, blueprints, etc., created a basic user interface, and created an informal test plan.
By the end of Week 6 we should have created a formal acceptance test plan.
By the end of Week 7 we should have finished the implementation of our product's prototype.
By the end of Week 8 we should have tested the product according to the acceptance test plan, finished the presentation, finalized the prototype, and finalized our report.
Deliverables
The final product will be a robot that is programmed to detect when a user falls and alerts emergency services if they do. Furthermore, we would like it to be capable of identifying fall risks and alerting the user of them, but we do not yet know if this can also be done within the course timeframe.
Logbook
Week 1
| Name | Total hours | Tasks |
|---|---|---|
| Yuting | 6 | Introduction lecture (1), meeting (1.5), Approach section (1.5), literature study (2) |
| Jie | ||
| Zhiyang | 6 | Introduction lecture (1), meeting (1.5), Introduction section (1.5), literature study (2) |
| Samir | 6 | Introduction lecture (1), meeting (1.5), Gantt chart (1), Planning section (1.5), Literature research (1) |
| Feiyang | 5 | Introduction lecture (1), meeting (1.5), literature study (2.5) |
| Nikola |
Week 2
| Name | Total hours | Tasks |
|---|---|---|
| Yuting | ||
| Jie | ||
| Zhiyang | ||
| Samir | 7.5 | Feedback session + meeting (1.5), State of the art section (6) |
| Feiyang | ||
| Nikola |
Week 3
| Name | Total hours | Tasks |
|---|---|---|
| Yuting | ||
| Jie | ||
| Zhiyang | ||
| Samir | ||
| Feiyang | ||
| Nikola |
Week 4
| Name | Total hours | Tasks |
|---|---|---|
| Yuting | ||
| Jie | ||
| Zhiyang | ||
| Samir | ||
| Feiyang | ||
| Nikola |
Week 5
| Name | Total hours | Tasks |
|---|---|---|
| Yuting | ||
| Jie | ||
| Zhiyang | ||
| Samir | ||
| Feiyang | ||
| Nikola |
Week 6
| Name | Total hours | Tasks |
|---|---|---|
| Yuting | ||
| Jie | ||
| Zhiyang | ||
| Samir | ||
| Feiyang | ||
| Nikola |
Week 7
| Name | Total hours | Tasks |
|---|---|---|
| Yuting | ||
| Jie | ||
| Zhiyang | ||
| Samir | ||
| Feiyang | ||
| Nikola |
Week 8
| Name | Total hours | Tasks |
|---|---|---|
| Yuting | ||
| Jie | ||
| Zhiyang | ||
| Samir | ||
| Feiyang | ||
| Nikola |
Literature study
- (Existing product regarding robot that dispensing pills) The robot, managed via an app, securely stores and dispenses medication, provides verbal reminders, and can alert caregivers if doses are missed. It features facial recognition and motion detection to ensure the right person receives the medication. The device complies with patient privacy laws and is positioned as a health care solution amid the growing trend of remote health care technology. Rosen, A. (2019), This robot makes sure you remember to take your pills. CUTTING EDGE | MAGAZINE, available at: https://www.bostonglobe.com/magazine/2019/03/29/this-robot-makes-sure-you-remember-take-your-pills/.
- (Introducing a new technology and a new way of remote health care) Telemedicine, an emerging technology, enables remote medical consultations through video conferencing or digital imaging systems, fostering coordination and collaboration in diagnosing and treating diseases. A three-tier pervasive telemedicine system utilizes a wireless body area network (WBAN) for continuous healthcare monitoring, with users obtaining vital signals in Tier 1 and transmitting them to healthcare providers in Tier 3 through personal gateways (Tier 2), such as smartphones. Tiers 1 and 2 serve as the client side, providing mobile health (mHealth) services, while Tier 3 represents the server side. Shuwandy, M. L., Zaidan, B. B., Zaidan, A. A., & Albahri, A. S. (2019). Sensor-based mHealth authentication for real-time remote healthcare monitoring system: A multilayer systematic review. Journal of medical systems, 43, 1-30.
- (Potential challenges raised by telemonitoring technology) Issues include the absence of suitable sensors, concerns about system size and weight, identification of invalid data, battery life, bandwidth, network coverage, and data transmission costs. Adoption challenges are highlighted, such as privacy concerns and potential insurance-related issues. Cultural adjustments in healthcare organizations and the need for new data analysis methods are also mentioned. Nangalia, V., Prytherch, D. R., & Smith, G. B. (2010). Health technology assessment review: Remote monitoring of vital signs-current status and future challenges. Critical Care, 14, 1-8.
- (Possible design ideas and the drawbacks in remote health-care technology) Several related work and design techniques have been presented. Zhou, B., Wu, K., Lv, P., Wang, J., Chen, G., Ji, B.& Liu, S. (2018). A new remote health-care system based on moving robot intended for the elderly at home. Journal of healthcare engineering, 2018. Available at: https://www.hindawi.com/journals/jhe/2018/4949863/.
- (Ethical concerns regarding telehealth) The paper discusses challenges related to integrating telehealth into healthcare systems. Concerns about data protection and privacy are raised due to increased access to sensitive patient data. Ethical issues arise regarding patient autonomy and the potential substitution of physical presence in healthcare. Botrugno, C. (2019). Towards an ethics for telehealth. Nursing ethics, 26(2), 357-367.
- (Collaborative Robot for Remote Dementia Care in Home) This paper shows a teleoperation of a remote care robot at home. This robot is designed for elderly people with dementia. Care givers can use this robot to provide care remotely. They can monitor the patient via robot vision, and control the robot arm via motion tracking. For instance, they can grab medicine and pills for the patient. https://ieeexplore.ieee.org/abstract/document/9116811/authors#authors
- (Human-Robot Interaction with the Elderly) Some researchers conducted an experiment of replacing a human care giver with a humanoid care robot for 10 weeks. The conclusion is that the elderly are willing to interact with the robot, but they think that the robot cannot replace a human care giver because of techniqual issues, lacking warmth, acceptance, and unexpected situations. https://dl.acm.org/doi/abs/10.1145/3313831.3376402
- (Patient Monitoring and Medicine Dispenser Robot) This robot is an assistive medical robot for doctors to take care of patients remotely. It combines the pill dispensing and patient monitoring. Doctors can set the prescription for patients. The robot will then remind patients to take pills at required time. It will at the same time recored the patient's temperature via infrared and store it in a database for further analysis. https://pubs.aip.org/aip/acp/article/2494/1/030004/2827068/Patient-monitoring-and-medicine-dispenser-robot
- (A design of a robotic system to dispense pills) This article introduces the algorithm of a automatic pill dispensing robot. It provides pills to the patient according to a schedule, and remind the patient with sound, light signals and text messages. The signals remain until the patient takes the pills and presses a button. If the patient does not take pills on time, the robot will contact the nurse. https://www.sciencedirect.com/science/article/pii/S0149291817302023
- (The Role of Healthcare Robots for Older People at Home) This paper discusses problems healthcare robots are facing and what solutions are there. We need to consider the acceptance of healthcare robots by the elderly and privacy issues when designing the robot. The elderly at home can face many different problems. For example, physical problems, mental issues, dimentia and so on. Different robotic solutions need to be considered to solve these problems. https://link.springer.com/article/10.1007/s12369-014-0242-2
- Robots in elderly care can be used to provide companionship and improve quality of life of elderly people affected with cognitive impairment/dementia, and can assist them in independent everyday living, by monitoring their health and monitoring the environment to detect dangerous situations, like fall risks, and can be used to remind them of medicines, appointments, tasks, etc. Vercelli, A., Rainero, I., Ciferri, L., Boido, M., & Pirri, F. (2018). Robots in elderly care. DigitCult-Scientific Journal on Digital Cultures, 2(2), 37-50. https://digitcult.lim.di.unimi.it/index.php/dc/article/view/54
- Yang et al. identified 10 grand challenges in robotics in 2018: New materials and fabrication schemes, biohybrid and bioinspired robots, power and energy, robot swarms, navigation and exploration, AI for robotics, brain-computer interfaces, social interaction, medical robotics, and robot ethics and security. Of particular interest to us is: navigation and exploration, AI for robotics, social interaction, and medical robotics. Yang, Guang-Zhong & Bellingham, Jim & Dupont, Pierre & Fischer, Peer & Floridi, Luciano & Full, Robert & Jacobstein, Neil & Kumar, Vijay & McNutt, Marcia & Merrifield, Robert & Nelson, Brad & Scassellati, Brian & Taddeo, Mariarosaria & Taylor, Russell & Veloso, Manuela & Wang, Zhong & Wood, Robert. (2018). The Grand Challenges of Science Robotics. Science Robotics. 3. eaar7650. 10.1126/scirobotics.aar7650.
- A review of the literature on assistive social robots in elderly care by Broekens, Heerink and Marcel found that there is some evidence that companion type robots have positive effects in healthcare for elderly people with respect to at least mood, loneliness and social connections with others. However, the strength of this evidence is limited, since (a) most studies have been done in Japan, with (b) a limited set of companion robots, i.e., Aibo and Paro, and (c) research designs are not robust enough, usually not described in enough detail to repeat, and confounding causal variables cannot be excluded. However, the review concludes that it is still worthwhile to invest in research methods to better examine the efficacy of social robots in elderly care. Broekens, Joost & Heerink, Marcel & Rosendal, Henk. (2009). Assistive social robots in elderly care: A review. Gerontechnology. 8. 94-103. 10.4017/gt.2009.08.02.002.00.
- The KSERA (Knowledgeable SErvice Robots for Aging) project integrates smart home technology and a socially-assistive robot to extend independent living for elderly people, in particular those with COPD. The project achieved the goal of integrating smart home technology and socially-assistive robots to allow the extension of independent living for elderly people. The results showed that (1) the KSERA system and Nao robot are likable, (2) the attitude toward the Nao robot is highly correlated with the attitude toward the system, and (3) communication through a robot is preferred over interaction with the individual technical elements of a smart home. Johnson, D.O., Cuijpers, R.H., Juola, J.F. et al. Socially Assistive Robots: A Comprehensive Approach to Extending Independent Living. Int J of Soc Robotics 6, 195–211 (2014). https://doi.org/10.1007/s12369-013-0217-8
- Direct social robots could decrease loneliness by creating conversational opportunities and, as prior literature (Turkle, 2011) shows, even a sense of attachment, especially as they develop technologically in the future. Additionally, in a study where a humanoid robot Zora was piloted in elder care services, the care personnel noted that, unlike a human caregiver, the robot does not get tired, it always responds in a friendly way, and it repeats things over and over if needed. Furthermore, the robot does not take things personally (Melkas et al., 2020). Breazeal (2004) mentions that one of the advantages of social robots is that they do not have any “social baggage” and therefore do not judge. In addition, it may be less stigmatizing for an older person to receive care from a robot than from a human (Prieto-Flores et al., 2011). Jari Pirhonen, Elisa Tiilikainen, Satu Pekkarinen, Marjut Lemivaara, Helinä Melkas, Can robots tackle late-life loneliness? Scanning of future opportunities and challenges in assisted living facilities, Futures, Volume 124, 2020, https://doi.org/10.1016/j.futures.2020.102640.
- The use of SARs in mental health research is not yet widespread, new robots and programming are constantly changing, adapting, and expanding. The use of SARs in mental health research and mental health interventions is nascent and has thus far been restricted to specific populations with limited measurement and scope. There is an abundance of opportunity in this area for growth, expansion, and exploration to triangulate SARs usability and efficacy data as the next step in advancing this field. Scoglio A, Reilly E, Gorman J, Drebing C. Use of Social Robots in Mental Health and Well-Being Research: Systematic Review, J Med Internet Res 2019;21(7):e13322. URL: https://www.jmir.org/2019/7/e13322. DOI: 10.2196/13322
(Please use APA 7 for bibliography)
- ↑ Shin J. H. (2022). Dementia Epidemiology Fact Sheet 2022. Annals of rehabilitation medicine, 46(2), 53–59. https://doi.org/10.5535/arm.22027
- ↑ 2.0 2.1 World Health Organization. (2023). Dementia. https://www.who.int/news-room/fact-sheets/detail/dementia
- ↑ Saha, S. (2023). Eldercare Assistive Robots Market. https://www.futuremarketinsights.com/reports/eldercare-assistive-robots-market
- ↑ Canadian Institute for Health Information. (n.d.). Dementia and falls. https://www.cihi.ca/en/dementia-in-canada/spotlight-on-dementia-issues/dementia-and-falls
- ↑ Dementia UK. Dementia and falls. (n.d.). https://www.dementiauk.org/information-and-support/health-advice/dementia-and-falls/
- ↑ Fernando, E., Fraser, M., Hendriksen, J., Kim, C. H., & Muir-Hunter, S. W. (2017). Risk Factors Associated with Falls in Older Adults with Dementia: A Systematic Review. Physiotherapy Canada. Physiotherapie Canada, 69(2), 161–170. https://doi.org/10.3138/ptc.2016-14
- ↑ Stinchcombe, A., Kuran, N., & Powell, S. (2014). Report summary. Seniors' Falls in Canada: Second Report: key highlights. Chronic diseases and injuries in Canada, 34(2-3), 171–174.
- ↑ Kakara R., Bergen G., Burns E. & Stevens M. (2023). Nonfatal and Fatal Falls Among Adults Aged ≥ 65 Years — United States, 2020–2021. MMWR Morb Mortal Wkly Rep 2023;72:938–943. DOI: http://dx.doi.org/10.15585/mmwr.mm7235a1.
- ↑ Centers for Disease Control and Prevention. (n.d.). Older Adult Falls Data. https://www.cdc.gov/falls/data/index.html
- ↑ Hesselink, G., Sir, Ö., & Schoon, Y. (2019). Effectiveness of interventions to alleviate emergency department crowding by older adults: a systematic review. BMC Emergency Medicine, 19. https://repository.ubn.ru.nl/bitstream/handle/2066/215426/215426.pdf
- ↑ Adeyemi, O., DiMaggio, C., Grudzen, C., Allison, C., Allen, K. V., & Chodosh, J. (2023). Emergency Medical Service Response Times and Fatal Fall Injuries Among US Older Adults: Analysis of the 2015 – 2020 National Trauma Data Bank. medRxiv, https://doi.org/10.1101/2023.06.18.23291570
- ↑ Koh, W.Q., Felding, S.A., Budak, K.B., Toomey, E., & Casey, D. (2021). Barriers and facilitators to the implementation of social robots for older adults and people with dementia: a scoping review. BMC Geriatr 21, 351. https://doi.org/10.1186/s12877-021-02277-9
- ↑ Carros, F. & Meurer, J. & Löffler, D. & Unbehaun, D. & Matthies, S. & Koch, I. & Wieching, R. & Randall, D. & Hassenzahl, M. & Wulf, V. (2020). Exploring Human-Robot Interaction with the Elderly: Results from a Ten-Week Case Study in a Care Home. https://doi.org/10.1145/3313831.3376402.
- ↑ Raß, E., Unbehaun, D., Wulf, V., Lüssem, J., Eilers, H., Lenz, G., Tandler, J., Afzali, S., Eroğlu, B. (2023). Investigating the Potential and Impacts of Social Robots to Engage People with Advanced Dementia and their Caregivers: Early Insights from an Exploratory Ethnographic Study within a Protected Care Environment. 272-278. https://doi.org/10.1145/3594806.3594826.
- ↑ D'Onofrio, G., Sancarlo, D., Ricciardi, F., Panza, F., Seripa, D., Cavallo, F., Giuliani, F., & Greco, A. (2017). Information and Communication Technologies for the Activities of Daily Living in Older Patients with Dementia: A Systematic Review. Journal of Alzheimer's disease: JAD, 57(3), 927–935. https://doi.org/10.3233/JAD-161145
- ↑ Søraa, R.A., Tøndel, G., Kharas, M. & Serrano, J.A. (2023). What do Older Adults Want from Social Robots? A Qualitative Research Approach to Human-Robot Interaction (HRI) Studies. Int J of Soc Robotics 15, 411–424. https://doi.org/10.1007/s12369-022-00914-w
- ↑ Johnson, D.O., Cuijpers, R.H., Juola, J.F. et al. (2014). Socially Assistive Robots: A Comprehensive Approach to Extending Independent Living. Int J of Soc Robotics 6, 195–211. https://doi.org/10.1007/s12369-013-0217-8
- ↑ Vercelli, A., Rainero, I., Ciferri, L., Boido, M., & Pirri, F. (2018). Robots in elderly care. DigitCult-Scientific Journal on Digital Cultures, 2(2), 37-50. https://digitcult.lim.di.unimi.it/index.php/dc/article/view/54
- ↑ Broekens, J. & Heerink, M. & Rosendal, H. (2009). Assistive social robots in elderly care: A review. Gerontechnology. 8. 94-103. 10.4017/gt.2009.08.02.002.00.