PRE2019 3 Group18
Group Members
| Name | ID | Major | |
|---|---|---|---|
Planning
Meetings held on Mondays and Thursdays. Tasks specified in the table have to be completed before the given meeting.
KdB = Kasper, N = Nick, D = Davide, KM = Kamil, M = Milan
| Week | Monday (morning) | Thursday (afternoon) |
| 1 | -- | -- |
|---|---|---|
| 2 | ALL: Form a group, decide on the subject |
|
| 3 |
|
|
| 4 | ||
| 5 | ||
| 6 | ||
| 7 | ||
| 8 | ||
| 9 |
Subject
Problem statement
WHO, short for World Health Organization, published an article on 30 October 2018 named ‘Diabetes’ (REF1). The article stated some key facts about diabetes. For example, the number of people with diabetes changed from 108 million to 422 million in 34 years. This is a rather concerning number, especially with the fact that diabetes can be treated (note: not cured!) and its effects can be delayed or even avoided with the help of a medication, a healthy lifestyle; a healthy diet with good physical activity and with the help of proper, professional screening of the patient. Present-day these challenges can be tackled properly, but the USE-aspect still has a lot of improvements to undergo. Later in this section we will look more in depth into the USE-aspect of problems with current technology.
Diabetes is a well-known disease, but there is still a lot of ignorance about the disease. Diabetes is a disease which occurs when the amount of glucose in your blood is too high. Having too much glucose in your blood for a long period of time can cause health problems. Diabetes is a general name for the diseases, it defines severel types of diabetes. Although there is no cure for diabetes (yet), a person can manage their diabetes to stay healthy and will be safe from its fatal consequences.
A lot of people undergo constraints because of the disease and with the help of technology products will make lives easier for diabetes patients. Diabetes patients first of all need to take medicine, depending on their type of diabetes (REF2). Also, they have to follow a personal diet matching with their diabetes type (REF2). This is a very important step for the treatment of diabetes and it requires a lot of effort from the patient. The diet has to be very specific, healthy and available to the patient. Problems with a good diet for a patient could be that a person is allergic to certain food, the diet does not provide a complete diet with all necessary vitamins or the food itself is too expensive for the person or even not available to the patient in his current location. These are all some technical issues that can arise when focusing on a good diet. But also the USE-aspect of technology to help patients is a big part. The app has to be user friendly and clear for people to use it concisely and correctly. Wrong data or mere laziness due to the app being hard to understand is disadvantageous and could potentially be fatal to patients. That is why this is an important problem which needs to be solved.
REF1 : [1]
REF2: [2]
Objectives
- Researching the state-of-the-art on diabetes
- Researching the needs of a diabetic patient
- Creating an app to assist these people with their diet
Diabetes Millitus
Diabetes Millitus is a chronic illness related to high blood sugar levels for a long duration of time. High blood sugar, blood glucose, is generally caused by a lack of secretion of insulin or a deficiency in reacting to insulin. Insulin is a hormone secreted by the pancreas. It is secreted when high levels of glucose are present in the bloodstream. Insulin facilitates the intake of glucose from the bloodstream to a cell. Also, insulin initiates the process of storing excess glucose as glycogen. Glycogen is a long chain of glucose molecules, which is used as short-term energy storage in animals. Insulin strongly inhibits lipolysis. Lipolysis is the fragmentation of lipid triglycerides, fat, into glycerol and fatty acids.[3] Therefore, the main function of insulin is to signal cells to take sugars from the bloodstream to burn them or store them as fat, and to stop secretion of sugars and fatty acids from lipolysis. So abnormally low levels of insulin would cause hyperglycemia and diabetic ketoacidosis.
Generally Diabetes M. can be divided in three main categories.
Type 1 diabetes is linked to insufficient insulin production. The main cause is an autoimmune destruction of beta cells of the pancreas. Beta cells are a type of cell located in the pancreas which are responsible for the synthesis and secretion of both insulin and amylin. In North America only 0.3% to 0.4% of the population is affected. The majority of affected patients are children.[4]
Type 2 diabetes is linked to insulin resistance and also insulin secretion. Insulin resistance means that the cells do not react to a normal dose of insulin. In America 6.6% of the population is affected. Patients are mainly Middle-aged and obese. Severely obese children also develop type 2. CAUSE: Decreased sensitivity to insulin (mediated glucose uptake) and decrease in insulin secretion.[5]
SYMPTOMS AND SIGNS: Classic symptoms of DM are polyuria, polydipsia, and weight loss. In addition, patients with hyperglycemia often have blurred vision, increased food consumption (polyphagia), and generalized weakness.
For type 1 DMloses metabolic control (such as during infections or periods of noncompliance with therapy), symptoms of diabetic ketoacidosis occur.(Dizziness, nausea, vomit, coma and death)
Chronic complications of hyperglycemia include retinopathy and blindness, peripheral and autonomic neuropathies, glomerulosclerosis of the kidneys (with proteinuria, nephrotic syndrome, or end-stage renal failure), coronary and peripheral vascular disease, and reduced resistance to infections. Patients with DM often also sustain infected ulcerations of the feet, which may result in osteomyelitis and the need for amputation.
TREATMENT: DM types 1 and 2 are both treated with specialized diets, regular exercise, intensive foot and eye care, and medications. Type 1: If a patient has not had a pancreas transplant they need insuline medication. "Tight control" of blood glucose is a more effective treatment instead of a "relaxed" or conventional control. A thight control treatment is more effective in reducing eye, nerve and renal complications, but increases the chance of hypoglycemia by more than two times. Thight control is considered an intensive therapy since frequent daily blood glucose measurments are necessary in combination with at least three or more insuline administrations. Intensive therapy is a burden and patients must be persistent. Type 2: Can be controlled with diet, exercise and weight loss. Also use of types of hypoglycemic drugs. Some drugs increase insuline production from the pancreas.(sulfonylurea) While others increase sensitivity to insuline. (biguanides or thiazolidinediones) Or others which decrease the absorption of carbohydrates. (alpha-glucosidase inhibitors) Studies on terapies with tight control of blood glucose, for type 2 patients, have not proved a decrease in cardiovascular death, non-fatal stroke, or limb amputation. But they decrease: the risk of non-fatal heart attacks by 15%, the risk of progression of retinopathy and nephropathy and the incidence of peripheral neuropathy. Unfortunately, as mentioned before tight control increases the risk of hypoglicemia by 2.4 times.
Users
- People who have diabetes and could use assistance with their diet
The application we aim to develop has a clear group of users; diabetic patients. Approximately 1,2 million Dutch people have diabetes. There are two types of diabetic patients, called type 1 and type 2. About 90% of all diabetic patients are type 2 diabetics. For now, our focus is on the patients of type 1 diabetes, which is the more severe form. These people need a specific diet and have to regulate their blood sugar level by administering insulin. These patients will probably benefit from a wellmade application that can support them with their diet and blood sugar regulation. We will try to find out how these people can be best supported by an application, and what their needs are going to be. An interview with the patient-communication advisor of Diabeter Eindhoven, and diabetic patient type 1 herself, Wietske Wits, has been held. She has elaborated on the user needs she finds important.
The interview
The primary goal of this interview is to gather more information on the state-of-the-art of diabetes and the difficulties of diabetes. This is to investigate the ways that diabetes influences the lives of people, and where support is desired. This will shape a clear image of what users of the application we aim to develop want in this application. It is important to consider what types of help and support users request from the application, to develop something that will actually support the user in manners that are desired by the user.
At first, the interview was mostly about the influence of type 1 diabetes on the life of individuals with the disease. A few new insights were provided and some ideas to take into account as well. Then, when specifically asking about the posibilities of an application we received some decent ideas and suggestions for improvement of the applications and support in the state-of-the-art that is currently available for patients of type 1 diabetes. Here, a summary of the conversance and information we received is given:
Diabetes has influence on everything; it has been estimated that being diabetic adds about 150 decisions every single day. These decisions revolve mostly around stabilizing blood sugar levels, like when to add how much insulin, what to eat, wheter or not to work out. There are (at least) 42 factors that influence blood sugar levels, so many things have to be taken into account (think of hormonal cycle, emotions, stress and adrenaline). You can never take one day off, the difficulties are constant.
At the moment, the institute Diabeter only advises carb counting applications. There are many applications and a variety exists that is of good use, but there are improvements possible:
- Since the struggle of being a diabetic is 24/7, it would be welcome to have some humour or encouragement in the application. It could also be used to buck someone up a little, making them feel supported.
- Many applications exist, but not often are they all inclusive. Having it all in one app would be a good improvement.
- Having the possibility to set the application up to send personalized reminders for taking insulin.
- Sometimes diabetics forget to take their insulin. These days, Facebook is often used to call out for other diabetics that are in the neighbourhood that could lend insulin to those that forgot it at home. The application we are developing could have a feature that people can contact each other if agreed to, to request assistance from other diabetics near using location.
Some things are important to take into account. When determining the target audience, it is important to consider age. Wietske advises to take a target audience aged between 18 and 50 years old. She also told us that it is important to always include a disclaimer saying that the application does not give off any medical advises. It is also important to note that there is a difference between patients using an insuline pump and patients using an insulin syringe, since these work in a different manner.
Besides these advises, Wietske Wits told us that some more people in the past have asked questions to do research or develop an app, but she has never heard back or seen results. She would be very interested to see something actually developed. She asked us to stay in touch and ensured that for follow up questions we can always approach her. The interview seems to be valuable for our research.
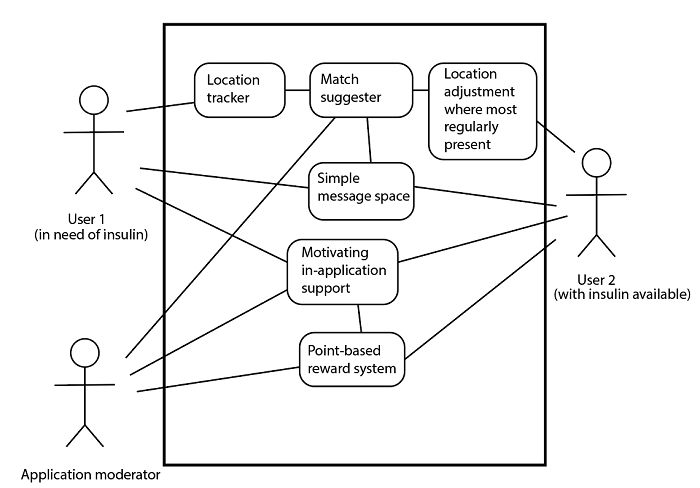
Use case
A use case for the idea of our application is suggested down below. In here, the two types of users are specified. These are of course not permanent roles, as one that has insulin to offer may another time be the user in need of insulin. In this way, users can support each other using the application and the possibilities it has to offer.
Figure X: Use case of application
As shown in the use case, the location trackers of the two users are not directly connected. This is to keep the privacy of the users in mind. The application can set up a connection or match between two users, without revealing personal data from one user to the other. This will make the application more user friendly. The moderator of the application will be aloof most of the time, especially when it comes to interaction between two users.
Requirement of the users
Our user requirements mostly depend on the functionalities our patient would need or want as a functionality of the app. The app has to make sure that the patient will follow a good diet (and that the patient will take his medicine), so the patient will have a (sort of) grocery list with the number of vegetables and other stuff the patient has to get. To help the patient to stick to this diet it will give many different examples of good meals to cook, but also to give the patient enough freedom to change some ingredients of those meals, like take other vegetables or choose chicken instead of pork. It should also be possible to choose a good meal from those example meals with a certain budget, so people do not have a lot of money, so it is very important to consider this as well. The app should also need the data of the measurement of the amount of glucose in the blood, based on these data the app can change the diet or call a doctor. It is not possible to measure the blood 24/7, so either a computer must simulate a person based on some measurements or the patient must measure his blood three or more times a day (the app can help remind this). This is very important because wrong data or forgetfulness of taking those measurements could lead to fatal problems.
To gather first-hand information about the requirements of the user an interview was held. The interview was held with the contactperson for diabetes in healthcare. The person has diabetes himself and acts as a communicationpoint for other parties who have questions about diabetes in the current healthcare system. The experience of diabetic patient is that has influence on their whole life. Around 150 moments a day the patient has to make decisions concerning their health due to diabetes; think about the concern for their bloodsugar-level in their blood. This has to be stabile and can be achieved with an insuline-pump, their diet or physical exercises. This constant attention towards these problems is very demanding of the patient throughout their day. There are around 42 factors which have influence on the bloodsugar level. Some very common ones are hormone cycle, emotions, tensions or stress due to work or adrenaline. There is never 'a day off' from the disease, it is always a danger to the patient.
So there are a lot of problems when having diabetes. Fortunaly for people with diabetes, there are already a lot of technologies to help a person. Think about automatic insuline-pumps which are connected to a bloodsugar-meter.
A type 1-patient does not need to follow a certain diet, but they do need insuline. They need this in two forms, namely one 'long-working' insuline shot and 4 'short-burst' insuline shots with meals. More and more people are getting an automatic pump-sensor device to control the insuline intake of the patient.
Some very important notes of the interviewed person where that people tend to forget to take insuline during mealtimes. This can be an improvement for current technology. Also, a carbohydrates-counter would be a fine addition to the current technology. The app can help make decisions about food. This remark is in accordance with the initial idea of improvement for our current technology. A remark which the interviewed person repeatedly emphasized on is that the disease is demanding the attention of the patient 24/7. Large leaps can be taken here, for example encouragement to the patient would be a fine addition or just plain humor. Nowadays, app are very concise and to the point. A more humain app is better for the person. Calculation of insuline according to the food the person wants to eat is also a good addition.
State-of-the-art
Diabetes applications
The market of diabetes applications on smartphones has grown immensely over the past years. Users can choose between many options, no matter which operating system is running on their phone. Presented research has focused on Android users, since our prototype will also be developed for that platform. The list below consists of some of the most popular applications. They were downloaded and tested, so that we would obtain some first-hand experience. At the end there is a paragraph summing up the general findings.
- Calorie Counter - MyNetDiary, Food Diary Tracker [6]
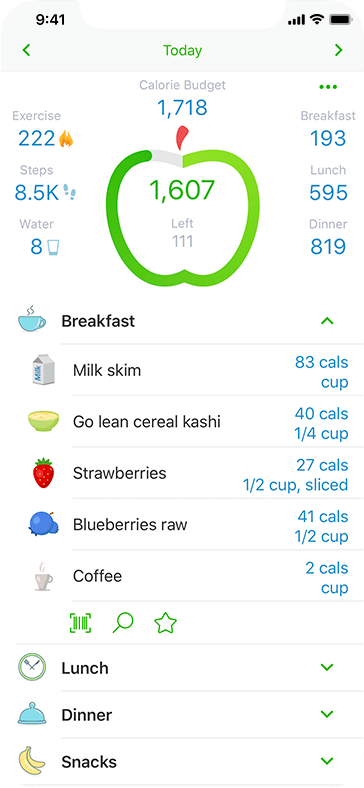
Example screen from MyNetDiary - Made not specifically for diabetic people, but for anyone who wants to have better control over their diet. Biggest advantage is the very big database of foods, with the possibility of updates from users. Includes a barcode scanner that allows to scan the food package for easy calorie and nutrients entry.
- The proposed (by the creators) way to use the application is as follows:
- Set a weight goal
- Enter a target date ( vacation, wedding, or reunion )
- Get a calculated Calorie Plan
- Log daily meals and exercise
- Follow daily Calorie Budget
- Reach your goal
- The application is extensive and sophisticated. However, it lacks support for functionalities specifically in need by people with diabetes, such as measuring/logging sugar levels. Some of those features are only unlocked if the user buys the full version of the application. A subscription costs $9 USD monthly. Thus rendering this option attractive for our target user only if they are willing to pay.
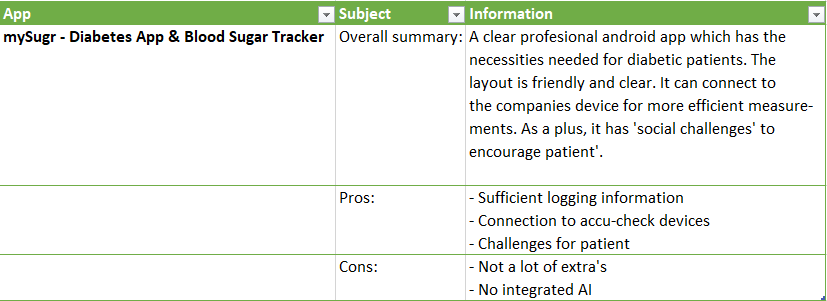
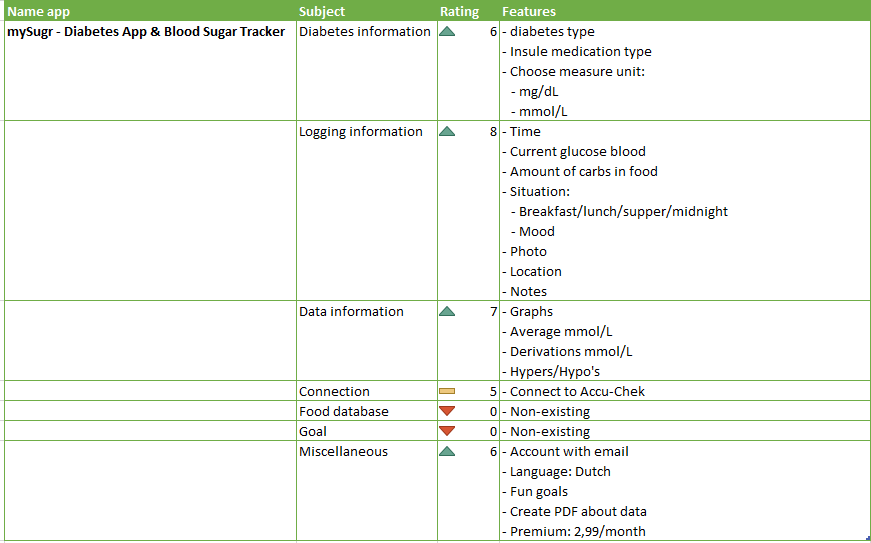
- mySugr - Diabetes App & Blood Sugar Tracker
- link to Google Play
- This application's target users are indeed people who struggle with diabetes. It was reported to be amongst the most used by the participants of this link study. It provides a vast range of activities. However, to fully benefit from the functionalities it is required to invest in the full version of the application. Some of the features are blocked or limited in the free version, for example only 5 food scan per day are allowed. This application supports
- Blood sugar tracking
- Meal logging
- Insulin dosage calculation
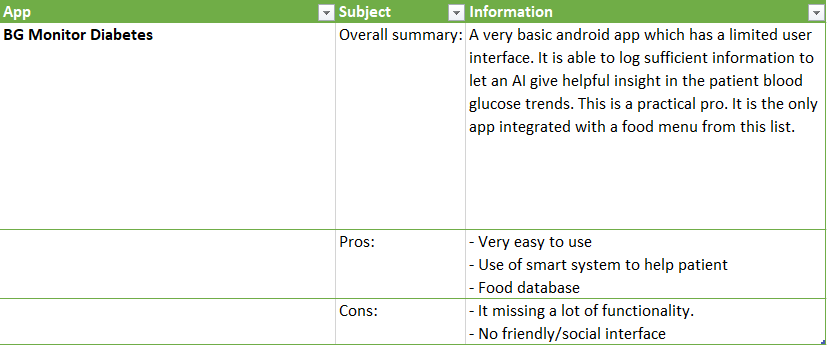
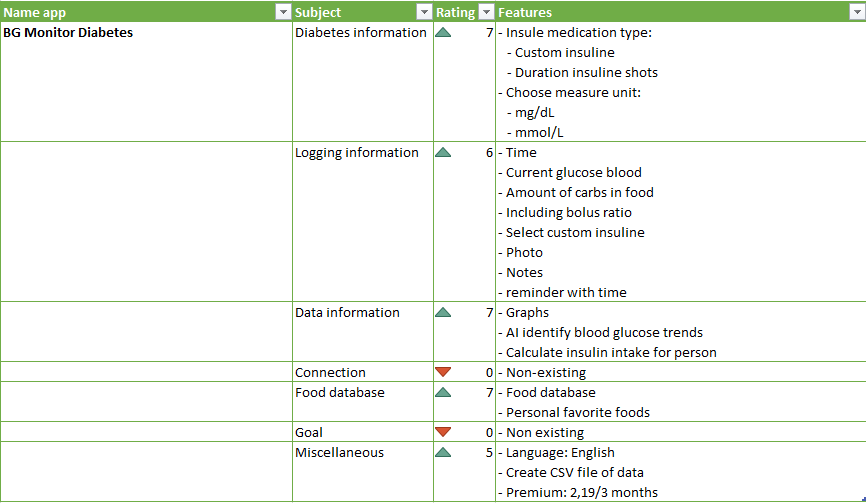
- BG Monitor Diabetes
- link to Google Play
- Functionalities available in the pro version (costs $4.99):
- Supports reminders to check your blood or give insulin
- Automatically calculates insulin dosages and total carbohydrates from multiple food servings
- Creates reports and can email them to healthcare provider within app
- Stores data on external could service for easy recovery
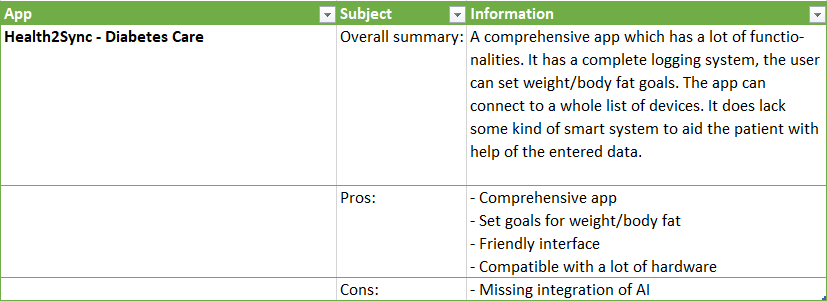
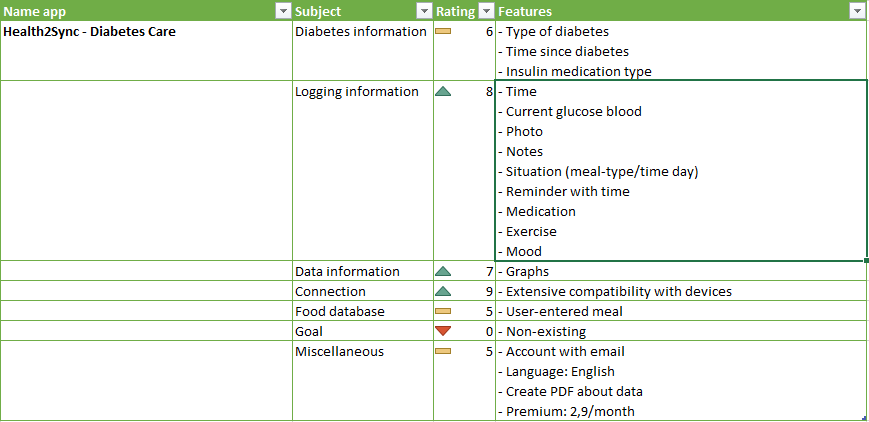
- Health2Sync - Diabetes Care
- link to Google Play
- Support logging and tracking of various inputs, such as blood sugar, blood pressure, weight, medication, diet, exercise, and mood.
- Distinctive feature of the application is the possibility of inviting 'partners' that have oversight over the gathered statistics and can provide encouragements.
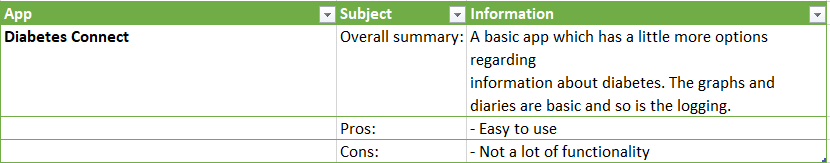
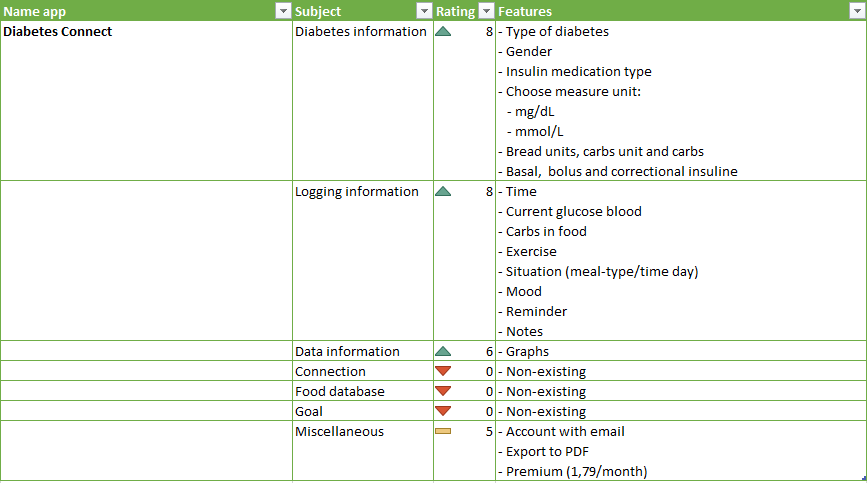
- Diabetes Connect
- link to Google Play
- Simple interface, easy to use and intuitive to navigate. Tracking weight, blood sugar, meals, insulin injections, medication. Supports synchronization over multiple devices.
- Can enter multiple data at once: blood glucose, insulin, and carbohydrates
- Glucool Diabetes
- link to Google Play
- Highly customizable: custom insulin, medication types, and exercise types
- Can enter multiple data at once: blood glucose, insulin, and carbohydrates
- Premium version costs 7.99$, unlocks all features such as creating graphs
The market of applications for diabetes users is very well developed. Users have a choice between many options that enable them to track every aspect of their illness. The basic options for every app include logging of information such as blood sugar level, insulin, meals, medication and activities. Some of them provide the option to generate graphs about the data. Most of the applications are not free, if the user want to make us of all the features they have to pay. The price range varies from 3$ one time purchase to 10$ monthly subscription plans.
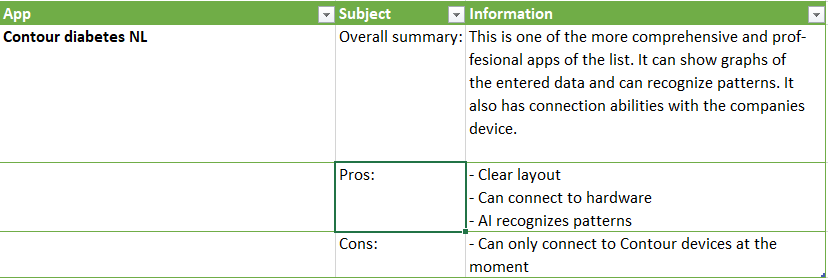
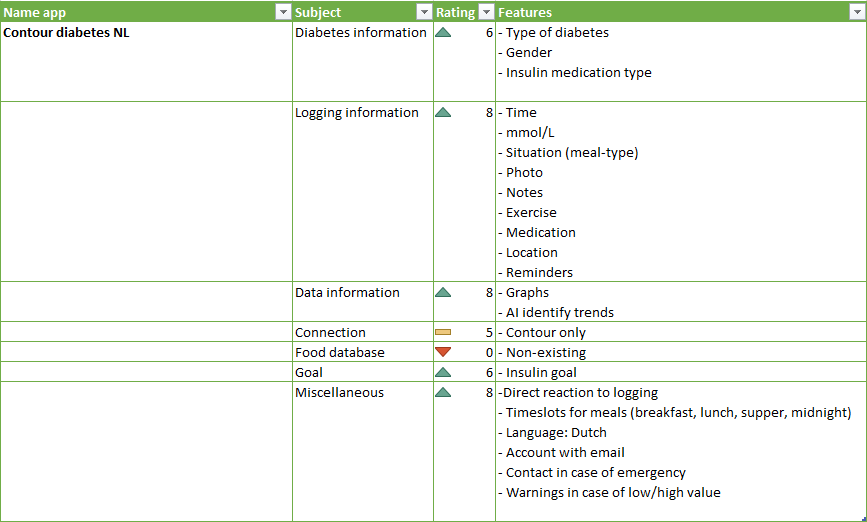
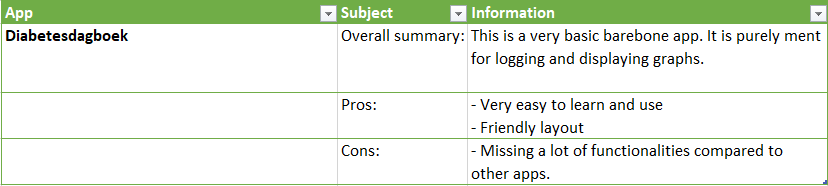
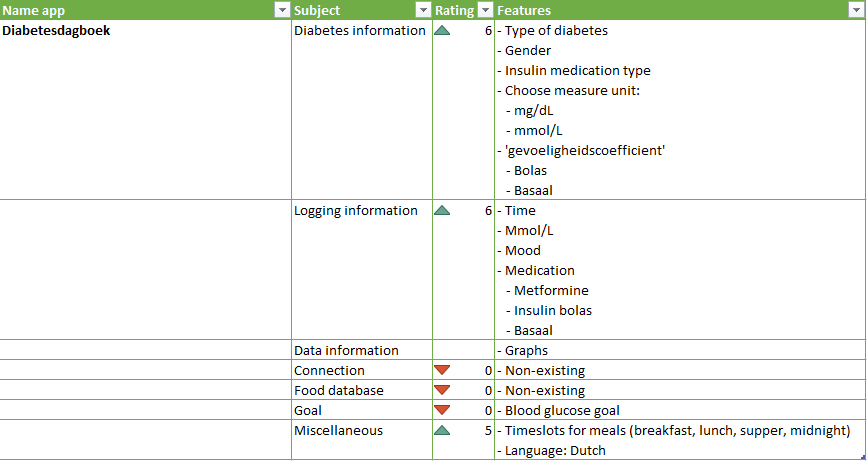
After extensive research an excel file is made with the most important information about the general apps about diabetes.
Usage of applications by people with diabetes
Nowadays smartphones are considered widely available and most people in highly developed countries make use of them. The total number of smartphones users worldwide was estimated to be 2.90 billion in 2018 [7]. The market for smartphone applications dedicated for people struggling with diabetes has also grown immensely. Only from 2011 to 2014 the amount of applications has risen from 80[8] to an astounding amount of over 1000 [9]. In 2018 this number was already around 5000(!), 3600 updated regurarly[10] However, according to the same research of the market, only 1.2% of the target group (people struggling with diabetes) were using an app in 2011. It was predicted that this number will increase to 7.8% in 2018. We could not find any recent research that would confirm this claim. This number of users also raises some suspicions from our side, since not all people have access to smartphones and not all people are skilled enough to use them. We suspect that taking these things into account the real percentage might be considerably higher. On the other hand, it has been shown [11] that compared to individuals without diabetes, smartphone use remains significantly less likely among individuals with diabetes, even after adjusting for age, race, ethnicity and socioeconomic status. Unfortunately no further studies have been conducted trying to explain this phenomenon.
Many reports indicate that the current state of the art for diabetes application is far from ideal. Practice standards are not met by these applications [12], causing a lower than expected number of users. The standards accepted by the market include:
- Personalization, i.e. modifiability, how much control does the user have over how the data is displayed and what information is gathered and shown in the first place
- Feedback, for example about the progress. The social aspect, connecting to other users is also very important.
- Feature coverage. An ideal application should have all the needed features in one place, users will not use several apps
- Integration. Supporting multiple platforms and devices, connecting to external devices such as glucose meters
- Motivational system. Related to the social aspect, encouragement from the application and other users has proven to have a positive impact
- Ease of data input. Effortless usage
- Design and user experience, aesthetics
Those standards were tested in a study done by Chomutare et al. [13]. They also concluded that personalized education is an underrepresented feature in diabetes mobile applications. No studies evaluating social media concepts in diabetes self-management on mobile devices was found, and its potential remains largely unexplored. Again, this touches upon the issue of diabetes applications being 'passive', instead of providing targeted support for users.
Another review of the market of diabetes applications [14] performed in 2015 claims that out of 65 reviewed applications "56 of these apps did not meet even minimal requirements or did not work properly". One of the conclusions was that users would benefit greatly from reminders (such as reminders for measuring blood glucose, insulin therapy meals and physical activity), which currently are not implemented to their full potential, despite being an effective method of increasing medication adherence[15]
The market is full of apps of dubious quality, but we still wanted to determine whether
- people are using these apps in the first place
- apps help improve their self-care
Research about these two matters is presented below.
For our project it is important to establish whether there is a relation between using diabetes apps and quality of health. A study[16] published in March 2019 was conducted to answer this question. From November 2017 to March 2018 an online survey was conducted. "One thousand fifty two respondents with type 1 and 630 respondents with type 2 diabetes mellitus (DM) entered the survey. More than half, 549 (52.2%), and one third, 210 (33.3%), of respondents with type 1 and 2 DM, respectively, reported using diabetes apps for self-management. To measure how participants took care of themselves a questionnaire from the Summary of Diabetes Self-care Activities was used. It included positions such as “general diet”, “specific diet”, “exercise”, “blood glucose testing" and “smoking”. Using diabetes apps for self-management was positively associated with higher self-care behaviour in both types of diabetes. Respondents tend to care more about their health if they are using an application. In other words, applications aid them in improving their lifestyle. Similar conclusions were made by Krishna and Boren [17] after investigating a comprehensive list of studies that evaluated the use of cell phone for health information. Using mobile phones results in improvement of health outcomes, because users become more knowledgeable and aware of their disease. It helps by providing care, support and aids in self-management improvements.
These findings support our motivation for the project - we want to help people with diabetes and improving smartphone applications can make a difference.
There may be many different apps to choose from, but most of them lack crucial functionalities[18]. From all the apps that were tested (371) all of them supported blood glucose level recording. However, alerts about hypoglycemia or hyperglycemia were found in 58.8% of apps, where only 20.7% and 15.4% supported an action prompt for hypoglycemia and for hyperglycemia respectively. Thus upon further investigation we see that only a very small percent of all apps has more advanced features implemented. Admittedly, the situation has improved. In 2011 the Android Market had no apps that offered direct data input from glucometers [19] and tracking insulin was an option only in 45% of the applications.
From our perspective the most crucial features are missing, those relating to autonomous actions of the application/system. Most of the apps can be used as sort of a logbook, allowing users to keep track of various things. There is however no active feedback from the applications, such as advices on what to do if the patients' blood sugar level drops below a certain level. There is evidence [20] confirming that active feedback and a care system that supports making clinical decisions achieves better results than just logbook based aids. This study performed a trial with adult patients that suffer from type 2 diabetes. Patients were assigned to one of two groups: mDiabetes or pLogbook (paper logbook). After 24 weeks there was a noticeable difference between the HbA1c levels in those two groups. The implementation of the mDiabetes for patients with inadequately controlled type 2 diabetes resulted in a significant reduction in HbA 1c levels. The mDiabetes group ex- hibited a lower blood glucose level at prebreakfast, prelunch, and postdinner than the pLogbook group did.
Application
Approach
Milestones
Week 1
- Form a group
Week 2
- Choose a subject, make it concrete.
- Update the wiki page with all the basic information (problem statement, objectives, users, deliverables, milestones)
- Prepare a meeting with a person from the diabetes centre
- Make a separate plan of the application development process
Week 3
- Interview processed to improve information on user needs
Week 4
- Concrete idea of what application to make
Week 5
Week 6
Week 7
Week 8
Finish writing our wiki and give the presentation of our project
Deliverables
The literatures
Logbook
Week 1
Missed because of problems with group forming
| Name | Student number | Activities (hours) | Total time spent |
|---|---|---|---|
| Kasper de Bruijn | 1333046 | ... | 0 |
| Nick Jansen | 1260731 | ... | 0 |
| Davide Fabbro | 1255401 | ... | 0 |
| Kamil Musiał | 1283073 | ... | 0 |
| Milan Koumans | 1256041 | ... | 0 |
Week 2
| Name | Student number | Activities (hours) | Total time spent |
|---|---|---|---|
| Kasper de Bruijn | 1333046 | Meeting Monday(2), Meeting Thursday(2), user research(2), preparing interview(2) | 8 |
| Nick Jansen | 1260731 | Working on wiki(1), Meeting Monday(2), Meeting Thursday(2) | 5 |
| Davide Fabbro | 1255401 | ... | 0 |
| Kamil Musiał | 1283073 | Meeting Monday(2), Meeting Thursday(2), wiki template (1), research state-of-the-art diabetes technologies (5) |
10 |
| Milan Koumans | 1256041 | Meeting Monday(2), Meeting Thursday(2), defining problem statement and research about diabetes (4) | 8 |
Week 3
| Name | Student number | Activities (hours) | Total time spent |
|---|---|---|---|
| Kasper de Bruijn | 1333046 | Having an interview and working this out(3), researching used needs and possibilities for application(3), adding interview and user needs to wiki(1) | 7 |
| Nick Jansen | 1260731 | Research on Firebase (8) | 8 |
| Davide Fabbro | 1255401 | ... | 0 |
| Kamil Musiał | 1283073 | Research on diabetes apps usage(4) | 4 |
| Milan Koumans | 1256041 | ... | 0 |
Week 4
| Name | Student number | Activities (hours) | Total time spent |
|---|---|---|---|
| Kasper de Bruijn | 1333046 | contact with Diabeter(1), searching for user needs(3), updating existing interview and scouting for new user case or source(5), developing use case(2) | 11 |
| Nick Jansen | 1260731 | Made a login, register and begin page in Android studio (3), Link the register page with Firebase via a Realtime Database (5), Link the register page with Firebase via Cloud Firestore (5), Did research on how to get data from one of the two databases (7) | 20 |
| Davide Fabbro | 1255401 | ... | 0 |
| Kamil Musiał | 1283073 | Finishing and writing down research on diabetes apps market, comparing with findings from the other group (6), Getting familiar with Google Maps API for Android (5), Creating a prototype app that implements location features needed for our project (6) | 17 |
| Milan Koumans | 1256041 | ... | 0 |
Week 5
| Name | Student number | Activities (hours) | Total time spent |
|---|---|---|---|
| Kasper de Bruijn | 1333046 | ... | 0 |
| Nick Jansen | 1260731 | ... | 0 |
| Davide Fabbro | 1255401 | ... | 0 |
| Kamil Musiał | 1283073 | ... | 0 |
| Milan Koumans | 1256041 | ... | 0 |
Week 6
| Name | Student number | Activities (hours) | Total time spent |
|---|---|---|---|
| Kasper de Bruijn | 1333046 | ... | 0 |
| Nick Jansen | 1260731 | ... | 0 |
| Davide Fabbro | 1255401 | ... | 0 |
| Kamil Musiał | 1283073 | ... | 0 |
| Milan Koumans | 1256041 | ... | 0 |
Week 7
| Name | Student number | Activities (hours) | Total time spent |
|---|---|---|---|
| Kasper de Bruijn | 1333046 | ... | 0 |
| Nick Jansen | 1260731 | ... | 0 |
| Davide Fabbro | 1255401 | ... | 0 |
| Kamil Musiał | 1283073 | ... | 0 |
| Milan Koumans | 1256041 | ... | 0 |
Week 8
| Name | Student number | Activities (hours) | Total time spent |
|---|---|---|---|
| Kasper de Bruijn | 1333046 | ... | 0 |
| Nick Jansen | 1260731 | ... | 0 |
| Davide Fabbro | 1255401 | ... | 0 |
| Kamil Musiał | 1283073 | ... | 0 |
| Milan Koumans | 1256041 | ... | 0 |
Minutes
References
- ↑ https://www.who.int/news-room/fact-sheets/detail/diabetes
- ↑ https://www.medicinenet.com/diabetes_treatment/article.htm#what_is_the_treatment_for_diabetes
- ↑ Dimitriadis, G., Mitrou, P., Lambadiari, V., Maratou, E. and Raptis, S., 2011. Insulin effects in muscle and adipose tissue. Diabetes Research and Clinical Practice, 93, pp.S52-S59.
- ↑ Venes, D. and Taber, C., 2017. Taber's Cyclopedic Medical Dictionary. 23rd ed. F.A. Davis Company.
- ↑ Venes, D. and Taber, C., 2017. Taber's Cyclopedic Medical Dictionary. 23rd ed. F.A. Davis Company.
- ↑ https://play.google.com/store/apps/details?id=com.fourtechnologies.mynetdiary.ad
- ↑ https://www.statista.com/statistics/330695/number-of-smartphone-users-worldwide/
- ↑ https://journals.sagepub.com/doi/full/10.1258/jtt.2012.111002
- ↑ https://research2guidance.com/top-14-diabetes-app-publishers-capture-65-market-share-of-the-diabetes-app-market-2/
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6484806/#jld190007r4
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4419894/pdf/1985360.pdf
- ↑ https://research2guidance.com/todays-diabetes-apps-are-far-away-from-meeting-the-seven-best-practice-standards-2/
- ↑ https://www.jmir.org/2011/3/e65/pdf
- ↑ https://link.springer.com/content/pdf/10.1007/s10916-016-0564-8.pdf
- ↑ https://academic.oup.com/jamia/article/19/5/696/2909139
- ↑ https://www.frontiersin.org/articles/10.3389/fendo.2019.00135/full
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2769746/pdf/dst-02-0509.pdf
- ↑ https://jamanetwork.com/journals/jama/article-abstract/2730605
- ↑ https://journals.sagepub.com/doi/full/10.1258/jtt.2012.111002
- ↑ https://care.diabetesjournals.org/content/early/2018/10/26/dc17-2197.full-text.pdf