PRE2016 3 Groep8
Student Numbers of group 8 members
- 0957735
- 0895428
- 0955135
- 0957168 Joris Verhagen
- 0960769
- 0959019 Bjorn van Rixtel
Problem definition
More than 1.2 million people in the Netherlands have diabetes. That is about one out of every fourteen people and everyday about 169 people are newly diagnosed. [1] Although it is treatable with medicines or insulin, it is a chronically disease you are confronted with everyday. Depending on the type of diabetes, people have to insert insulin three times a day, around every meal. A diabetes patient always has to keep track of the number of grams of carbohydrates that have been consumed. On the basis of a formula, it can be calculated how much insulin is needed to keep ones blood sugar level on healthy terms. However, this is a standard formula for everyone and throughout your own life it also differs how much extra insulin is needed for every gram of carbohydrates. This formula should actually differ for every person and change from time to time. It is also quite some work to always keep track of the food or carbohydrates you have eaten, especially for a plate full of hot steaming food...
State of the Art
Artificial Intelligence in Diabetes
Currently the most known AI approach in diabetes is the approach from PEPPER [8] (patient empowerment through predictive personalized decision support). PEPPER is a newly launched three-year research project, funded by the EU Horizon 2020 Framework. It’s goal is to create a portable personalized decision support system to empower individuals on insulin therapy to self-manage their condition. PEPPER employs CaseBased Reasoning to advise about insulin bolus doses, drawing on various sources of physiological, lifestyle, environmental and social data. It also uses a Model-Based Reasoning approach to maximise users’ safety.
Case-Based Reasoning (CBR) is a consolidated artificial intelligence technique, extensively applied in medicine, that tries to solve newly encountered problems by applying solutions learned from similar problems encountered in the past.
The system will be integrated with an unobtrusive insulin patch pump and has a patient-centric development approach in order to improve patient self-efficacy and adherence to treatment.
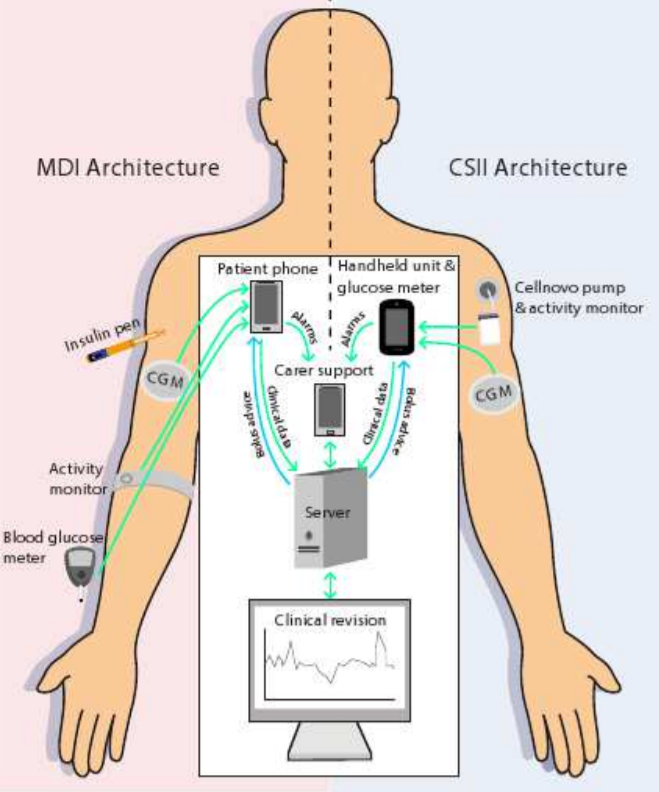
In the figure below, two architectures can be seen. These methods principally don’t differ quite much. In a nut shell, the PEPPER systems provide a portable personalised decision support system for insulin dosing that combines data from multiple sources such as body-worn sensors and manual inputs. These body-worn sensors for instance are the activity monitors that can be seen in the picture above. The manual inputs are given to the system by making use of a phone or handheld and consist of personal inputs like for instance the time someone sported, the amount and kind of food someone ate or the whether or not consumption of alcohol. The CaseBased Reasoning module is designed to provide a personalised insulin dose which adapts over time.
Idea
Goal
Our goal is to develop a diabetes application that helps a patient with the problems mentioned above. The most important part of the application is an algorithm that learns from the user and optimizes the formula accordingly. At the start of using the application you have to fill in what you have eaten on a day and your blood glucose level for a longer period. From this information the algorithm learns what your blood glucose level will be depending only on what you have eaten on a day. This information will be used to let the user know how much insulin must be inserted. Additionally, the input of what you have eaten should be simple. This can be done with text or a picture. The program also remembers what you often eat at a certain time of the day, so if you want to fill in what you have eaten you receive suggestions of specific meals or snacks. As extra help the application can be linked to a kitchen scale with Bluetooth. If you scoop up dinner on your plate while it is on the scale the application immediately knows how much grams of a certain kind of food you are going to eat. What the food that the user is weighing is, can be selected on the smartphone application.
Target group
The current state of the formula
Investigation in the existing research in formula optimalization
USE aspects
Existing Measuring Techniques
Test App for the software and formula
Userfriendly
Week planning
Task division
Introductory presentation, February 13th: Joris Veens, Ineke Kil
- Defining autonomous part for formula optimizing: Joris Veens, Jolien van der Thiel
- Bluetooth connected kitchen scale: Joris Verhagen, Bjorn van Rixtel
- Lay-out application (inputs, outputs as well): Ainse Kokkelmans
- USE aspects, ethical aspects, social relevance: Ineke Kil
Case scenario
Users
Current solutions to the problem
Most patients today use the manual calculation method for determining the necessary insulin dose. This is a time-consuming and, mainly in the beginning, a complex process, since 40-50% of the total daily insuline dose is to replace insulin overnight, when you are faston or between meals and the other 50-60% is for carbohydrate coverage and high blood sugar. [3]
Many of the diabetes patients find this process less than ideal. The weight and the amount of carbohydrates per certain amount of all the foods that the patient is going to eat needs to be known to calculate an insulin dose. There are, however, apps that take away some of the calculations from the patient. These apps will be explained in 'State of the art'.
State of the art
Two existing technologies to ease the insulin dose calculations are apps and insulin pumps. These technologies will be explained in this chapter.
Apps:
Current insulin calculating apps work on simple calculations. In general, the user enters their current blood sugar level and the amount of carbohydrates that the user is going to consume. The app will calculate the necessary dose of insulin for the user. Almost every application has the feature of saving the calculated insulin dose to a log. This log is able to provide insight over the user's glucose level throughout the day [4]. The app which is regarded by its users as the most useful on AppCrawlr, is the $1.99 Glucose Companion app. Since this is regarded as most useful, it can also be regarded as state-of-the-art concerning diabetes applications. The special feature that this app offers is that it can keep a better track on the glucose levels and insulin doses and that it gives advice on certain diet options [5]
Insulin pumps:
An insulin pump, which is shown on the image below, is connected to the patient by a cathether placed under the skin. When the pump is connected, the patient can receive short-acting insulin. The patient can increase the dose with buttons on the pump itself. This is to compensate the carbohydrates from a meal. The pump can also treat high blood glucose levels by taking a bolus. This is also determined by the patient him- or herself. It is important to note that the pump does not automatically correct the dose for everthing that the patient undergoes (such as meals and activities). The dose calculation is still done by the patient itself. The insulin pump has some advantages and disadvantages with respect to normally getting your insulin. These are stated below:
Advantages
The website from the American Diabetus Society gives multiple advantages [6]. The main one is that the patient does not have to bother with individual insulin injections which can really interfere with the patients life. Other advantages are:
- Insulin pumps deliver insulin more accurately than injections do.
- Insulin pumps result in fewer large swings in your blood glucose level since the doses are applied in a constant way.
- Insulin pumps allows the patient to be flexible about when and what he or she eats since ????????
- Insulin pumps allows the patient to excercise without having to eat large amounts of carbohydrates.
Disadvantages
The insulin pump does come with some disadvantages however. These are also given by the American Diabetus Society [7].
- Insulin pumps can cause weight gain to the patient.
- Insulin pumps can be expensive (and certainly are when they are not included in the patient's insurance).
- The insulin pump is connected to the patient most of the time. This can be bothersome.
In short, although the insulin pump solves some of the problems for the patient, it does not solve the biggest one which is manually increasing the insulin dose.
File:21235 large Insulin-Pump.jpg
Sources
[1] https://www.diabetesfonds.nl/home
[2] http://www.avdweb.nl/arduino/hardware-interfacing/scale-interface.html
[4] http://appcrawlr.com/ios-apps/best-apps-insulin-calculator
[5] http://appcrawlr.com/ios/glucose-companion#authors-description
[8] http://www.ecai2016.org/content/uploads/2016/08/W7-AID-2016.pdf