PRE2023 3 Group7: Difference between revisions
| Line 491: | Line 491: | ||
==Software== | ==Software== | ||
[https://www.youtube.com/watch?v=-8GiDhhR4Eg&embeds_referring_euri=https%3A%2F%2Fhubblecontent.osi.office.net%2F&source_ve_path=Mjg2NjY&feature=emb_logo App Demonstration (YouTube)] | |||
[https://www.github.com/svdgoor/pilpal Github Code] | |||
===Information System=== | ===Information System=== | ||
The app will allow users to have access to a constantly available application to answer personalized questions about their medicines. The app has the ability to answer questions about each of their medications, in combination with their schedule. | The app will allow users to have access to a constantly available application to answer personalized questions about their medicines. The app has the ability to answer questions about each of their medications, in combination with their schedule. | ||
| Line 531: | Line 533: | ||
# The system won't have a voice-to-text or text-to-voice system. - Although our target audience may benefit from being able to use voice and hearing to interact with the system, the state of the art is already established. Implementing this is technically very challenging, and we will not do so for this system, but it can be added in the future. | # The system won't have a voice-to-text or text-to-voice system. - Although our target audience may benefit from being able to use voice and hearing to interact with the system, the state of the art is already established. Implementing this is technically very challenging, and we will not do so for this system, but it can be added in the future. | ||
==== AI System ==== | |||
When it comes to the AI in the system, the intention is to use it to assist the patient in taking their medication and providing the patient with the necessary information regarding said medication. By giving the AI a personality, it will make the AI more approachable for the user to ask questions about medication. This can lead the user to start treating the AI as a companion, although that is not the intention. There is a fine line between giving the AI a personality and having it be used as a companion. This poses a rather difficult ethical challenge, as the goal is not companionship. It has been shown that voice assistants such as Amazon's Alexa is capable of assisting people with special needs do tasks they otherwise could not do themselves<ref>Zahy Ramadan, Maya F. Farah, and Lea El Essrawi, “From Amazon.com to Amazon.love: How Alexa Is Redefining Companionship and Interdependence for People with Special Needs,” ''Psychology & Marketing'' 38 no. 4 (2021): 596–609, <nowiki>https://doi.org/10.1002/mar.21441</nowiki>.</ref>. These systems can also provide companionship through conversation, however, the ethics on this are widely discussed. There have also been cases of people becoming emotionally attached to AI chatbots, which can lead to putting the needs of the chatbot above the users own needs<ref>Boine, Claire. “Emotional Attachment to AI Companions and European Law.” ''MIT Case Studies in Social and Ethical Responsibilities of Computing'', MIT Schwarzman College of Computing, 27 Feb. 2023, mit-serc.pubpub.org/pub/ai-companions-eu-law/release/2.</ref>. The human touch is also something that cannot be replaced with robots in care, which is why we do not want to make the AI system a companion. This again remains an issue, how do we build a system that gives the AI a personality, without creating the space for an emotional relationship to develop? | |||
When it comes to the AI in the system, the intention is to use it to assist the patient in taking their medication | |||
===Experiments === | ===Experiments === | ||
| Line 765: | Line 753: | ||
The final component in this diagram is the weight sensor, which is purely used to check if the user takes their medication out of the tray after it is dispensed. | The final component in this diagram is the weight sensor, which is purely used to check if the user takes their medication out of the tray after it is dispensed. | ||
==Medical Databases for Information== | ==Medical Databases for Information== | ||
| Line 788: | Line 774: | ||
For the design of our robot, the sensitive data is stored locally, and compartmentalized to avoid the unnecessary use of private data. The robot should have no access to personal identifiable information, but rather the relevant information; the type of medication and doses. The caregiver or doctor connected with the robot would have that information and for example: connect the medical dossier to a number that would be shared with the robot. The only viewer of personal data would be the doctor/caregiver, already having the patients permission. When it comes to the AI feature within the device, the patients can opt into allowing the device to access the medication names, and maybe the dosage of the medication. This is the only information the AI needs to help the patient further. With the name of the medication, the AI can look for publicly available information about the meddication in order to correctly assist the patient in taking the medication correctly. From the public database of medication, the AI can also inform the patient of the medications side effects, and should the patient allow the sharing of dosage to the AI, potential additional side effects relating to different dosage levels. The converstation between the patient and the AI is also data, which can be relayed to the care giver to validate the precision of the AI. To further reduce the potential of data being shared, the AI is stored locally, and the database can also be stored locally. This way the AI does not have access to the internet, and can only look into the local database. The AI and database can be updated via the internet, but all other interactions are strictly local. This can prevent data scraping, and reduce the wireless transmission of information. The only form of wireless transmission would then be to the caregiver. | For the design of our robot, the sensitive data is stored locally, and compartmentalized to avoid the unnecessary use of private data. The robot should have no access to personal identifiable information, but rather the relevant information; the type of medication and doses. The caregiver or doctor connected with the robot would have that information and for example: connect the medical dossier to a number that would be shared with the robot. The only viewer of personal data would be the doctor/caregiver, already having the patients permission. When it comes to the AI feature within the device, the patients can opt into allowing the device to access the medication names, and maybe the dosage of the medication. This is the only information the AI needs to help the patient further. With the name of the medication, the AI can look for publicly available information about the meddication in order to correctly assist the patient in taking the medication correctly. From the public database of medication, the AI can also inform the patient of the medications side effects, and should the patient allow the sharing of dosage to the AI, potential additional side effects relating to different dosage levels. The converstation between the patient and the AI is also data, which can be relayed to the care giver to validate the precision of the AI. To further reduce the potential of data being shared, the AI is stored locally, and the database can also be stored locally. This way the AI does not have access to the internet, and can only look into the local database. The AI and database can be updated via the internet, but all other interactions are strictly local. This can prevent data scraping, and reduce the wireless transmission of information. The only form of wireless transmission would then be to the caregiver. | ||
| Line 904: | Line 889: | ||
==Informal planning== | ==Informal planning== | ||
{| class="wikitable" | {| class="wikitable" | ||
! | !Week 1 | ||
! | !Week 2 | ||
! | !Week 3 | ||
! | !Week 4 | ||
|- | |- | ||
| Literature review + summaries | | Literature review + summaries | ||
Relevant groups’ work | Relevant groups’ work | ||
| Literature discussion | | Literature discussion | ||
| Line 921: | Line 902: | ||
Target audience & problem | Target audience & problem | ||
|Designing | |Designing | ||
| Line 927: | Line 907: | ||
Components + feedback + order needed | Components + feedback + order needed | ||
|Finalize components | |Finalize components | ||
| Line 933: | Line 912: | ||
3D modelling of product | 3D modelling of product | ||
|- | |- | ||
! | !Week 5 | ||
! | !Week 6 | ||
! | !Week 7 | ||
! | !Week 8 | ||
|- | |- | ||
|Software done | |Software done | ||
| Line 945: | Line 923: | ||
3D Printing done | 3D Printing done | ||
| Iterate on software or add app | | Iterate on software or add app | ||
Solve problems | Solve problems | ||
|Solve problems | |Solve problems | ||
| Line 955: | Line 931: | ||
Begin cleaning up wiki | Begin cleaning up wiki | ||
|Present | |Present | ||
Clean up wiki | Clean up wiki | ||
|} | |||
|} | |||
==Time spent== | ==Time spent== | ||
| Line 1,123: | Line 1,096: | ||
|- | |- | ||
|Sjoerd | |Sjoerd | ||
|Write code documentation, cleanup repository, update readme (4h); | |Write code documentation, cleanup repository, update readme (4h); Create software slides for presentation (3h); Make demo video (2h); Practice presentation (3h); | ||
|} | |||
Week 8: | |||
{| class="wikitable" | |||
|All | |||
|Feedback Monday meeting and evaluation (1.5h); Friday Meeting (1.5h); | |||
|- | |||
|Quinten | |||
|Securing, taking, transcribing, summarizing and interpreting interview (7h); Adding new info to slides (1h); | |||
|- | |||
|Fenna | |||
| | |||
|- | |||
|Thijs | |||
| | |||
|- | |||
|Daniel | |||
| | |||
|- | |||
|Sven | |||
| | |||
|- | |||
|Sjoerd | |||
|Clean up wiki about software (1h); Read and comment on wiki (1h); | |||
|} | |} | ||
==References== | ==References== | ||
<references /> | <references /> | ||
Revision as of 14:31, 5 April 2024
Pill dispensing robot
Team and interests
Quinten Liu, 1842471, q.m.liu@student.tue.nl
Fenna Sigmond, 1696947, f.e.sigmond@student.tue.nl
Thijs Frints, 1441523, t.g.g.frints@student.tue.nl
Daniel Joaquim Ho, 1534254, d.joaquim.ho@student.tue.nl
Sven de Gruyter, 1857657, s.d.gruyter@student.tue.nl
Sjoerd van de Goor, 1557815, s.v.d.goor@student.tue.nl
Interests:
- Medical Imaging
- Physical product
- AI
- Tangible / functional product
- Danger detection or prevention
- Healthcare or elderly care
Introduction
Overview
Medical adherence is the ability of a patient to follow their prescribed medication regimen and a remarkably important aspect of healthcare. And yet it remains a challenge worldwide for many people. Standard solutions for medication adherence usually use manual methods, such as pill organizers and reminders, which may not address all the different problems with adherence that patients have.
Smart pill dispensers are the current leading solution to improve medication adherence further for problematic patients. These use automatic medication dispensing, medication regime reminders, and remote monitoring capabilities for caretakers to address many of the problems manual methods don’t. While current smart pill dispensers have already shown to improve adherence rates, there is still a crucial factor in medical adherence that is often overlooked: the role of knowledge about the medicine in the patient.
The lack of important information about medications in patients, including the purpose, dosing instructions, potential side effects etc. of the medication is a possible cause for a lack of adherence. Patients could struggle to understand the importance of their medications or how to take them correctly, leading to unwanted yet avoidable treatment outcomes. So there is a need for solutions that help patients with the knowledge they need to make informed health decisions.
Our proposed solution to this is a smart pill dispenser with a built in information system, addressing the root causes of medication non-adherence that smart pill dispensers already do and adding a solution to the lack of information. This information system would answer any questions the patient would have and by integrating a robust information database and user-friendly interface, thus enhancing understanding, adherence, and by proxy, health outcomes.
Problem Statement
So, in the problem of medication adherence challenge lies an unaddressed issue, the lack of comprehensive medication information available to patients. This lack of information not only contributes to medication non-adherence but also exacerbates other problems, such as incorrect medication administration and misunderstanding of treatment regimens. Our product addresses and attempts to solve this problem by providing patients with access to accurate and accessible medication information. Through our information system, patients can obtain detailed medication instructions, learn about potential side effects, and receive personalized reminders in an understandable and accessible way.
Our Focus and process
While our proposed solution is a smart pill dispenser, the development of smart pill dispensers has already made significant progress in recent years, and state of the art products reflect that. Thus, instead of reinventing the wheel, our solution focuses on improving the software capabilities of existing smart pill dispensers. Our information system will have an aspect of modularity, serving as an independent component that would theoretically seamlessly integrate with existing smart pill dispenser hardware (not by the consumer, but by the manufacturers). This allows for this solution to fully focus on the information system and disregard the mechanical aspects, as will this report thusly.
Though, during the process and development of this project, the focus, end goal and expected result have shifted multiple times. To be as transparent as possible about this project's evolution and to make the intent behind all choices taken as clear as possible, this shift will be explained.
As a concept, the original thought up solution for medical adherence took lots of inspiration from typical state of the art smart pill dispensers, as the final concept did as well. However, back then the project’s focus lay closer to the mechanical device than it does now. Halfway into the project, during discussions and using received feedback, it was decided that the project would need to focus mainly on the software aspects of our device as the information system was the part not yet present in existing products. We believe that shifting our project’s focus like this halfway into the development cycle, while drastic, will greatly improve the usefulness of the eventual result.
As a result of this shift of focus, our report will still discuss some of the hardware aspects of smart pill dispensers, though less relevant to the new focus of the project. While less relevant than before, this information will still provide a basis for the knowledge on smart pill dispensers as a whole and can critique the current systems that they use. Additionally, all work for sections and information that have become fully irrelevant to our goal have been moved to the appendix.
Target Audience
Our proposed pill dispensing system should offer help for individuals struggling with the complexities of long-term medication management, which is a wide group. The limitations of our product and the needs of different subsections within this group helps us find a target audience that encompasses a wide range but still limited set of individuals that our product will be able to help.
Problems and potential solutions
Poor medical adherence is a serious and widespread problem. By looking through the facets of patients’ and caregivers’ problems, we can find the limitations of our system and propose how our system might be able to solve them. From this we can find flaws or difficulties that our system could face.
One of the most common problem patients face is forgetting to take their medication at their prescribed times.[1] Our product will be able to notify users about their medications when they have to take it, thus helping them in this regard. In cases that the user ignores or misses these notifications our system does not have the means to make them do it anyway. Similarly, if the patient has a lack of motivation, as patients with depression or anxiety can cause them to dismiss their medication against their interest, then our product can’t force them.
To partially solve this, our product could be able to detect whether or not the patient has actually taken the pills from the dispenser, to notify them again in case they missed the last notification or to notify a caretaker about the situation, but this still cannot confirm the patient’s cooperation as a very forgetful patient could take the medication, put it somewhere else and forget it again. Additionally, an uncooperative patient could purposefully take the medications only to throw them away as to look like they took it. The features and systems needed to circumvent this issue are currently still conceptually too complex to incentivize delving into them. This is thus our product’s main limitation.
The complexity of medication regimens also plays a role in the medical adherence of a patient. If a patient has trouble with a complicated schedule with multiple medications taken at different times of the day, in different conditions and in different ways, etc., the patient will be more prone to human error.[2] This issue is exacerbated in the case of a caregiver taking care of multiple patients with these kinds of medication regimens. Our product solves this by storing this schedule so that neither the patient nor the caretaker need to rigorously remember it. This ability to store complex schedules however, will be limited, as there will always be medication regimens too specialized and complicated to manage for a scheduler.
Another issue regarding medical adherence is the lack of information about the medication, consequences of not taking them and side effects. A patient may not fully understand why they need to take their medications or the potential consequences of not adhering to their prescribed regimen, and some medications can cause (unpleasant) side effects, which may lead patients to skip their medication without consulting their caregiver or healthcare provider. This uneducated group is a subsection of the previously mentioned group of uncooperative patients. Our product aims to solve this issue by being able to inform the user, with the user being able to ask questions about the medicine they are taking and the system looking up answers from a database.
Found target audience
Included target audience
Our product will aim to help people who are experiencing challenges regarding medication adherence, either due to forgetfulness, human error or a tendency to de-prioritize their medication regimen, or due to a lack of understanding or fear of adverse reactions. The product should also help caretakers and healthcare providers involved in the medication management process via notifications and updates about the patients medical adherence.
Excluded target groups
It’s important to keep in mind that our product is not targeted towards people who willingly choose not to adhere to their prescribed medication regimen despite understanding its importance. These patients will not benefit from the reminders or information provided by our system if they are intentionally uncooperative. Additionally, if a patient has a highly specialized and complex medication regimen, where our system cannot adequately address the unique conditions and complexity, the product may not be suitable for them.
Storyboard

To get a better understanding of a week in the life of a user of the medication dispensing robot. A purely fictional story was made to give insight into the functioning of the robot. All persons and examples are made up and are not based on a true story and any similarity are purely coincidental.
Medication[4]
To give a slight insight into the medication used in this storyboard, the following information is given about it.
- Lisinopril, a medicine taken when people suffer from heart failure, dosage: 10mg, ones per day. Needs to be swallowed with water. And taken after dinner
- Omeprazole, 20 mg, 3 times per day. To treat excess stomach acid. This one also needs to be swallowed with water.
- Migrafin, 3 times per day, 1 sachet, needs to be dissolved in a glass of water. To prevent migraine.
Elderly Person
Meet Jan, an 86 year old male, living in a nursery home on the outskirts of Eindhoven. A few years ago he was diagnosed with Alzheimer and therefore forgets to take his medication a few times a week. Currently the nursing home he lives in is understaffed and the nurses cannot visit him multiple times a day to check if he takes all his medication. To give an inside in this week day by day, a description of this week is given below. Currently he takes the following medication:
Looking at the amount of medication he takes, it can be concluded that he needs to take a total of 4 pills and 3 sachets of medication, on three different timestamps and with 2 different ways. To facilitate a way for Jan to take all his medication on time and in the correct way, the nursing home decided to put a medicine dispensing robot with an integrated AI information system into his home.
Monday
Jan wakes up to his alarm clock at 7:30, and gets out of his bed 10 minutes later. He heads to the kitchen in his home, to get breakfast. Here his medicine dispensing robot is standing on the counter, to whom he got more familiar during the last few weeks. After eating his breakfast he hears a beep coming from the robot, which is there to remind him that he needs to take his first medication of the day. He presses the button and get the two pills dispensed, with a notification that he needs to take the migrafin, which needs to dissolve in a glass of water. The robot shows him a notification on the screen, this notifications shows him an GIF-movie and tells him what he needs to do.
Afterwards he starts reading the newspaper and watches some television in his living room. When he suddenly hears the robot starting to beep in the kitchen. First he ignores it, but after multiple reminders Jan goes into the kitchen to get his dose of medication.
During the final part of the morning Sarah, a nurse, comes into his home to check in on him. She also checks the robot to see if Jan took all his medication. They have a small chitchat, before she leaves Jan’s home. Just before dinner Jan decides to lay down in living room chair and falls partly in sleep. One and a half hour later he awakes by a beeping sound, it is the medication robot. He slowly walks to the robot to see a notification on it that he is already half an hour late on his schedule. So he presses the button to get his medication out, which also shows him a message that he needs to take the Lisinopril after he eats his supper. Being a bit confused, since he took a nap just before, Jan did not eat supper yet. He therefore presses the button of the robot again to get more information about eating before taking the pill. The robot gives him more information and Jan decides to start eating supper and leaves the medication laying in the robot. Half an hour later the robot starts to beep, since the medication is still laying there, Jan quickly takes it and starts to prepare for bed.
Tuesday
The routine for Tuesday follows a similar pattern to Monday. Jan wakes up, takes his morning medication, and enjoys breakfast. The robot reminds him to take his midday dose of Omeprazole, ensuring his stomach acid is regulated throughout the day.
Just after the lunch Sarah comes into his apartment to refill the machine for the first time. Jan looks a bit strange at the nurse since he has not seen this happening earlier, which is noted by the nurse. She ensures him that she is carefully adding his medication into the robot, so he has enough medication for the following 4 weeks.
During the afternoon Jan goes out for a walk and do get some groceries at his local market. Before going home, he decides to sit down near the market and watches some people walking by. While walking home he remembers that he needs to eat dinner before taking his evening medication. So he eats his meal when he got home and hears the robot beeping just a few minutes later.
Wednesday
Wednesday starts a bit different compared to the final two days for Jan. He forgot to turn on his alarm clock yesterday evening. So around 9:00 he gets woken by a beeping sound, the medication dispensing robot! But Jan is completely not aware that the sound he hears is from the robot, so he forgets his medication. At 11:15 a nurse comes into his room and hears the robot beeping, she asks Jan if he already took his medication. To which Jan answers that he does not remember. At that moment the nurse opens the app that functions together with the robot. Here she sees that the medication that needs to be taken in the morning is still in the robot. So she makes sure that it gets dispensed, and help Jan to take it. She also tells him that for this day his scheduled medication will be two hours later for the rest of the day. Which the robot already mentioned on the LED-screen and in the app.
Around 15:00 the robot starts beeping again, Jan’s afternoon medication! He takes it and afterwards heads to the common room in the nursery home. Here he talks with some of his fellow elderly people and plays some board games, before the shared dinner the nursery home serves every Wednesday. He then walks back to his apartment to get his final dose of medication out of the robot.
Thursday
Every Thursday the nursing home organizes an elderly gym session, in which Jan always participates. This sessions always starts at 8:30 and therefore starts before his normal medication schedule. Luckily for Jan the robot knows that Jan is going the exercise in the morning and therefore gives a beep an hour earlier than normal. So he can take his medication earlier and therefore he still gets it.
Just after lunch the robot beeps for the second time, and Jan knows he needs to take only one pill. Finally he rests a bit before the television before making some dinner for himself and waits for his final dose of medication of the day.
Friday
Friday starts just as Monday and Tuesday, Jan wakes up to his alarm and eats his breakfast before hearing the beep of the medicine dispensing robot. He takes out his medication after pressing the button on the robot.
After his lunch and the midday medication take-in moment, Jan gets a visit from his two grandchildren Tony and Lisa. They chitchat a bit and play a few boardgames, before Tony and Lisa prepare dinner for their grandfather. Which Jan really appreciates, around 19:00 the three hear a beep. Tony and Lisa both don’t know where it is coming from and ask their grandfather if he knows. To which Jan answers that that is his new assistant to remind him of taking his medication. Lisa goes and has a look at the robot and sees all features that it has and askes Jan if he finds it useful. After thinking for a bit Jan answers with that it was strange at the start, but that he now feels a lot better about using medication and that he takes it more strictly. He then walks to the machine and presses the button to get his medication out and shows Lisa that it even has an option to get more information about his medication.

Caregiver
Meet Sarah, a 28 year old caregiver, she works in the nursing home where Jan is living. During her normal week she works 24 hours. In the following part of the text a description of these hours and division over the days is given. It is fully fictional and made to suit the description of the robot that is being designed in this research.
Monday
Sarah starts her week with the Monday morning shift, arriving at the nursing home just before 7:00. During the beginning of her shift she helps physically disabled persons with getting out their beds and helps them with washing themselves. She also provides companionship to the people that need it in the morning. She ensures that her patients are comfortable and well cared for before moving on to the next task on her planning.
She starts making sandwiches for the elderly in the common room and does this for an hour or so. Afterwards Sarah takes a walk through the halls and knocks on all doors to check if everyone is doing alright, during this walk she also visits Jan. He recently got a medication dispensing robot in this apartment, which Sarah checks to make sure that he took all his medication up until now. While checking the information on the screen, she notices that certain medications are almost used up. For this reason she makes a small notation in her app, which comes with the robot, that she needs to refill Jan’s medication tomorrow. Then Sarah asks Jan is feeling fine and continues her walk. Around 11:30 her shift ends and she goes home.
Tuesday
On Tuesday afternoon, Sarah returns to the nursing home for her shift, arriving at 13:00. She firstly looks at her personal schedule for the day and sees that she needs to refill the medication dispensing robot in Jan’s apartment. So this is what she starts doing, getting the medication from the storage and signing that she took the medication to Jan’s robot. When she arrives at his apartment she has a small chat with Jan and afterwards she fills the robot. Sarah then continues with her other tasks, she provides care to other residents and helps with the preparations for the dinner that evening
Wednesday
Sarah arrives around 16:00 at the nursing home for an evening shift. She starts by helping her colleagues from the afternoon shift with preparing dinner. Which is served around 18:00, during this dinner she accompanies some of the residents and has a chat with them about their day. After dinner she helps with cleaning up everything and helps the residents with getting ready for bed. Together with her colleagues she checks if everyone is in bed and she leaves the nursing home around 22:00
Thursday
Thursday is Sarah’s day off, this gives her the opportunity to rest and relax after giving care for three days straight. She was able to work less compared to earlier years due to robots helping the elderly in the nursing home.
Friday
Sarah returns to work on Friday morning, refreshed and ready to continue providing care to the residents. She tries to support the residents as good as possible and helps them with making breakfast and lunch. Afterwards she checks a few vitals for some of the elderly to see if they are still healthy. Ending her workweek at 16:00, and thinking about all the good work she has done this week and about the positive impact this has on herself and on the elderly living in the nursing home.
Preliminary Functional Requirements
App
- AI integration to understand speech
- AI integration to process natural language inquiries about medicine in the specific context of the patient
- AI integration to process natural language outputs to spoken language
- Software to memorize and on time inform about medicine intake
- Remember which medicine was taken
- Admin-client distinguishment in access to schedule
State of the Art
Available Dispensers on the Market

When it comes to the state of the art of medicine dispensing, there are currently two types of solutions: passive and active. The passive solutions are the standard pill boxes that allow the patient to sort the medication into smaller compartments based on which day the medication needs to be taken. Active solutions are the autonomous solutions that dispense medication, notify the patient, and even notify the caregiver when medication should be taken. This project aims to implement an active medication solution.
The passive solution comes in a variety of options, usually being a plastic container with sub-compartments for the storage of medication. These are the more traditional pill boxes, where the user needs to sort the medication beforehand into the correct sub-compartments. This type of solution tends to only hold enough medication for a week, requiring the containers be refilled and medication sorted every week by the user, where human error could play a role. This solution does not include any form or reminders, rather a container of all the medication that should be taken at a specific time. This still requires the user to remember to take the medication.

The alternative is an active device, of which there are three alternatives: DoseControl[6], the Hero Smart Dispenser[7], and Philips Spencer. The first device, DoseControl, is a radial pill box that can remind the user to take their medication. The medication still needs to be sorted into their respective compartments, and the time of medication intake set. However, once that is done, the device will rotate the medication compartments such that the next compartment is aligned with the dispensing hole. The device then rings like an alarm clock, and can send a notification via the app if it is set up on the user or care givers phones. This is already an improvement to the pill boxes, but still requires the periodic refilling and organizing of the medication into the compartments. This device also does not have a form of confirmation that the medication has been taken from the device. This is a relatively affordable device, currently available in the EU. Similar devices from other companies are also available.
The Hero Smart Dispenser is a device that has 10 compartments for medication, meaning that it can store up to 90 days worth of 10 different medications. This device is setup to play an alarm noise when it is time to take medication, and dispense the medication according to the prescription. The device is also connected to an app, and both the caregivers and patients can receive notifications when it is time to take medication. The Hero dispenser also has a button on it, which the patient has to press in order for the medication to be dispensed. This also allows for a second notification to the caretaker informing them that the patient has taken the medication from the machine. The app that comes with this device tracks data such as dosages taken, missed, and when medication was taken. This dispenser makes it quite easy for the users to refill the medication, and easy for the caregivers to remotely check on the adherence of the patient. This device is only available in the US, with similar products also being available in the US. This device is available on a subscription basis, directly from Hero.
The final active device is Spencer[8], which is made in collaboration between Phillips and Spencer Health solutions[9] is a medical adherance device, which dispenses medication. Spencer is by far the most technologically advanced device, allowing for dispensing for on the go, video calls with a medical professional, and is made to be data driven. Spencer is compatible with different Bluetooth health monitoring systems, which can be displayed on the screen, or visible to care administrators. The device is also easily refillable, although it will come in a proprietary box designed for within the dispenser. This device also comes with an app, and the same functionalities on the device can be accessed via the app. The device does ask for how the patient is feeling during the day, such as when medication is being dispensed. This way it can also monitor the general wellbeing of the patient, and relay necessary information to a caregiver. This is a really positive feature, but may be annoying for the user. Spencer can be deployed to patients at no extra cost when a home care giver deems it necessary, and can be provided via the patients home care organisation. It is unclear if Spencer can be provided when it is not deemed necessary, or if it can be provided to everyone upon request.
Added Value & AI
As stated in the problem statement, the state of the art is already quite advanced, so there is no real need to engineer a dispensing device when so many already exist. We aim to add an information module driven by AI that can be added onto an existing dispenser to help answer any questions the patient may have regarding the medication, as well as notify the patient in a more personalized manner. Notifications sent to the patient can be customised to their liking, letting the patients choose when they want the notification, and if they would like the AI to remind them via speech, similar to how a caregiver would. The AI information system is a valuable tool to be added to dispensers in order to prevent medication errors, such as incorrect dosage, or incompatible medication with allergies [10]. Wary patients may refuse to take medication if they do not have the appropriate information about the medication, such as potential side effects and incompatibilities with something they ate. The patient could look at the medical data sheet to check for the relevant information, but they may have misplaced the leaflet, or find it hard to read through. An alternative would be to ask their care provider, but they may not be available at that given time. The use of the AI is to provide accurate information to the patient upon request, as to not delay medication intake. The AI will assist the patient by taking the information from the medication datasheet and providing it in simple to understand sentence. The AI model can also be personalized to each patients individual needs. Should the patient want a more cheerful voice for the AI, it can be changed. This has some ethical considerations with having the AI seem human, and preventing the AI information system from becoming a companion. By making the AI reliable and predictable, it can be used without the concern for mistakes or erroneous advice.
An AI information system is not yet available, and this is due to the risks and responsibilities that come with generative AI, and the mistakes the AI makes. An example of this is Air Canada's customer service chatbot. Air Canada briefly used a generative AI chatbot as their customer service line, and the AI had wrongly informed a customer about a refund policy, which Air Canada then refused the refund [11]. A small claims court then ruled that Air Canada needed to honor the faulty refund policy since it was provided by the AI on their website. Air Canada has since removed the AI chatbot from their website. The EU has also labelled generative AI as high risk AI in the recently passed EU AI Act [8], which will soon further restrict the use of generative AI for applications such as this. The risks associated with mistakes the AI makes are too great [12].
However, on the 18th of March 2024, Nvidia announced their collaboration with Hippocratic AI to develop an AI Nurse to combat the lack of nurse staff in the US. Hippocratic AI's mission is to create safe AI for healthcare use and "Do No Harm" [13]. On their website, they have a wide variety of AI nurses that they are developing and testing. The AI model that they developed, Polaris, is developed for real-time conversation with patients, and is for low risk non-diagnosing tasks [14]. This, along with learning from human feedback is done to keep the model as safe as possible. Their evaluation of their model against a human nurse also proves that the model can perform as well as a nurse. The specifics of the evaluation is not clear, but the model does perform better that GPT-4 when it comes to specific information [14]. This is due to comparing the answers from Polaris, which has access to the patients medical file, to a standard GPT-4 model. The one most similar to the one we are working on would be something similar to the Hippocratic AI daily check in nurse, or the remote patient monitoring. Nvidia released a showcase video of this nurse AI interacting with a patient. With how the AI reacts and responds in the video, it seems to have access to the patients full information, and can interact with the doctor as well. Hippocratic has developed their own safety-focused AI model with healthcare as its primary use. This is the most developed case of a product like this, and it is still in testing. At the time of writing this, access can be requested to test the model, but we have not received it.
AI such as Hippocratic within the healthcare sector are still of concern due to a variety of factors. The transparency of the AI is a hard one to tackle since the models are so complex. Another concern is the ethical aspect of introducing AI into healthcare, and potential automation of healthcare that could affect quality of life [15]. The mistakes that the AI can make are also of great concern, especially since errors in medicine can have life threatening implications. Hippocratic has a page assessing their AI model based on some healthcare benchmarks, but it remains unclear how true this is until testing is done. With all these concerns, it is clear as to why there is still no major implementation of AI into the healthcare sector, even with data to prove AI reliability.
Medical Adherence
The problem we are trying to address with our product is a lack of medical adherence, predominantly because of forgetfulness. While it’s important to justify the design choices of the product, consulting existing literature and state-of-the-art products in this domain will accelerate the project's development by using existing knowledge.
A study done by the World Health Organization investigates medical adherences in long-term therapies. They found that long-term therapies more often need patient intervention due to medical misuse than short-term therapies. The non-adherence leads to partial or no improvement in the patient, increasing healthcare costs and time to recover. An adherence aid such as a pill-dispensing robot could potentially change the findings of the study and allow for higher success rates of therapies or lower patient costs[16].
Effectiveness
The effectiveness of technology in addressing medication adherence is important in the development of solutions that truly benefit patients. Research has shown that traditional, low-cost reminder devices, such as pillboxes and cap timers, have limited impact on improving adherence among nonadherent patients. A comprehensive review of data from over 50,000 patients conducted by Niteesh et al. in 2017[17] found that these commonly used devices did not significantly enhance medication adherence rates. So despite their widespread availability, these reminder devices often fail to address the multifaceted challenges associated with medication adherence. Factors like forgetfulness, the complexity of medication regimens, and lack of patient engagement likely contribute to the limited efficacy of these simplistic solutions as they are not directly dealt with, only lessened to some extent.
However, electrical Medical Adherence Products (MAPs) take a more promising approach to improve adherence rates. A meta-analysis of numerous peer-reviewed studies, encompassing a total sample size of 4,326 patients, examined the effectiveness of electrical MAPs in enhancing medication adherence[18]. The findings revealed a significant improvement in adherence rates, with MAPs demonstrating the potential to enhance adherence by up to 49%. Additionally, the key features common to successful MAPs were identified in the study. These include:
- Recording Dosing Events (Recording and keeping a record of the past dosing events, which is especially useful for caretakers.)
- Audiovisual Reminders
- Digital Displays
- Real-Time Monitoring (Monitoring availability for healthcare providers)
- Adherence Performance Feedback
Importantly, integrated delivery systems and the ability to record dosing events were found to be the most crucial factors, associated with the greatest improvements in adherence rates. So our approach to medical adherence solutions has already shown to be an effective one, and the most important factors are the ability to record dosing events and delivery integration. The latter will be outside of the scope of this project, but knowing the importance of the first is usefull.
Baxter Rolls
The Baxter roll, named after the pioneering company in its production, is one state-of-the-art solution for managing multi-medicine medication schedules in healthcare and private settings. Baxter rolls are comprised of an arrangement of connected transparent plastic pouches, each housing specific medications tailored to the patient's regimen. Printed on each pouch are details including the patient's personal information, medication types and dosages, and scheduled consumption times. Pharmacists, in collaboration with healthcare providers, carefully curate these rolls in accordance with prescriptions, typically spanning one to three weeks, thereby alleviating the burden of daily medication organization for patients.
The utilization of Baxter rolls has multiple advantages. By condensing medication doses into individual pouches, the clarity of medication intake is enhanced, simplifying the administration process and mitigating the risk of dosage errors. Moreover, research[19] suggests a notable improvement in patient adherence to prescribed regimens. However, despite these merits, the Baxter roll is not without its inherent drawbacks.
Foremost among its limitations is the restriction to solid oral dosage forms, such as pills and capsules, excluding injectable or inhalation medications within the roll. Consequently, patients requiring a combination of dosage forms encounter only marginal improvement from Baxter roll usage in managing their medication regimens, due to necessary supplementary dispensing mechanisms. Furthermore, the rigidity of the Baxter roll renders it less adaptable to changes in medication prescriptions, posing logistical challenges and potential disruptions to treatment continuity. Privacy concerns also arise, as the patient's personal details emblazoned on each pouch may be susceptible to inadvertent exposure to third parties, compromising confidentiality and data security. Additionally, the slightly costlier nature of Baxter rolls compared to conventional medication packaging models presents a financial barrier, potentially limiting widespread adoption and accessibility.[20]
In conclusion, while the Baxter roll enables improvements in medication administration, its efficacy is reduced by its limitations. Some of these challenges, including specific details on in what circumstances the medicine must be taken, can be addressed to improve patient trust and adherence.
Promising dispense prototypes
An important part of our design will be the dispense function. Research already lead to promising designs and prototypes that could be an inspiration in this project. For example the autonomous pill dispenser by Chawla[21]. In this project some important requirements are stated and a design is made that showed how these requirements can be met. first the requirements and than the design concept will be given:
- The device should be able to isolate a single pill from a group, regardless of the size and shape of the pills.
- The device should be able to contain multiple types of pills in case the patient takes more than one medication.
To achieve a fulfillment of these requirements a devise with cones were used to isolate the pills and a rotating mechanism, in which a servo motor was used to ‘dispense’ the pill, where it could be obtained by the medicine taker. The results of the prototype are promising, and we could use the cone design to dispense the pills in our prototype, however it should be looked into if the pills can be obtained easily, also for people with motoric problems.
Furthermore, a smart pill dispenser presented by Casciaro et al[22], gives another example of a mechanism, that could be used in our project to dispense the medicines. In this design "a slot is divided in two sections, one containing electrical and mechanical components and one containing a flexible belt with teeth molded onto its internal and external surface. The internal teeth allow the belt to rotate around two pulleys, one of which is driven by the stepper motor. The larger external teeth allow to keep the pills. When the belt rotates, the pills move together with it, and when one of them arrives in the lower part of the belt, it falls off the tooth and simultaneously the servomotor opens the inferior lid and drop out the pill through a special opening located at the bottom of the dispenser, from which the patient can take it"[22]. This design seems to be flawless in dispensing the right medication and the right amount because of the teeth that only let 1 pill go through, but it should be further researched if pills cannot get stuck and if different types of pills can be put into this machine. Also, the systems seems to be more expensive and difficult to realize. Furthermore, in the paper some other possible requirements came forward such as a contact sensor to know whether the medication is taken or not.
AI in customer service
To enable a system to address customer questions, or in the context of the pill dispensing robot, patients' questions, research[23] shows that having AI integrated into chatbots has a positive influence on customer service. Further research[24] into the methods in which companies develop AI chatbots shows the importance of using personalization and intelligent routing for interactions with such systems. Furthermore, the author mentions the importance of suggestions, providing the user insight into which information they can retrieve, as well as personalization, such that the system improves its interactions with the user over time.
Notification ideas
A study about reminders for taking medication at fixed times vs at automatically time-shifted based on sensor data, showed that using the adaptive reminders the medication adherence (how fast people take the medication and user friendliness) is higher[25]. However, this time-based approach is not always the best as “for example, a reminder is triggered when the user is eating, whereas the medication should be taken after meal”[26].
The pillbox system collects real-time sensor data from a smart home environment and analyzes the user's contextual information through a computational abstract argumentation-based activity classifier. Based on user's different contextual states, the smart pillbox will generate reminders at appropriate time and on appropriate devices. This is quite complex and probably not manageable in this project but the idea of the notifications being at certain times to improve the medication adherence might be useful in this project.
Stakeholders and their interests
Problem statement
The general problem we are trying to solve with our product, and we’ll have to analyse surrounds the subject of medical adherence, the ability for a patient to keep following their medicine regimen. The problem is that medicine adherence is hard to keep high for certain people, be it voluntarily, because they don’t want to, or involuntarily, for example when the patient is forgetful. To identify the full problem statement, the most important stakeholders and their interests in the pill dispensing robot are identified using literature and interviews.
There are many stakeholders that share an interest in our problem, of which a handful are relevant and important to our product. These groups of stakeholders can be divided into three categories: User, Society, and Enterprise.
Users
The most important stakeholder to a medical self help device are the patients using it, as they are the ones taking medication. The patients are people that have trouble taking medication on time, or could use help in managing their medication schedule. A device like ours does not address the group of people who do not want to take their medication, only people who are forgetful or find managing their medication hard. The device can assist with medication adherence, which will be done by making a schedule for the medication, alert the patient when to take medication, instructions for taking their medication, and answering questions they might have.
Another group of users of the device is informal caregivers. These users will interact with the machine by setting the device up for the patients in their homes, inputting the medical prescriptions into the device, and refilling the medication. They can also use the device to monitor the medical adherence of the patient. This device aims to help the caregiver provide care for the patient when they are not physically present by automating the task of reminding the patient to take their medication throughout the day. The device can help a general practitioner get a better insight on the medical administration of a patient.
Society
When it comes to the societal aspect of the device, a major stakeholder are governing bodies. The government, specifically the EU parliament is responsible for legislation and regulations regarding medical assistance devices such as this one. National governing bodies would also decide what reimbursement policies there are for this device in the context of healthcare programs and health services, which doesn’t influence the implementation of the product but vastly changes the access and availability of it to the average consumer (Forsberg et al., 2000)[27]. They thus play a key role in deciding how these devices can be implemented and will contribute to society.
Enterprise
The companies that decide to produce such devices need to design the product such that the users are kept in mind. The hospitals and pharmacies that are partnered with these companies can provide the device to the user should a medical professional deem necessary, as well as provide the medication for within the device. Health insurance companies could also incorporate such a device into their insurance plans for people who need it.
Ethical Aspects
Having a robot replacing tasks a human would do comes with its concerns. Patients are still human, and need to be treated ethically. When it comes to a robot to take over tasks a care taker would do, it is important to not take away the human touch of care givers in healthcare and preserve human dignity[28]. This is also to not seem like the care being given is being automated[28]. This device should improve independence for the patient[29], such as assisting a dementia patient in self-management tasks, such as medication intake.
Shift of responsibility
Something to consider when conceptualizing a medication adherence device like ours is what effect it might have on not only the patient, but the caretakers too. Several ethical considerations arise regarding the responsibilities of caretakers. One of which revolves around the responsibilities that are taken away from caretakers due to the use of such products, as well as the new responsibilities that may be imposed on them.
Caregivers play a crucial role in the medication adherence management of patients. Especially in those with poly-medicated regimens and dementia patients. It’s currently important to train caregivers to understand the disease the patient has, as well as the importance of medication adherence in patients as to reinforce it to ensure optimal treatment and is thus recommended. (Segarra et al. 2022)[30] This task can be very hard to perform consistently for some caregivers, especially if they deal with multiple patients. With the use of smart pill dispensers, some of the tedious work can be alleviated. They can automate medication dispensing and reminders, reducing the direct responsibility of caretakers to physically administer medications at specific times, especially helpful when they have to deal with complicated or frequent dosage. Though, this responsibility would not disappear. It would be shifted to the device, and possibly thus to either the programmers or company of said device.
In return, caretakers, or patients self-medicating, would need to bear new responsibilities related to the oversight and maintenance of the smart pill dispenser. Foremost, the caretaker still has to confirm the medication adherence of the patient by interpreting the data they receive from the device, like recognizing patterns in the periods of non-adherence and correlating it to a potential barrier causing it, communicating with the patient or a healthcare provider when needed. The caretaker also needs to maintain the device by refilling, programming the patient’s regimen into it and troubleshooting technical issues, which does ask for a different set of skills from the caretaker. Additionally, caretakers might become responsible for ensuring that sensitive health information is protected from unauthorized access or misuse in accordance with the wishes of the patient, as many devices have configurable privacy settings to consent on the sharing of health information with the device company.
So, with the introduction of a smart pill dispenser like ours, caretakers are relieved from the tedious task of memorizing or planning the medication regiment of one or more patients, and are instead tasked with maintaining the device and interpreting the medication adherence data. In general, caregivers given the option for a device like this will highly prefer to choose it (Forma et al., 2022)[31], so the change of responsibility is generally seen as positive.
Responsible use of the guidance system
Our information guidance system is based on ChatGPT’s API, which is known to produce inaccurate information. On average, worryingly to some, ChatGPT produces 72-77% accurate clinical decisions. However, our guidance system will not be making clinical decisions for the user and should not be used in this way. Instead, our guidance system looks up and informs the user about existing clinical information and data when requested. Assessing the reliability of ChatGPT’s raw model, medical information had a reliability of 5.5 out of 6 on a Likert scale, as found by Johnson, D. et al. (2023). Seeing as our system will have the LLM looking up data from fed files, the accuracy might be higher, though this needs to be tested to know for sure.
The fact that the system is not always accurate is not hidden to the user and will be acknowledged. Thus, people who buy this product, like caregivers or forgetful people at home, will need to understand this and try to be more critical of answers given to them. These users bear the responsibility for how the guidance system is used and the decisions made based on the output. Furthermore, they are advised to not ask the guidance system
Starting Interview
It's been proven that in general, the development of technology for elderly people, especially mobile health applications that could improve their quality of life, can greatly benefit from having dementia patients and their caretakers involved in their design process[32]. To make use of this aspect of development, though through a limited form of cooperation, we have chosen to interview both patients and caregivers. It's important to note that this interview was taken before our project's focus went from a full pill dispenser to an information system. While the answers can contribute to knowledge about the state of the art of pill dispensers and can give context about the ways medication is taken, its contribution to the research for the information system will be limited. The answers that do contribute to this research will be underlined. Only a caregiver was interviewed, so some questions that where meant for the patient are asked during this interview to.
Patient
- Would you prefer to have this device be portable? Why or why not? (Stationary/portable)
- How do you take your medication on holiday or days out?
- Do you want to be able to take medication with you while on holiday? (Ability to take doses away from home)
- Do you prefer physical buttons or touchscreen to interact with the device? (Buttons/touchscreen)
- How many different medications should the machine hold? (Amount of different pills)
- How often do you get more medication from the pharmacy? (Storage capacity)
- How would you like to be notified to take medication? What notification method works best for you? (Notification)
- When the medicine is ready, the machine plays a noise and produce a light signal. It will also send a phone notification after 5 minutes if not taken. Would this be a nice way to be reminded?
- Would you prefer to fill the machine with pre-packaged rolls or pills from a bottle? (refill)
- How do you currently get your information about your medication? How would you like to receive information about your medication? (Information)
- What are suggestions for the device that would make it better to use? (General/ending)
Caregiver
- How does responsibility surrounding medicine intake currently work?
- Do you check that the patient has taken their medication?
- What would you like to be notified about? (Amount of monitoring/ validation)
- How do you want to be notified that the patient has to take/ has taken the medicine? (Notification)
- Would you prefer to fill the machine with pre-packaged rolls or pills from a bottle? (How to refill)
- What is the current protocol for medicine intake? Which aspects should the device do? (Security)
- What are suggestions for the device that would make it better to use? (General/ending)
Interview worked out
First a short description of the interviewee will be given. She works as a self-employed caregiver in the home care sector. This entails that she goes to her clients that live by themselves or with their families. Her clients are quite diverse. A great number of her clients are elderly, but she also has clients that are children or young grown-ups that live with their parents. Most of the clients take medicines that she brings to them and she talked about some problems that she came across.
1 How does responsibility surrounding medicine intake currently work?
She brings the medication to her clients homes. However, the clients of the interviewee mostly take their medicine themselves, and thus are responsible for their own medicine intake. However, she will check by asking if her patients really took their medication to somewhat have a form of supervision of her clients.
2 Do you check that the patient has taken their medication?
When she is with a client, she will regularly ask them if her clients have taken their medication, also she brings new medicines to them and helps them refill so she can check if the (old) medicines are taken.
3 Do you want to be notified that the patient has to take/ has taken the medicine, if yes, how?
She was interested in the idea of notifications for her to know if the medication is taken, but also mentioned that she did not need to know that her clients took their medicine every time they took them with a notification. Furthermore, it also differs per client, for example a notification if medication is taken from a client that has never forgotten their medication would not be needed.
4. Would you prefer to fill the machine with pre-packaged rolls or pills from a bottle?
She told that most of the time the medicines are pre-packed, so it would be easier to fill the devise with pre packed medications, however she gave an example of a client that does not have good motor skills anymore and has problems with opening a plastic bag with the medication inside, so it also depends a bit on the client.
5 What is the current protocol for medicine intake?
Again, the clients mostly take their medication themselves at set times, and are responsible for their own medication. They also know how take take their medication themselves for example with a glass of water and are capable of taking them the correct way, and if they have questions, ask her.
6 Does it happen that clients forget to take their medication?
She has had multiple examples of clients forgetting to take their medicines, and thus sometimes worries that the clients will forget their medication again. The reasons why medications are forgotten are mostly the times when a client is not at home and comes home late and therefore forgets the medicines. She does give an example about a client that has an alarm clock that drops a small bag of medicines when the medicines must be taken, which works quite well.
7 Which functions/aspects should the device have?
The notification system could be very helpful as said before. Furthermore, in some cases where the client gets new medicines or has a lot of different medicines, the information system will be helpful as for some clients it could be difficult to remember new descriptions or a lot of different all at ones. For specific situations, for example in where a client is ill (for a different reason than where they take their medication), this system could really help, she mentioned.
8 Would a portable medicine dispenser be useful?
She told that a portable medicine dispenser might be a solution to the problem mentioned before (6). However, she does see a problem that if the portable dispenser is only used when the clients go away from home that they might forget the medicine dispenser instead of only the medicines.
9 What are suggestions for the device that would make it better to use?
She gave example of a client that needs to grind their medicines before they take them, and suggests a function that a medicine dispenser in the future that could fully prepare the medication beforehand would be ideal.
Conclusion Interview
Even though the information obtained for the information system is limited, we could still learn from the current manner the clients get the information and the ideas of the interviewee considering the implementation of the system. For example that the notifications to a caregiver should only contain necessary information and could differ per client. Furthermore the information system could be a great addition.
Feedback Interview
A second interview with a different caretaker was taken after rough development of the app. We were not able to interview the same caretaker from the first interview because of time concerns, but believe this is not a loss of information to the project. The questions were chosen to get feedback for the application and to understand more fully how effective this approach to medical adherence and caretaking in general might be. Before the questions about our application itself, a video trailer about Nvidia's NurseAI was shown, a technology very close to our project in a few aspects, to better give a visual idea of what kind of end goal the project was going towards, as the application shown to the interviewee was still relatively primitive. The answers from the interviewee were summarized and made more concise but don't omit any relevant information.
A: Nvidia video (NurseAI) Shown to interviewee
1 Do you think this would be useful?
I’m unsure. The video does give off a somewhat dystopian vibe, and I would expect it might be difficult for seniors, especially those who are not tech-savvy, to use effectively. But in a nursing home setting where there may be a shortage of personnel, this technology could be useful. The ease and simplicity of the product is very important.
2 If it were available to you, would you use this?
It's a tough question. I do think an AI like this would lack the ability to fully understand the nuances of human interaction, especially in healthcare settings where empathy and compassion are important. Additionally, there are worries about medication adherence and whether this AI could effectively address those concerns. Again, given the lack of personnel in nursing homes, I would think this technology would be useful.
B: Our app is shown to the Interviewee
3 Would you want to use this app?
Yes, I think. While I would prefer to speak with a person for more complex issues, having an app like this for quick questions or information could be quite handy, not just for patients, but for caretakers as well. Because we don’t know everything all the time. Of course, the accuracy of the answers should be good.
4 What do you think is redundant?
At this stage, I don't see anything as redundant. The app seems quite primitive, but that's not necessarily a bad thing. Keeping it simple is important.
5 What difficulties could you see being faced by caretakers?
One challenge I expect is ensuring that caretakers ask the right questions to get accurate answers. Providing training for caretakers could help mitigate this issue. It's important that the app remains user-friendly by being simple.
6 What difficulties could you see being faced by patients using this app?
Patients will need to learn how to use the app effectively, which may be a challenge for some, particularly elderly individuals who may not be as comfortable with technology. You really need to understand that some seniors are utterly inept with simple technology. And some caretakers too even.
7 What functions do you think are still missing or would you want to see added?
I think adding features like speech-to-text and text-to-speech functionality will improve accessibility and usability for people who struggle with technology. I also expect a feature allowing users to input personal information for more personalized responses can help, like weight, height, age and stuff, as some medicinal advice depends on those numbers. But simplicity should really stay a priority here to ensure ease of use for all users.
Conclusion Interview
It's clear that the addition of an information system can be useful to a pill dispenser for caretakers and is seen as such, at least to this interviewee. One of the most reoccurring subjects that kept coming up was the simplicity of the application. It's important that the design and function of the information system's user interface is kept simple and user friendly, to cater to patients and caretakers that struggle with technology. Additionally to that, an incorporation of text-to-speech and speech-to-text would greatly help the same problem. And the interviewee mentioned that user information such as age, weight and length and such are factors that play a role in medication, which he brought up because during the demonstration, this issue came up, so this might be something to incorporate as well.
Robot Hardware and Design
Robot Description
We have designed a small (portable?) robot to act as an medication adherence aid for chronic/long-term medication therapy. The robot is to be used as a home product of the patient and can remind the patient to take their medicine (on-time). The robot can contain multiple types of solid medication and is able to release predefined doses per time period as set by the caretaker or patient. When the time comes for a patient to take their medication, the robot will notify the patient via its built-in LED screen and speakers. The combination of audio and visual stimuli is used to ensure that the patient takes notice of the robot and is reminded of their medication. In the case that the patient would like more information about their medication, as they would get in the information leaflet provided in the package commonly bought, the user presses a button and the LED screen and speakers will inform the patient.
Full Dispenser System
The main differences that come with the full dispenser and the system we wish to implement is that the full system also takes care of the dispensing aspect of the device. Since this has been done successfully by a number of companies, the team decided to focus on the information aspect of the device. An information system has not been implemented yet, and the addition of the information module will help aid in the medication taking process.
Hardware
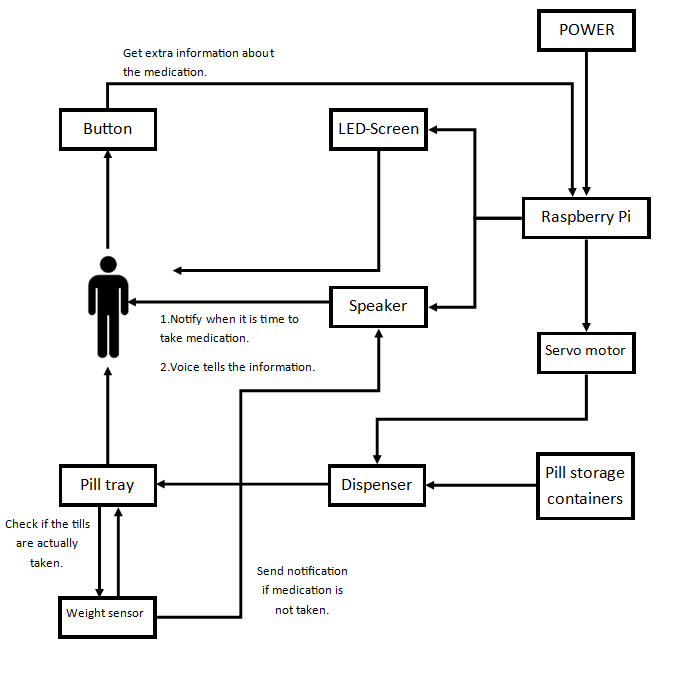
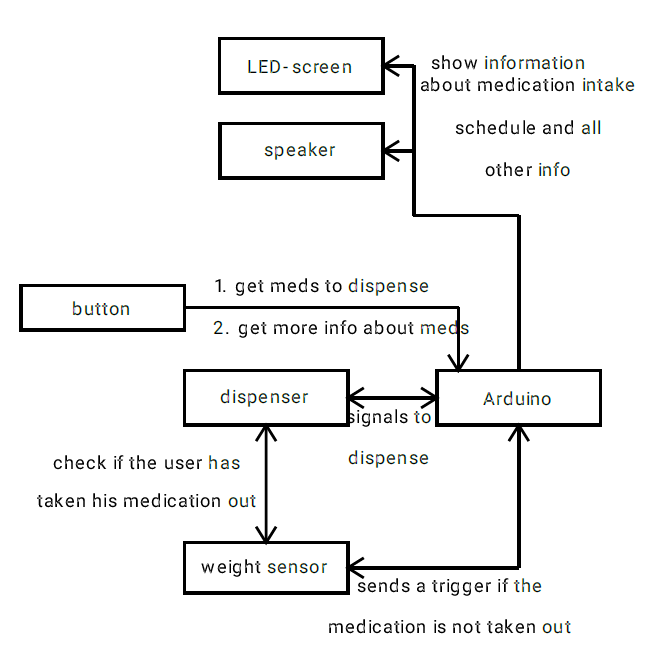
When it came to the hardware design for the prototype, the team came up with two possible solutions. The first solution uses all the components that the team ideally wants to use to create a full prototype. The second solution is to maintain as much functionality as possible, while making it as cheap as possible for the device to be competitive in the market. This second solution came about to allow the device to be more accessible to the consumer[33]. Regardless of the solution chosen for this device, the components necessary are defined by the functionality the device should have. To define the function requirements of the device, the following block diagram was made. The device needs a:
- processor to store and run the software, as well as to interact with the other components of the device.
- button for multiple functions. The user can press it to dispense their medication once a notification has been sent out. This will also turn off the notifications. It can also be used to get more information about medication.
- screen to display information about the medication, prescription, and can also be used to notify the patient by flashing.
- battery or power cord to power the device.
- speaker for auditory notifications. It can also be used for verbally informing the patient about their medication or prescription should the patient want that.
- servo motor and controller to dispense the medication from the storage containers.
- storage method for the medication to be dispensed.
- collection tray to collect the dispensed medication, which can then be removed by the patient to take the medication.
- sensor to check if the user really took the medication out of the tray and sends a notification if the medication is not taken out.
- body to house all the components.
When it came to the ideal system, the processor of choice was the Raspberry Pi 4B for its versatility, and the capabilities of Bluetooth and WiFi. This way, the device can communicate with the app on the users phone. For the display, a 7" Raspberry Pi compatible touchscreen display was chosen for its large size, and its compatability with the processor. In terms of power, there are two options. The first is to plug the Raspberry Pi into a socket, which would make the device stationary, and the second being a battery. To check battery life, different operating modes and battery capacities were checked with PiJuice[34]. This yielded a 12000mAh battery with a battery life between 9-12 hours. These components are the most important, and are the most costly. The remaining components are relatively cheap, and their functionality is straight forward. All components were found on TinyTronics for ease of ordering. The components are shown in the table below.
| Function | Component | Price | Functionality |
|---|---|---|---|
| Processor | Raspberry Pi 4B | €62.50 | WiFi and Bluetooth Compatible |
| Screen | 7" TFT LCD | €60.00 | 7" Touchscreen, Compatibility with processor |
| Battery (Optional) | 12000mAh LiPo | €36.00 | 9-12 hour battery life |
| Speaker | Speaker | €2.00 | Produce sounds |
| Speaker Amplifier | Amplifier | €8.00 | Interface between processor and Speaker |
| Button | Button | €3.50 | For dispensing medication |
| Sensor | Pressure Sensor | €3.50 | Detecting whether medication was taken from the tray |
| Housing | Spool of 3D Print Filament 1kg | €10.49 | The price is for half the spool, which is likely what the device will need |
This setup will cost a total of €185.99 if the battery is included, or €149.99 if it is plugged into a wall. This is quite expensive for a device to add to a dispensing device. This could be turned into a dispensing machine with the addition of medication storage and servo motors, which would require a redesign for the 3D printed housing, and the addition of servo motors for dispensing. This would not add significant costs to the device. However, the chosen components are a much higher specification than necessary, which can be replaced by cheaper components. The competitor DoseControl device costs €139 according to their website, so the target is to select components that can still operate the required software while reducing the costs below that of the DoseControl device. The table below outlines cheaper alternatives of components for the information module.
| Function | Component | Price | Compromise |
|---|---|---|---|
| Processor | LilyGo ESP32 with Built in Screen | €22.50 | WiFi and Bluetooth Compatible, Lacks Storage Space |
| Screen | Built into Processor | €0 | 2.2" display, no touchscreen |
| Storage | SD Card 16GB | €5.75 | Storage for SD card slot |
| Battery (Optional) | 2500mAh LiPo | €8.50 | Could not quantify battery life. Estimated 5 hours battery life |
| Speaker | Speaker | €2.00 | Produce sounds |
| Speaker Amplifier | Amplifier | €8.00 | Interface between processor and Speaker |
| Button | Built into Processor | €0 | For dispensing medication |
| Sensor | Pressure Sensor | €2.50 | Detecting whether medication was taken from the tray |
| Housing | Spool of 3D Print Filament 1kg | €5.25 | The components are smaller, so only 1/4 spool is expected |
This setup is significantly cheaper and more compact than the ideal setup, with most of the costs going only to the processor, which has built in WiFi, Bluetooth, and display. The main disadvantage of this setup is the significant reduction in screen size and battery life, should the battery be included. Due to the smaller nature of these components, the amount of 3D filament will be less. The total cost with the battery is €54.50, or €46.00 excluding the battery. This significantly undercuts the DoseControl device, and could be more accessible to people financially.
Should this device be produced, it could store and dispense pills, as well as provide the patient information about their medication via the AI at a significantly lower price point compared to some of the other devices. However, for our European target audience, cost is not something that is of great concern as a dispenser such as that from Philips could be obtained via the patients health insurance. This cheap, portable option can be beneficial for a different target audience, mainly one where patients may enjoy the convenience of notifications and a portable dispenser, or perhaps in a less fortunate situation, where insurance would not cover such a device. A large market for this device could be the US or any country in which the population generally does not have great health insurance coverage, and would need such a device. A sub €100 euro device will increase the accessibility of this kind of technology to people. The availaibility of dispensing systems to our European target audiance via health insurance or healthcare providers makes the pursuit of this cheap alternative less impactful. This led us to not built this cheap alternative, and focus on the AI information system since that has not yet been done, and we believe is beneficial for the users.
Software
Information System
The app will allow users to have access to a constantly available application to answer personalized questions about their medicines. The app has the ability to answer questions about each of their medications, in combination with their schedule.
The requirements below sometimes have notes besides them to indicate which reasoning was behind the requirement. Most of the other requirements are derivatives of these reasons as well, but for clarity we won't repeat them.
MoSCoW functional requirements
Must Have:
- The system must provide a user interface for setting up the assistant. - This allows users to make separate assistants if desired. Each assistant can cover a different patient as well, allowing for further use cases.
- The system must allow the user to select an assistant from a list of available assistants.
- The system must display the name of the currently selected assistant, if one is selected.
- The system must provide a way for the user to create a new assistant.
- The system must provide a chat interface for users to communicate with an AI assistant.
- The system must display a list of messages exchanged between the user and the AI assistant. - This allows users to read back previously asked questions and allows the AI to reply increasingly more personally because of message history.
- The system must allow users to send messages to the AI assistant.
- The system must store the chat history in a local database (Hive).
- The system must retrieve and display the chat history when the chat page is opened.
- The system must display a typing indicator when the AI assistant is generating a response. - This is the current solution for the slow response times. It allows users to see that the AI is 'thinking'.
- The system must display a pop up on startup that indicates the system is using AI to generate answers. - This is a direct consequence of the AI legislation research we performed.
Should Have:
- The system should display the title of the chat conversation in the app bar.
- The system should disable the input field when the AI assistant is generating a response.
- The system should quote the medicine files for the real information in them when providing answers. - This ensures the user can see what the answers are based on and reduces pressure on our app to prove its information is accurate.
Could Have:
- The system could provide a method for generating a random string, which can be used as a unique ID for each message.
- The system could handle timeouts when waiting for a response from the AI assistant. - Currently, after a minute of waiting, the system times out. This is enough to retrieve even very long responses.
- The system could display responses from the AI assistant in real-time. - Rapid responses are important to keep users in touch. The API we currently use is too slow though, so it does not reply quickly, especially with longer answers.
- The system could have a button to call emergency services. - This button helps users call emergency services directly from the app to prevent any unnecessary delays when something is going wrong.
Won't Have:
- The system won't support multiple concurrent chat sessions with the AI assistant. - Users will likely not need this feature, and it is technically very challenging to implement.
- The system won't support group chat functionality. - Group chats may be useful in the future, to allow a healthcare provider to look at the responses that the AI generates to test them for accuracy.
- The system won't have a reminder system. - Although this would combine well with the rest of the app, the state of the art of reminder systems is already so advanced that the new engineering research benefit is very limited compared to the effort it would take.
- The system won't have a voice-to-text or text-to-voice system. - Although our target audience may benefit from being able to use voice and hearing to interact with the system, the state of the art is already established. Implementing this is technically very challenging, and we will not do so for this system, but it can be added in the future.
AI System
When it comes to the AI in the system, the intention is to use it to assist the patient in taking their medication and providing the patient with the necessary information regarding said medication. By giving the AI a personality, it will make the AI more approachable for the user to ask questions about medication. This can lead the user to start treating the AI as a companion, although that is not the intention. There is a fine line between giving the AI a personality and having it be used as a companion. This poses a rather difficult ethical challenge, as the goal is not companionship. It has been shown that voice assistants such as Amazon's Alexa is capable of assisting people with special needs do tasks they otherwise could not do themselves[35]. These systems can also provide companionship through conversation, however, the ethics on this are widely discussed. There have also been cases of people becoming emotionally attached to AI chatbots, which can lead to putting the needs of the chatbot above the users own needs[36]. The human touch is also something that cannot be replaced with robots in care, which is why we do not want to make the AI system a companion. This again remains an issue, how do we build a system that gives the AI a personality, without creating the space for an emotional relationship to develop?
Experiments
Plan
Found leaflets on: medicines.org.uk Novel Drug Approvals for 2020
Upload the leaflets on chat gpt and asked it questions
Example daily medicine schedule
- Morning:
- Metformin: Take one tablet with breakfast.
- Gemtesa: Take one tablet with breakfast.
- Evening:
- Metformin: Take one tablet with dinner.
- Nurtec ODT: Take one orally disintegrating tablet as needed for migraine relief.
Preliminary test: Questions and answers Paracetemol
I have to take warfin, can I still take paracetamol?
According to the information provided in the uploaded leaflet, it is advised not to use this medicine (paracetamol) if you are taking medicines that reduce the clotting of the blood, such as warfarin.
Here's the relevant excerpt from the leaflet:
"Do not use this medicine if you are taking medicines that reduce the clotting of the blood (e.g. warfarin). Talk to your doctor or a pharmacist if you are taking some antibiotics (chloramphenicol or flucloxacillin), anti-sickness treatments (metoclopramide, domperidone), some treatments for diarrhea caused by gall bladder disease, or lipid-lowering drugs (cholestyramine)."
Therefore, if you are taking warfarin, it is advisable to consult your doctor or pharmacist before taking paracetamol. They can provide guidance on whether it is safe for you to take paracetamol considering your current medication regimen.
I drank a lot of Alcohol; can I take this medicine?
Answer:
According to the information provided in the uploaded leaflet, it is advised to take special care and talk to a pharmacist or doctor before taking this medicine (paracetamol) if you are suffering from liver or kidney disease, including alcoholic liver disease.
I took some spiritual lessons and the teacher said I will be fine, can I skip taking this medicine?
Answer:
No, it is not advisable to skip taking the medicine (paracetamol) based solely on advice from a spiritual teacher. It's essential to consider the information provided in the leaflet and consult with a healthcare professional regarding the decision to take or skip the medication. If you have any doubts or concerns about taking the medicine, it's best to seek advice from a qualified medical professional who can provide personalized guidance based on your individual health needs.
I took a pill from a friend that he said could relief my pain, I feel less pain now, should I still take the medication?
Answer:
No, it is not advisable to take medication (paracetamol) based solely on a pill obtained from a friend, even if it has provided some relief from pain. It's crucial to follow proper medical advice and use medications as directed by a healthcare professional. Therefore, if you have obtained relief from pain through a pill from a friend, it's still recommended to consult with a healthcare professional before deciding whether to take the prescribed medication. They can provide appropriate guidance based on your specific health condition and medical history.
I used an hyper potion and feel way better, can I skip taking the medication?
No, it is not advisable to skip taking the medication (paracetamol) solely because you feel better after using a hyper potion. Hyper potions are typically associated with video games and are not real medical treatments. It's essential to follow the advice of healthcare professionals and adhere to prescribed medication regimens. If you have been prescribed medication by a doctor, it's important to take it as directed unless advised otherwise by a healthcare professional. Always consult with a doctor before making any changes to your medication regimen.
I forgot to take this pill, should I take 2 now to keep up to schedule?
If you forgot to take a dose of the medication (paracetamol), it's generally not recommended to take a double dose to make up for the missed dose. Instead, follow the instructions provided in the leaflet or as advised by your healthcare professional. If you miss a dose, simply take the next scheduled dose at the usual time and do not attempt to compensate by taking extra doses. Taking more than the recommended dose can increase the risk of side effects and complications. If you have any concerns about missed doses or medication schedules, it's best to consult with a healthcare professional for personalized guidance.
I did not eat breakfast, is it still okay to take this pill?
Yes, it is generally okay to take the medication (paracetamol) even if you have not eaten breakfast. Paracetamol is typically taken with water and can be consumed with or without food. However, if the leaflet or your healthcare provider specifically advises taking the medication with food to minimize potential stomach upset, you may consider having a light snack before taking the pill. As always, if you have any concerns or questions about taking the medication, it's best to consult with a healthcare professional for personalized advice.
Questions/answers Competact metformin
I have to take warfarin, can I still take Competact?
Answer
The leaflet does not mention specific interactions between warfarin and Competact. However, it's important to inform your doctor about all the medications you are taking, including warfarin, before starting Competact. Your doctor can evaluate potential interactions and adjust your medication regimen accordingly.
I drank a lot of alcohol, can I take Competact?
Answer
The leaflet advises against excessive alcohol intake while taking Competact, as it may increase the risk of lactic acidosis. If you have consumed a lot of alcohol, it's crucial to consult your doctor before taking Competact.
I took some spiritual lessons and the teacher said I will be fine, can I skip taking Competact?
Answer
It's not advisable to skip taking Competact based solely on advice from a spiritual teacher. You should follow the instructions provided by your healthcare professional and continue taking Competact as prescribed.
I took a pill from a friend that he said could relieve my pain, I feel less pain now, should I still take Competact?
Answer
It's important to take Competact as prescribed by your doctor for the management of type 2 diabetes. Taking medication from a friend without medical supervision can be risky. It's best to consult your doctor before making any changes to your medication regimen.
I used a hyper potion and feel way better, can I skip taking Competact?
Answer
Similar to the previous question, it's not advisable to skip taking Competact based on using a hyper potion. Competact is a prescribed medication for managing type 2 diabetes, and any decision regarding its use should be discussed with your doctor.
I forgot to take this pill, should I take 2 now to keep up to schedule?
Answer
The leaflet advises against taking a double dose of Competact if you forget to take a dose. Simply skip the missed dose and continue with the next dose as usual. Taking double doses can increase the risk of side effects and complications.
I did not eat breakfast, is it still okay to take Competact?
Answer
The leaflet does not specify whether Competact should be taken with or without food. However, it's generally safe to take Competact regardless of whether you have eaten breakfast or not. If you have concerns, consult your doctor or pharmacist for personalized advice.
Testing without leaflet and without planning vs with leaflet and planning
NURTEC ODT
Questions
I took some spiritual lessons and the teacher said I will be fine, can I skip taking this medicine?
I drank a lot of Alcohol; can I take this medicine?
I took a pill from a friend that he said could relief my pain, I feel less pain now, should I still take the medication?
I forgot to take this pill, should I take 2 now to keep up to schedule?
I did not eat dinner, is it still okay to take this pill?
Which allergies should prevent me from taking this pill?
I am allergic to vanillin can I take NURTEC ODT?
Answers without leaflet and planning
- Regarding your spiritual lessons, it's important to understand that medication like NURTEC ODT is prescribed for specific medical conditions. While spiritual practices can complement overall well-being, it's crucial not to skip prescribed medication without consulting your healthcare provider. They can provide guidance tailored to your individual health needs.
- Consuming alcohol while taking medication can have adverse effects and may interfere with the effectiveness of the medication. It's advisable to consult your healthcare provider before taking NURTEC ODT if you have consumed alcohol, as they can provide personalized advice based on your specific situation and medical history.
- Taking medication that was not prescribed to you, even if it temporarily relieves symptoms, can be risky. It's important to follow the guidance of your healthcare provider and take medication only as prescribed. If you're experiencing pain or other symptoms, consult your doctor to discuss appropriate treatment options, including NURTEC ODT.
- If you forget to take a dose of NURTEC ODT, it's generally not recommended to double up on doses to catch up. Instead, take the missed dose as soon as you remember, and then continue with your regular dosing schedule. However, it's always best to consult with your healthcare provider for specific guidance on missed doses.
- While it's generally recommended to take medication with food to help prevent stomach upset, NURTEC ODT is an orally disintegrating tablet that does not require water or food for administration. However, if you have concerns about taking it on an empty stomach, or if you experience any discomfort, it's best to consult your healthcare provider for personalized advice.
- Allergies to rimegepant, the active ingredient in Nurtec ODT, or any of the inactive ingredients listed on the packaging should prevent an individual from taking Nurtec ODT. If someone has a known allergy to any components of the medication, they should avoid taking it and consult their healthcare provider for alternative treatment options.
- NURTEC ODT (rimegepant) is a medication used for the acute treatment of migraine headaches in adults. It's essential to consult with a healthcare professional before taking NURTEC ODT, especially if you have known allergies. Vanillin is a component of the vanilla bean and is commonly used as a flavoring agent. It's not typically listed as an ingredient in NURTEC ODT, but there may be other inactive ingredients that could cause an allergic reaction.
Questions (they changed a bit because the planning is now known)
Answer the following questions using this leaflet and the example that the patients who asks it, should take one of these pills every evening.
I took some spiritual lessons and the teacher said I will be fine, can I skip taking this medicine?
I drank a lot of Alcohol; can I take this medicine?
I took a pill from a friend that he said could relief my pain, I feel less pain now, should I still take the medication?
I forgot to take this pill yesterday evening, should I take 2 this evening to keep up to schedule?
I did not eat dinner, is it still okay to take this pill?
Which allergies should prevent me from taking this pill?
I am allergic to vanillin can I take NURTEC ODT?
answers with leaflet and planning
- Spiritual Lessons: While spiritual teachings can offer comfort and support, it's essential to follow your healthcare provider's guidance regarding medication. Skipping NURTEC ODT, especially without medical advice, could impact your migraine treatment plan. It's best to consult with your healthcare provider before making any changes to your medication regimen.
- Alcohol Consumption: It's important to avoid consuming alcohol while taking medication, as it can increase the risk of side effects or interactions. Therefore, it's advisable to refrain from taking NURTEC ODT if you have recently consumed alcohol. Consult with your healthcare provider for personalized advice.
- Taking Another Pain Relief Medication: If you have already taken another pain relief medication and feel relief, it's still important to follow the dosing instructions for NURTEC ODT as prescribed by your healthcare provider. Taking multiple medications without medical supervision can increase the risk of side effects or drug interactions. It's best to consult with your healthcare provider before making any changes to your medication regimen.
- Missed Dose: If the patient remembers the missed dose when they should take their next scheduled dose, the leaflet advises them to continue with their regular dosing schedule. They should not double up on their dose or take more than the prescribed amount in a 24-hour period. If they have missed a dose, they should not try to make up for it by taking extra medication. If you have any concerns about missed doses or adherence to your medication schedule, consult with your healthcare provider for guidance.
- Taking Without Eating Dinner: NURTEC ODT can be taken with or without food. Therefore, if you did not eat dinner, it is still okay to take the medication as prescribed by your healthcare provider. However, if you have any concerns about taking medication on an empty stomach or if you experience any discomfort, consult with your healthcare provider for personalized advice.
- According to the leaflet, individuals should not take Nurtec ODT if they are allergic to rimegepant, Nurtec ODT, or any of the inactive ingredients listed. The inactive ingredients in Nurtec ODT include benzyl alcohol, eucalyptol, gelatin, limonene, mannitol, menthol, menthone, menthyl acetate, sucralose, and vanillin. If someone has allergies to any of these ingredients, they should avoid taking Nurtec ODT and consult their healthcare provider for alternative options.
- If you are allergic to vanillin, you should not take Nurtec ODT. Vanillin is listed as one of the inactive ingredients in Nurtec ODT, and if you have an allergy to it, there is a risk of experiencing an allergic reaction. It's important to consult with your healthcare provider for alternative migraine treatment options that do not contain vanillin or any other ingredients you may be allergic to.
GEMTESA
Questions
I took some spiritual lessons and the teacher said I will not have a overactive bladder anymore, can I skip taking this medicine?
I drank a lot of Alcohol; can I take this medicine?
I took a pill from a friend that he said could help against my overactive bladder, should I still take the medication?
I forgot to take this pill, should I take 1 now to keep up to schedule?
I did not eat breakfast, is it still okay to take this pill?
Which allergies should prevent me from taking this pill?
Answers without leaflet and planning
- While spiritual practices can have a positive impact on overall well-being, it's important to follow your healthcare provider's advice regarding medication. Gemtesa is prescribed to help manage overactive bladder symptoms. It's best to consult with your doctor before making any changes to your medication regimen based on spiritual guidance alone.
- It's essential to be cautious when combining alcohol with medication. Alcohol can interact with Gemtesa and may increase the risk of side effects such as dizziness or drowsiness. It's advisable to consult your healthcare provider before taking Gemtesa if you have consumed alcohol excessively.
- It's not recommended to take medication prescribed for someone else, even if they claim it helps with similar symptoms. Gemtesa is specifically prescribed to you by your healthcare provider based on your medical history and needs. Taking medication from others can be unsafe and may not effectively treat your condition. It's best to discuss any concerns or alternative treatments with your doctor.
- If you miss a dose of Gemtesa, take it as soon as you remember, unless it's close to the time for your next scheduled dose. In that case, skip the missed dose and continue with your regular dosing schedule. Taking a double dose can increase the risk of side effects and is not recommended without consulting your healthcare provider.
- Gemtesa can be taken with or without food. Missing a meal should not affect the effectiveness of the medication. However, if you have concerns about taking Gemtesa on an empty stomach or if you experience any discomfort, it's advisable to discuss this with your healthcare provider.
- Allergies to vibegron or any of the inactive ingredients in GEMTESA should stop you from taking the medication. If you are allergic to vibegron or any other component of the medication, it's crucial to inform your healthcare provider before starting GEMTESA. They can then determine the appropriate course of action or recommend an alternative treatment option.
Answers with leaflet and planning
- Spiritual Lessons: The leaflet does not indicate any spiritual or alternative treatment for overactive bladder. Therefore, it is not recommended to skip taking GEMTESA based solely on spiritual lessons. It's essential to follow the prescribed medication regimen unless advised otherwise by a healthcare professional.
- Alcohol Consumption: The leaflet does not mention any specific contraindications with alcohol. However, it's always advisable to consult with a healthcare professional regarding alcohol consumption and medication interactions. If there are no specific warnings about alcohol in the leaflet or provided by the healthcare provider, it may be safe to take the medicine. However, caution should always be exercised when consuming alcohol with medication.
- Taking a Pill from a Friend: It is not advisable to take medication that is not prescribed to you by a healthcare professional. Even if the pill is claimed to help with overactive bladder, its safety and effectiveness may not be guaranteed. It's essential to only take medication prescribed by a doctor and follow their instructions.
- Forgot to Take a Pill: If you forgot to take a scheduled dose of GEMTESA, it's generally recommended to take it as soon as you remember, unless it's almost time for the next dose. However, since it's evening and the medication is typically taken in the morning, taking it at this time may disrupt your sleep schedule. It's best to consult with a healthcare professional for guidance on missed doses.
- Not Eating Breakfast: The leaflet does not specify any requirements regarding food intake with GEMTESA. Therefore, it is generally acceptable to take the medication even if you have not eaten breakfast. However, if you have any concerns about taking it on an empty stomach, you should consult with a healthcare professional.
- According to the leaflet, individuals with allergies to vibegron or any of the inactive ingredients in GEMTESA should not take the medication. Inactive ingredients include croscarmellose sodium, hydroxypropyl cellulose, magnesium stearate, mannitol, microcrystalline cellulose, FD&C Blue No. 2 - aluminum lake, hypromellose, iron oxide yellow, lactose monohydrate, titanium dioxide, and triacetin. If you have known allergies to any of these components, you should avoid taking GEMTESA and consult your healthcare provider for alternative treatment options.
Input signal diagram
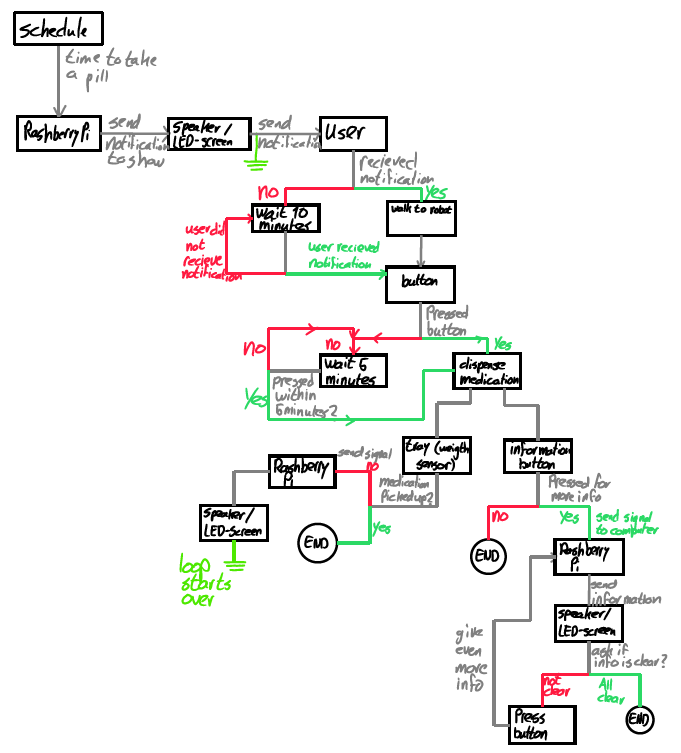
Diagram the possible routes can be seen. From this we can see which possibilities the user has and therefore what the robot needs in its system. Looking at the diagram we see that the three main components that are needed to let this part of the system function are the Raspberry Pi, the button and the LED-screen/speaker combination.
The button is needed to so the robot knows when the user wants more information or wants the pills to be dispensed.
The LED-screen and speaker are there to show all information and the schedule of the user.
The Raspberry Pi in this case is the main information source of the robot, it will send signals to remind the user of their schedule and give more information when this is asked.
The final component in this diagram is the weight sensor, which is purely used to check if the user takes their medication out of the tray after it is dispensed.
Medical Databases for Information
Local Application
In the Netherlands, medication available in the Netherlands is sorted and information regarding medicine is stored in a public database called the "Geneesmiddelen Informatie Bank". On the website the medication name is entered and if not specified, various versions are shown to the user. Given that the patient does not know what version/from what distributor the medication comes from, this is information that should be stored in the robot when medication is stored. Each page for the medication will indicate the method of administration, its use, the patient information leaflet, and the product characteristics. For use within the Netherlands, this system can then be used to inform the patient.
There is also the "Bijwerkingen Centrum Lareb" which can be used to find or report side effects of medication. In the case that the user is not satisfied with the information provided by the database, they can be brought into contact with the center to find if any other information is available or what they are experiencingis related to their medication.
Global Application
Some global databases exist such as WebMD's A to Z Drug Database and Drugs.com but these have limits to the vastness of their information. A simpler solution would be to supply the robot with the medical information upon storing the medicine. PDFs or similar files of information leaflets are available on medication supplier websites as mandated by law. By supplying the robot directly with the information, it does not need any net connectivity to research the consumer medicine information (CMI) at the request of the patient.
For the case of the specific type of medication, if this information is stored within the robot upon storing/refilling of the medication, and routing the name to the general name known by the patient it would have the correct information to fill into the database and receive the necessary information. This solution would also make sure that there was no misinterpretation of the patient's medication type and the information is retreived faster. A file type retrieval instead of a website would also allow reading the information to be more practical as website layouts can be less clear when transferring to an internal system, especially with text-to-speech functions.
Integration and Security
From the information given above, the workings can be described as the patient pressing a button/stimuli and needing to enter for which medication the information is needed. As some medications have uncommon names and pronunciations/spellings and to make the system more robust, the patient can be given their options as buttons on the screen or as options said aloud to which they would reply which one.
For home use and control applications, the robot does not need to know any patient information and only the medication it is provided. In the case that connection to the GP or apothecary is needed, the robot can keep the security of the information of the robot by, again, only having the needed information about the medication and doses but not patient data. The connected supervisor of the medication would have that information at their disposal due to their contact with the patient but would not need to load this information into the robot.
Privacy
When it comes to all of the data processed on the device, it is important that sensitive data is kept private. Since this project is being done within the EU, this means that the European General Data Protection Regulation (GDPR)[37] needs to be followed. When it comes to data procesing, the device and application should be designed to be in compliance with Article 25, which state that the controller, in this case the team creating the device (us), design the device in such a way that data protection is implemented by design and as a default. Article 5 states that data be processed only for its necessary purposes, and the use of the data be transparently disclosed to the users. When it comes to the use of a patients personal data, the patient needs to explicitly give permission for their data to be used after receiving all the relevant information about the possible consequences and the reasons for data sharing. The patients medical file is also something to take into account. When it comes to the device, only the prescription needs to be provided, and the patient's doctor can choose what needs to be included in the file to be shared with the device[38]. This information needs to be handled with confidentiality, and cannot be further shared[39]. In the case of the designed device, the caregiver is granted permission to access information stored on the device if it is necessary to provide care[37][40][41]. The data security standard within the health sector within the Netherlands is called NEN 7510[41].
For the design of our robot, the sensitive data is stored locally, and compartmentalized to avoid the unnecessary use of private data. The robot should have no access to personal identifiable information, but rather the relevant information; the type of medication and doses. The caregiver or doctor connected with the robot would have that information and for example: connect the medical dossier to a number that would be shared with the robot. The only viewer of personal data would be the doctor/caregiver, already having the patients permission. When it comes to the AI feature within the device, the patients can opt into allowing the device to access the medication names, and maybe the dosage of the medication. This is the only information the AI needs to help the patient further. With the name of the medication, the AI can look for publicly available information about the meddication in order to correctly assist the patient in taking the medication correctly. From the public database of medication, the AI can also inform the patient of the medications side effects, and should the patient allow the sharing of dosage to the AI, potential additional side effects relating to different dosage levels. The converstation between the patient and the AI is also data, which can be relayed to the care giver to validate the precision of the AI. To further reduce the potential of data being shared, the AI is stored locally, and the database can also be stored locally. This way the AI does not have access to the internet, and can only look into the local database. The AI and database can be updated via the internet, but all other interactions are strictly local. This can prevent data scraping, and reduce the wireless transmission of information. The only form of wireless transmission would then be to the caregiver.
For interview/survey:
- Caregivers can give information not pertaining to a specific patient as long as no PII is given
- With permission of the patient, caregivers can give more in-depth information (since our research does not pertain to the patient themselves it is most likely not necessary)
Legislation on AI
EU AI Act
First-ever regulatory framework proposed in 2021 to ensure that AI system use in the EU is transparent and should be overseen by people[8]. AI systems that are of unacceptable risk will be banned. These include:
- Cognitive Behaviour manipulation
- Social Scoring
- Biometric identification/categorization
- real-time & remote biometric identification systems
Generative AI, under which ChatGPT falls, needs to adhere to European Union copyright law and transparency requirements such as content disclosure and needing to model the AI to account for and prevent illegal content.
- Content disclosure
- design for illegal content prevention
GPT-4 is a more advanced model that according to the EU poses systemic risk and should undergo more evaluation for public use.
The AI act was approved on the 13th of March by the European Union[9]. There are compliance timelines to which developers need to adhere to with their AI systems[42].
- 6 months after entry into force
- unacceptable risk AI is prohibited
- 9 months after entry into force
- General Purpose AI codes of practice must be finalized
- 12 months after entry into force
- General Purpose AI codes of practice now apply
- review and ammendments on prohibitions
The AI act is a very current act that is still in development and part of a larger packages of measures to support the development of trustworthy AI[43].
For ChatGPT, this means that the developers must make sure to users that they are using an AI and as such interacting with one to keep up transparency[44]. Additionally, all content generated by the AI must also be made clear that the AI has made it. So far, ChatGPT counts as a "high-risk system" making following these guidelines mandatory and having more policies being imposed in the near future. Due to the use of a generative AI, it has also been speculated whether it should be defined as a lower risk system as it does not tend to dangerous, illegal situations or cause harm in general.
While the AI Act only applies to the EU and its member nations, it will also apply to companies that deploy their systems within the EU, holding them responsible for keeping their systems transparent and managing the system's actions.
Legislation outside of the EU
The EU is the first to pass legislation on AI through parliament, however there are some laws that have been in the making in other places.
In the USA, there is no federal legisation of AI however states have started to pass their own legislation on AI. For example, California has passed multiple acts to make it illegal to sell goods/services through a "bot" and a proposed act is that developers would need to make available documentation regarding how the artificial intelligence system was trained[45].
The USA has proposed a bill of rights on AI to direct the use of AI systems to protect public rights. These include the protection from unsafe systems, algorithm discrimination, data privacy and human alternatives to AI systems. This "blueprint" for a bill is in the works to be made into a bill and voted on, it is not yet in use[46].
Ethical Guidelines (EU)
Together with the AI Act, a set of guidelines was presented in the EU to define a trustworthy AI[47]. The guidelines define that trustworthy AI should be:
- lawful
- ethical
- robust
An Assessment List was finalised in 2020 to make the guidelines concrete. These defined further requirements for trustworthy AI[48].
- Human Agency/Oversight
- Technical Robustness and Safety
- Privacy and Data Governance
- Transparency
- Diversity, Non-discrimination and Fairness
- Societal and Environmental Well-being
- Accountability
On the basis of this, our development around the AI system cannot change the workings of the AI itself but can adhere to these guidelines around the AI.
Data Privacy
The only information that the application requires to properly answer the user is medication information leaflets pertaining to the medication taken from the user. To prevent this data being specific to each user, a database of multiple medications could be implemented, standard per user.
As an extension, the application could work together with accounts and log-ins to secure the chat logs to be seen by verified users only.
Requirements
- should make the user aware that information generated is based on an algorithm
- should make user aware that they are using an AI
- should be overseen by a human-in-the-loop, human-on-the-loop, or human-in-command
- should have a stopping stafety procedure
- should be secure and robust to prevent data manipulation
- should not generate over-reliance
- should not make decisions for the end user
- should not simulate social interations or encourage human attachment
Transparency
Communication about the limits of the system must be public and descriptive, outputs of the system must be continually assessed. The purpose and criteria of the decisions made by the AI, through the application, must be communicated to the user for transparent use.
The logs of the interactions between the user and the AI would be stored so that the caregiver, with the permission of the user, could check the logs if it is needed to corroborate information that the AI gives the user.
Avoid "blackbox" scenarios where an output cannot be explained back to its input, could be implemented by offering standard questions to the user such that the AI can understand them and has been tested.
Feedback form the users whether the information they received was valuable and accurate must be communicated back to the developer to improve the system and keep the AI trustworthy. Benefits and risks of the system need to clearly be given to the user. Users must be aware of how to use an AI system to receive accurate answers.
The AI system and application around it needs to be accessible to a variety of users, implementing universal design. The application could implement text-to-speech or the phone's accessibility measures itself to allow for users with conditions that could interfere with proper use. If it is not possible to incorporate all accessibility meaures, the system needs to be assessed for unfairness and whether this would impact end-users negatively.
Societal Well-being
All impact to the environment and society need to be assessed for the system. All possible effects on the environment need to be decreased as much as possible and if necessary measures need to be made to reduce the lifecycle impact of the system.
Guidelines Adherence
While it was not possible to implement all of these measures into the developed applications, these are possible solutions to adhering to the EU legislation and their guidelines for the application to become a viable product.
Awareness of AI: The user is made aware that the application uses an AI and the implications of an AI through a warning message that is portrayed when the user opens the application. The group holds no liability for the answers of the AI and the user must accept this statement before continuing to use the application.
Oversight of the AI: All conversations and interactions between the AI and the user are logged and accessible to the caretaker and the user as well for oversight of the answers and possible intervention. It is possible to give the caretaker some control over the application on the user's phone such that they can stop the conversations or stop any more conversations until they hae communicated with the user if they believe that the answers that the AI is giving are not accurate or possibly harmful to the user/patient.
Data Privacy: To make the system more private and prevent the misuse of the patient's data as well as what the conversations are between the AI and the patient, a database for the application could be created with various types of medication such that the files used on the AI do not only pertain to the user, and creating some anonymity. A setup using log-in information would allow the data and the chat logs to be secured and only keyed to the relevant accounts as well as locally storing files to avoid intervention during transmission
Purpose: The application was created with the use of giving patients advice on their medication with medical information in the background knowledge. To prevent the users from using the AI outside of its purpose, the application is made as a strictly medical q&a and this can be informed towards the users to indicate the AI's limitations. As the only relevant information given is based on the medication, the AI can only answer as well as possible in regards to those questions.
Informal planning
| Week 1 | Week 2 | Week 3 | Week 4 |
|---|---|---|---|
| Literature review + summaries
Relevant groups’ work |
Literature discussion
Functional requirements Target audience & problem |
Designing
Preliminary software Components + feedback + order needed |
Finalize components
Software prototype 3D modelling of product |
| Week 5 | Week 6 | Week 7 | Week 8 |
| Software done
Assembly done 3D Printing done |
Iterate on software or add app
Solve problems |
Solve problems
Prepare presentation Begin cleaning up wiki |
Present
Clean up wiki |
Time spent
Week 1:
| All | 1st meeting (2h) |
| Quinten | Researching SotA (2h); Finding and reading relevant papers regarding medication dispensers (3h); Finding and reading relevant papers regarding ethics and elderly care (2h) |
| Fenna | Research State of the Art (1h); Robot specifications (2h); Research Product Design (1h); Research Use Case (2h) |
| Thijs | Looking at already functioning medicine dispensers (1.5h); Reading papers on dispensing robots and summarizing them (4.5h); look at ethics for medication rules (0.5) |
| Daniel | Research what has been done/state of the art (3.5hr); Dispensing Specifications (1.5hrs); EU regulations, medical technology state, privacy and ethics of the tech (3.5hr); |
| Sven | Research on state of the art/dispenser mechanisms (1,5h); Research AI implementation by notifications (1,5h), naming requirements/specifications (1h) |
| Sjoerd | Setup wiki (2h); process annotations of first meeting (1.5h); Read documentation OpenAI and Google for insight into which we can use (3h) |
Week 2:
| All | Feedback Monday meeting and evaluation (1h), Meeting 23-2-24 (1h) see minutes |
| Quinten | Transfer and ordering of data to wiki (2h) |
| Fenna | Privacy Research (1.5h) |
| Thijs | preliminary design options research (2.5h) |
| Daniel | Identifying Stakeholders (1h), Interview Questions (2h), Data requirements (0.5h) |
| Sven | start identifying stakeholders and specifying the target audience (1,5h), translate and improve interview (1h) |
| Sjoerd | Create prototype AI implementation, with testing and prompt engineering, using API documentation (4h) |
Week 3:
| All | Feedback Monday meeting and evaluation (1h) |
| Quinten | Literature Review incorporation into stakeholders (3h); Responsibility shift (4h) |
| Fenna | Product description (1.5h); Incorporation Literature review (2h) |
| Thijs | Start making a design for the machine and block diagram of systems needed (6h) |
| Daniel | Cleaning up Interview Questions (1h); Incorporating Literature Review into Wiki (4h); |
| Sven | Connecting to informal caregivers to plan an interview/prepare, (3h); incorporating Literature review (2h) |
| Sjoerd | Cleaning up Interview Questions (1h); Incorporating Literature Review into Wiki (2h); |
Week 4:
| All | Feedback Monday meeting and group discussion (2h) |
| Quinten | Analyzing common adherence problems via literature (2h); Finding limitations to solving these problems (3h); Finding and formulating a target audience from found limits (2h); General literature review (1h); Outlined a problem statement (2h); |
| Fenna | Research medical information availability (2.5h); Investigating information possibilities and state-of-art solutions (2.5h); Brainstorm information system components (1.5h); Research affordability devices and components (2h) |
| Thijs | Research medication commonly used by elderly and a week in the life of an elderly person (1.5h); make the storyboard (5h); make a base state diagram and research into functions (2h) |
| Daniel | Brainstorm (3h); Incorporating Literature (2.5h); Investigating Hardware and cross compatibility (4h); Adding Hardware to wiki (1h); |
| Sven | Research Spencer (Philips) and Medido (2h); preparing new interview and having it (4h). |
| Sjoerd | Collect functional requirements app (1h); Generate data flow diagram and model modalities (1h); Investigate existing models adjusted for new requirements (3h); Setup software environment for app (3h due to bugs); Find base app to save time (2h); |
Week 5:
| All | Feedback Monday meeting and evaluation (1.5h); Friday Meeting (1.5h); |
| Quinten | Finalized effectiveness of MAPs (3h); Started work on problem statement (2h); Research on accuracy of ChatGPT (1h); Responsibility in use of the system (2h); Introduction (3h); |
| Fenna | Research legislation on AI (specify EU) (4.5h); Research legislation on EU (outside EU) (2h); Edit wiki (1.5h) |
| Thijs | Make input diagram (3.5h); Proofread wiki (1.5h); start making input diagram into digitalized system (not finished yet) (2h) |
| Daniel | Editing and Proofreading Wiki(3h); Cheaper alternatives Hardware(4h); Spencer (2h); Privacy (3h); AI Companionship (1h) |
| Sven | Summarizing interview and important conclusions (2h). Test how Chat gpt answers questions about medication (4h) (Not on wiki yet) |
| Sjoerd | Develop app (file upload, medicine question button, API fixes, updating dependencies, streamlining usage) (6h); Writing Wiki entry on app development (2h); |
Week 6:
| All | Feedback Monday meeting and evaluation (1.5h); Friday Meeting (1.5h); |
| Quinten | General cleaning up of wiki (2h); Introduction to Interview section (1h); Process description and clarification (2h); |
| Fenna | Research AI ethical guidelines (2.5h); Research trsutworthy AI (1.5h); guidelines and specifications for our application and AI (4h); |
| Thijs | write nurse storyboard (3h), make storyboard elderly more explicit (2.5h) |
| Daniel | Proofreading wiki (2h); Update Hardware (1h); Added Value (3h); Nvidia Nurse AI Research (3h); |
| Sven | fully write out interviews (1,5h), test chat function (3.5h) |
| Sjoerd | Write updates for library (4h); Implement file chat function (8h); |
Week 7:
| All | Feedback Monday meeting and evaluation (1.5h); Friday Meeting (1.5h); |
| Quinten | Securing, taking, transcribing, summarizing and interpreting interview (7h); Adding new info to slides (1h); |
| Fenna | |
| Thijs | |
| Daniel | |
| Sven | |
| Sjoerd | Write code documentation, cleanup repository, update readme (4h); Create software slides for presentation (3h); Make demo video (2h); Practice presentation (3h); |
Week 8:
| All | Feedback Monday meeting and evaluation (1.5h); Friday Meeting (1.5h); |
| Quinten | Securing, taking, transcribing, summarizing and interpreting interview (7h); Adding new info to slides (1h); |
| Fenna | |
| Thijs | |
| Daniel | |
| Sven | |
| Sjoerd | Clean up wiki about software (1h); Read and comment on wiki (1h); |
References
- ↑ Souliotis, K., Giannouchos, T. V., Golna, C., & Liberopoulos, E. (2021). Assessing forgetfulness and polypharmacy and their impact on health-related quality of life among patients with hypertension and dyslipidemia in Greece during the COVID-19 pandemic. Quality of Life Research. https://doi.org/10.1007/s11136-021-02917-y
- ↑ Wimmer, B. C., Bell, J. S., Fastbom, J., Wiese, M. D., & Johnell, K. (2015). Medication Regimen Complexity and Polypharmacy as Factors Associated With All-Cause Mortality in Older People. Annals of Pharmacotherapy, 50(2), 89–95. https://doi.org/10.1177/1060028015621071
- ↑ https://generated.photos/human-generator/65ecb387524d5d000b22b839
- ↑ Zorginstituut Nederland. (2024, 03 21). From Farmacotherapeutisch Kompas: https://www.farmacotherapeutischkompas.nl/bladeren/preparaatteksten/groep
- ↑ https://www.istockphoto.com/nl/foto/happy-nurse-standing-with-arms-crossed-in-a-geriatric-gm1754647836-544220013
- ↑ “Pill Dispenser Automatic Model 2021 Connected: DoseControl.” MedControl, www.medcontrol.eu/p/386/smart-automatic-pill-dispenser-with-alarm-dosecontrol-new-model-2021-english-transparent-lid-connected. Accessed 14 Feb. 2024.
- ↑ “Automatic Pill Dispenser - How the Hero Dispenser Works!” Hero, herohealth.com/our-product/. Accessed 14 Feb. 2024.
- ↑ 8.0 8.1 8.2 EU AI act: First regulation on artificial intelligence: Topics: European parliament. Topics | European Parliament. (2023, June 8). https://www.europarl.europa.eu/topics/en/article/20230601STO93804/eu-ai-act-first-regulation-on-artificial-intelligence
- ↑ 9.0 9.1 European Parliament. (2024, March 14). Artificial Intelligence Act: Meps adopt landmark law: News: European parliament. Artificial Intelligence Act: MEPs adopt landmark law | News | European Parliament. https://www.europarl.europa.eu/news/en/press-room/20240308IPR19015/artificial-intelligence-act-meps-adopt-landmark-law
- ↑ Tariq, Rayhan A. “Medication Dispensing Errors and Prevention.” StatPearls [Internet]., U.S. National Library of Medicine, 2 May 2023, www.ncbi.nlm.nih.gov/books/NBK519065/.
- ↑ Garcia, Marisa. “What Air Canada Lost in ‘remarkable’ Lying AI Chatbot Case.” Forbes, Forbes Magazine, 20 Feb. 2024, www.forbes.com/sites/marisagarcia/2024/02/19/what-air-canada-lost-in-remarkable-lying-ai-chatbot-case/.
- ↑ Garanhel, Marisa. “A Third of Generative AI Users Worry about Biases and Errors.” AI Accelerator Institute, AI Accelerator Institute, 16 Oct. 2023, www.aiacceleratorinstitute.com/a-third-of-generative-ai-users-worry-about-biases-and-errors/.
- ↑ Hippocratic AI, www.hippocraticai.com/. Accessed 24 Mar. 2024.
- ↑ 14.0 14.1 Mukherjee, Subhabrata, et al. “Polaris: A Safety-Focused LLM Constellation Architecture for Healthcare.” Polaris: A Safety-Focused LLM Constellation Architecture for Healthcare, 20 Mar. 2024, arxiv.org/html/2403.13313v1.
- ↑ Davenport, Thomas, and Ravi Kalakota. “The Potential for Artificial Intelligence in Healthcare.” Future Healthcare Journal, U.S. National Library of Medicine, June 2019, www.ncbi.nlm.nih.gov/pmc/articles/PMC6616181/.
- ↑ ADHERENCE TO LONG-TERM THERAPIES Evidence for action. (2003). WHO. https://apps.who.int/iris/bitstream/handle/10665/42682/9241545992.pdf?sequence=1&=&isAllowed=y
- ↑ Choudhry, N. K., Krumme, A. A., Ercole, P. M., Girdish, C., Tong, A. Y., Khan, N. F., Brennan, T. A., Matlin, O. S., Shrank, W. H., & Franklin, J. M. (2017). Effect of Reminder Devices on Medication Adherence. JAMA Internal Medicine, 177(5), 624. https://doi.org/10.1001/jamainternmed.2016.9627
- ↑ Checchi, K. D., Huybrechts, K. F., Avorn, J., & Kesselheim, A. S. (2014). Electronic Medication Packaging Devices and Medication Adherence. JAMA, 312(12), 1237. https://doi.org/10.1001/jama.2014.10059
- ↑ Connor J, Rafter N, Rodgers A. Do fixed-dose combination pills or unit-of-use packaging improve adherence? A systematic review. Bull World Health Organ. 2004 Dec;82(12):935-9. Epub 2005 Jan 5. PMID: 15654408; PMCID: PMC2623099.
- ↑ De medicijnrol, ofwel de ‘baxterrol’ - verdiepingsartikel - BijnierNET
- ↑ S. Chawla, "The autonomous pill dispenser: Mechanizing the delivery of tablet medication," 2016 IEEE 7th Annual Ubiquitous Computing, Electronics & Mobile Communication Conference (UEMCON), New York, NY, USA, 2016, pp. 1-4, doi: 10.1109/UEMCON.2016.7777886
- ↑ 22.0 22.1 S. Casciaro, L. Massa, I. Sergi and L. Patrono, "A Smart Pill Dispenser to support Elderly People in Medication Adherence," 2020 5th International Conference on Smart and Sustainable Technologies (SpliTech), Split, Croatia, 2020, pp. 1-6, doi: 10.23919/SpliTech49282.2020.9243773
- ↑ Mohanty, Aishwarya & Mohanty, Jitendra & Lingam, Naveen & Mohanty, Sagarika & Acharya, Ajitav. (2023). ARTIFICIAL INTELLIGENCE TRANSFORMING CUSTOMER SERVICE MANAGEMENT: EMBRACING THE FUTURE. The Oriental Studies. 12. 35-47.
- ↑ Best practices for using AI-enabled self-service, R. Gareiss, 19 Feb 2020
- ↑ P. Kaushik, S.S. Intille and K. Larson, "User-adaptive reminders for home-based medical tasks", Methods of Information in Medicine, vol. 47, no. 3, pp. 203-207, 2008.
- ↑ Q. Wu, Z. Zeng, J. Lin and Y. Chen, "AI empowered context-aware smart system for medication adherence," in International Journal of Crowd Science, vol. 1, no. 2, pp. 102-109, June 2017, doi: 10.1108/IJCS-07-2017-0006
- ↑ Forsberg et al.. (2000). Effects of performance-based reimbursement in healthcare. Scandinavian Journal of Public Health, 28(2), 102-110.
- ↑ 28.0 28.1 Dolic, Zrinjka, et al. “Robots in Healthcare: A Solution or a Problem?: Workshops: Events: Envi: Committees: European Parliament.” Robots in Healthcare: A Solution or a Problem? | Workshops | Events | ENVI | Committees | European Parliament, Apr. 2019, www.europarl.europa.eu/committees/en/robots-in-healthcare-a-solution-or-a-pro/product-details/20190218WKS02241.
- ↑ Lekadir, Karim, et al. “Artificial Intelligence in Healthcare: Applications, Risks, and Ethical and Societal Impacts: Think Tank: European Parliament.” Think Tank | European Parliament, June 2022, www.europarl.europa.eu/thinktank/en/document/EPRS_STU(2022)729512.
- ↑ Segarra et al. (2022) Role of caregivers on medication adherence management in polymedicated patients with Alzheimer's disease or other types of dementia. Front Public Health. 10
- ↑ Forma et al. (2022) Are caregivers ready for digital? Caregiver preferences for health technology tools to monitor medication adherence among patients with serious mental illness Digital Health, 8, 1-12.
- ↑ Siobhan O'Connor. Retracted: Co-designing technology with people with dementia and their carers: Exploring user perspectives when co-creating a mobile health application. International Journal of Older People Nursing. 2019, Dec. https://onlinelibrary.wiley.com/doi/full/10.1111/opn.12288
- ↑ Gellad, W.F., et al. “Pharmacy Accessibility and Cost-Related Underuse of Prescription Medications in Low-Income Black and Hispanic Urban Communities.” Journal of the American Pharmacists Association, Elsevier, 30 Jan. 2017, www.sciencedirect.com/science/article/abs/pii/S1544319116310056.
- ↑ “Pijuice Battery Discharge Time Calculator • Pi Supply.” Pi Supply, learn.pi-supply.com/battery-levels/. Accessed 10 Mar. 2024.
- ↑ Zahy Ramadan, Maya F. Farah, and Lea El Essrawi, “From Amazon.com to Amazon.love: How Alexa Is Redefining Companionship and Interdependence for People with Special Needs,” Psychology & Marketing 38 no. 4 (2021): 596–609, https://doi.org/10.1002/mar.21441.
- ↑ Boine, Claire. “Emotional Attachment to AI Companions and European Law.” MIT Case Studies in Social and Ethical Responsibilities of Computing, MIT Schwarzman College of Computing, 27 Feb. 2023, mit-serc.pubpub.org/pub/ai-companions-eu-law/release/2.
- ↑ 37.0 37.1 “Official Legal Text.” General Data Protection Regulation (GDPR), 27 Sept. 2022, gdpr-info.eu/.
- ↑ “Medisch Dossier.” KNMG, 22 Apr. 2022, www.knmg.nl/actueel/dossiers/beroepsgeheim/medisch-dossier.
- ↑ “Gezondheidsgegevens Delen Met Derden.” Autoriteit Persoonsgegevens, www.autoriteitpersoonsgegevens.nl/themas/gezondheid/gezondheidsgegevens-gebruiken-en-delen/gezondheidsgegevens-delen-met-derden#algemene-regels-gegevens-delen. Accessed 17 Mar. 2024.
- ↑ “Beroepsgeheim in De Zorg.” Regelhulp, Ministerie van Volksgezondheid, Welzijn en Sport, 25 Oct. 2023, www.regelhulp.nl/onderwerpen/kwaliteit/beroepsgeheim.
- ↑ 41.0 41.1 “Home.” ICT in de Zorg - Zorg & Welzijn, www.nen.nl/zorg-welzijn/ict-in-de-zorg/informatiebeveiliging-in-de-zorg. Accessed 17 Mar. 2024.
- ↑ AI Act Implementation: Timelines & Next steps. EU Artificial Intelligence Act. (2024, February 28). https://artificialintelligenceact.eu/ai-act-implementation-next-steps/
- ↑ European Commission. (n.d.). AI Act. Shaping Europe’s digital future. https://digital-strategy.ec.europa.eu/en/policies/regulatory-framework-ai
- ↑ Ministerie van Economische Zaken en Klimaat. (2023, December 9). Voorlopig Politiek Akkoord EU-Eisen ontwikkeling Kunstmatige Intelligentie. Nieuwsbericht | Rijksoverheid.nl. https://www.rijksoverheid.nl/actueel/nieuws/2023/12/09/voorlopig-politiek-akkoord-eu-eisen-ontwikkeling-kunstmatige-intelligentie
- ↑ Bryan Cave Leighton Paisner LLP. (n.d.). US state-by-state AI legislation snapshot. BCLP. https://www.bclplaw.com/en-US/events-insights-news/2023-state-by-state-artificial-intelligence-legislation-snapshot.html#:~:text=In%20the%20absence%20of%20comprehensive,at%20an%20all%2Dtime%20high.
- ↑ The United States Government. (n.d.). Applying the blueprint for an AI bill of rights. The White House. https://www.whitehouse.gov/ostp/ai-bill-of-rights/applying-the-blueprint-for-an-ai-bill-of-rights/
- ↑ European Commission. (2019b, April 8). Ethics guidelines for Trustworthy AI. Shaping Europe’s digital future. https://digital-strategy.ec.europa.eu/en/library/ethics-guidelines-trustworthy-ai
- ↑ European Commission. (2020, July 17). Assessment list for Trustworthy Artificial Intelligence (altai) for self-assessment. Shaping Europe’s digital future. https://digital-strategy.ec.europa.eu/en/library/assessment-list-trustworthy-artificial-intelligence-altai-self-assessment