PRE2024 3 Group19: Difference between revisions
| (64 intermediate revisions by 5 users not shown) | |||
| Line 29: | Line 29: | ||
|} | |} | ||
==Problem Statement== | ==Problem Statement== | ||
In 2020, 55 million people were diagnosed with dementia worldwide. This number is expected to grow to 139 million people in 2050 | In 2020, 55 million people were diagnosed with dementia worldwide. This number is expected to grow to 139 million people in 2050<ref>''ADI - Dementia statistics''. (z.d.). ADI - Dementia Statistics. <nowiki>https://www.alzint.org/about/dementia-facts-figures/dementia-statistics/</nowiki> | ||
</ref>. Two thirds of people living in care homes have dementia<ref>Sharp S. Home from home : a report highlighting opportunities for improving standards of dementia care in care homes.. Alzheimer's Society; 2007. | |||
</ref>. Dementia is a general term for a syndrome that affects memory, thinking and the ability to perform daily tasks. A common symptom of dementia is agitation. When someone is agitated, they feel irritable and restless. People are uncooperative and have difficulties focusing when feeling agitated. They can also show violent or disruptive behavior and have a lack of impulse control. This negative and dangerous behavior could cause dangerous and unpleasant situations for both people with dementia but also for their family, friends, and staff of care homes. | |||
Research has shown that music can have a positive effect on people with dementia. It can help to use music during therapy sessions with a licensed music therapist. Research also shows that music can help outside of therapy sessions. It can help agitated patients feel more calm and it can have a positive impact on a patients heart rate or blood pressure. | Research has shown that music can have a positive effect on people with dementia. It can help to use music during therapy sessions with a licensed music therapist. Research also shows that music can help outside of therapy sessions. It can help agitated patients feel more calm and it can have a positive impact on a patients heart rate or blood pressure. | ||
Currently, music needs to be played by a caregiver or a therapist; there has to be someone to start the music. But what if there is | Dementia is typically characterized by a disturbance of the higher cortical functions. However, people with dementia can often still remember the lyrics of songs they used to listen to in the earlier stages of life. It seems that the long-term memory for music is often still in tact, even in people in the later stages of dementia and is less affected by the typical metabolic disorders and nerve cell loss. This is the case, because long-term music memory is not located in the hippocampal area, which is were most ordinary memories are stored, but in the supplementary motor cortex, which is responsible for complex motor movements<ref>Rebecca Dahms, Cornelia Eicher, Marten Haesner, Ursula Mueller-Werdan, Influence of Music Therapy and Music-Based Interventions on Dementia: A Pilot Study, ''Journal of Music Therapy'', Volume 58, Issue 3, Fall 2021, Pages e12–e36, <nowiki>https://doi.org/10.1093/jmt/thab005</nowiki> | ||
</ref>. | |||
Currently, music needs to be played by a caregiver or a therapist; there has to be someone to start the music. But what if there is no one present? Then there is no one to play music for a patient when they are stressed or agitated. This is what our project aims to solve. Instead of needing someone to be present, our proposal is that a wearable device will monitor a patient and start playing music when applicable. | |||
So, this project aims to create a well researched design proposal to help agitated dementia patients without needing immediate assistance of a caregiver, by monitoring a patient's stress level and playing music when they are stressed. | So, this project aims to create a well researched design proposal to help agitated dementia patients without needing immediate assistance of a caregiver, by monitoring a patient's stress level and playing music when they are stressed. | ||
==Objectives== | ==Objectives== | ||
The main objective of this research is to find a way to calm dementia patients down when they are feeling stressed. It is quite common for people with dementia to be distressed, which can be caused by feeling disoriented, having unmet needs, as well as many other factors (Coping with distress - Dementia UK | The main objective of this research is to find a way to calm dementia patients down when they are feeling stressed. It is quite common for people with dementia to be distressed, which can be caused by feeling disoriented, having unmet needs, as well as many other factors<ref>Dementia UK. (2025, 21 maart). ''Coping with distress - Dementia UK''. <nowiki>https://www.dementiauk.org/information-and-support/health-advice/coping-with-distress/</nowiki></ref>. It has been found that music interventions lower anxiety levels and generally make patients (and even caregivers) feel more relaxed <ref name=":4" />. That is why music will be implemented in the design to alleviate stress. In order to further assess what we want our design to achieve, we will be using the MoSCoW method. | ||
==== Must have ==== | |||
* A calming effect on the patient | * A calming effect on the patient | ||
* A stress sensor of some kind to determine when the music should be turned on | * A stress sensor of some kind to determine when the music should be turned on | ||
==== Should have ==== | |||
* Music from the patients youth | * Music from the patients youth | ||
* Comfortability (if the stress sensor is wearable) | * Comfortability (if the stress sensor is wearable) | ||
==== Could have ==== | |||
* A calming effect on the caregiver | * A calming effect on the caregiver | ||
* Slowly increase volume to limit the shock | * Slowly increase volume to limit the shock | ||
| Line 57: | Line 60: | ||
* A stress sensor based on sound | * A stress sensor based on sound | ||
==== Will not have ==== | |||
* Scaring the patient by sudden loud music | * Scaring the patient by sudden loud music | ||
| Line 64: | Line 66: | ||
The target users of this design are people with dementia, particularly those in the mid-to-late stages of the condition. Dementia affects cognitive functions such as reasoning, memory, and emotional regulation, making patients more prone to stress, anxiety, and agitation. This has detrimental effects on their well-being. | The target users of this design are people with dementia, particularly those in the mid-to-late stages of the condition. Dementia affects cognitive functions such as reasoning, memory, and emotional regulation, making patients more prone to stress, anxiety, and agitation. This has detrimental effects on their well-being. | ||
It has been found that in the brains of people with Alzheimer's Disease the musical memory regions are largely spared and well-preserved. For this reason, music can be very effective in retrieving musical memories for these people and reducing stress. One study studied the effect of music intervention on patients with severe dementia and found there is a short-term improvement in emotional state <ref name=":2">Ekra EMR, Dale B. Systematic Use of Song and Music in Dementia Care: Health Care Providers’ Experiences. ''J Multidiscip Healthc''. 2020;13:143-151 | |||
<nowiki>https://doi.org/10.2147/JMDH.S231440</nowiki></ref>. Recognition of familiar music was particularly considered as emotionally meaningful for people in the late stages of dementia <ref name=":3">Ting B, Chen DT, Hsu WT, Liang CS, Malau IA, Li WC, Lee SL, Jingling L, Su KP. Does Music Intervention Improve Anxiety in Dementia Patients? A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J Clin Med. 2023 Aug 24;12(17):5497. doi: 10.3390/jcm12175497. PMID: 37685564; PMCID: PMC10488399. | |||
</ref>. | |||
= | |||
</ref>. | |||
Given the cognitive impairments associated with dementia, the design of the aid to measure stress and play music must function autonomously with minimal user input. Furthermore, as most individuals with dementia belong to an older demographic, potential physical limitations should be taken into account. It is essential that the stress sensor is easy to use and imposes minimal physical constraints to ensure comfort and practicality. Potential perceptual limitations are also important to consider. The volume of the device for playing music must be able to be adjusted to an appropriate level. The music should be loud enough for the patient to actually perceive the music, but it should not be too loud, since this could only contribute to the distress. | |||
Another crucial user requirement is the personalization of the aid. Both in the measurement of stress and for the intervention in the form of playing music, personalization is needed. Personalization allows the aid to calibrate to a user's unique stress patterns, ensuring more accurate responses. Furthermore, since music preferences vary from person to person, the system must be capable of playing the specific music that elicits positive emotions for each individual. This personalization is essential for effectively reducing stress levels and providing a soothing experience. | |||
Since the caregivers of people with dementia are often also affected by distress of these individuals, they can be considered secondary users. They play a vital role in setting up and managing the device, selecting appropriate music and monitoring its effectiveness. To avoid adding to their workload, the system must be as simple to use as possible. They might also be the people buying the device so it would be beneficial for us to take their wishes into account (from a marketing perspective). | |||
From our interviews it became apparent that the device is most likely to be a success when used by people still living at home. For people living at nursing residencies the device can only be of use when they are in their own room. Since the music will be played on an external speaker, it is not feasible to use the device in group settings such as the dining hall of a nursing residency. Furthermore, in such group settings, there are always caregivers who can also help calm down the agitated patient, whereas the purpose of this device is to help patients with dementia calm down when there is no one around to immediately help them. Elderly people still living at home are more often in the situation that there are no caregivers around, that is why they are our main target group. | |||
== | == Research == | ||
== Stress Measurement Techniques for Wearable Devices == | === Possible Stress Measurement Techniques for Wearable Devices === | ||
Stress is a physiological and psychological response to external stimuli, influencing various bodily functions such as skin conductance, heart rate and brain activity. Wearable sensors | Stress is a physiological and psychological response to external stimuli, influencing various bodily functions such as skin conductance, heart rate and brain activity. Wearable sensors for monitoring stress are increasingly incorporated in consumer products such as smart watches. However, selecting the right combination of sensors for a wristband involves balancing accuracy, comfort, and practicality. In this section we explore several different stress measurement techniques and evaluate which are the best options to implement in wrist-worn wearables. This way we can make the optimal choice of features to incoporate in our design proposal. | ||
==== Electrocardiography (ECG) - Heart Activity Measurement ==== | ===== Electrocardiography (ECG) - Heart Activity Measurement ===== | ||
ECG measures the electrical activity of the heart, specifically heart rate variability (HRV). A lower HVR often indicates higher stress levels. In order to be able to conduct an ECG, electrodes are placed on the skin, commonly in the form of a chest strap or adhesive patches.<ref name=":0">S. Gedam and S. Paul, "A Review on Mental Stress Detection Using Wearable Sensors and Machine Learning Techniques," in IEEE Access, vol. 9, pp. 84045-84066, 2021, doi: 10.1109/ACCESS.2021.3085502. | ECG measures the electrical activity of the heart, specifically heart rate variability (HRV). A lower HVR often indicates higher stress levels. In order to be able to conduct an ECG, electrodes are placed on the skin, commonly in the form of a chest strap or adhesive patches.<ref name=":0">S. Gedam and S. Paul, "A Review on Mental Stress Detection Using Wearable Sensors and Machine Learning Techniques," in IEEE Access, vol. 9, pp. 84045-84066, 2021, doi: 10.1109/ACCESS.2021.3085502. | ||
| Line 169: | Line 103: | ||
- It is not easily integrated into a wristband due to placement limitations | - It is not easily integrated into a wristband due to placement limitations | ||
==== Photoplethysmography (PPG) - Optical Heart Rate Monitoring ==== | ===== Photoplethysmography (PPG) - Optical Heart Rate Monitoring ===== | ||
PPG uses LED light reflection to measure blood volume changes in the capillaries, indirectly determining heart rate and HRV. An LED-light is shown onto the skin and a sensor measures the amount of light that is reflected back. The more light is reflected back, the lower the blood volume. This technology is widely integrated into smartwatches and wristbands.<ref name=":0" /> | PPG uses LED light reflection to measure blood volume changes in the capillaries, indirectly determining heart rate and HRV. An LED-light is shown onto the skin and a sensor measures the amount of light that is reflected back. The more light is reflected back, the lower the blood volume. This technology is widely integrated into smartwatches and wristbands.<ref name=":0" /> | ||
| Line 184: | Line 118: | ||
- Affected by skin tone, environmental light, and sensor placement | - Affected by skin tone, environmental light, and sensor placement | ||
==== Galvanic Skin Response (GSR) - Skin Conductance Measurement ==== | ===== Galvanic Skin Response (GSR) - Skin Conductance Measurement ===== | ||
GSR measures skin conductivity, which increases as sweat glands activate under stress. This is a direct indicator of autonomic nervous system activity. GSR works through electrodes on the skin that measure the electrical conductivity of the skin.<ref name=":0" /> | GSR is also referred to as electrodermal activity (EDA). GSR measures skin conductivity, which increases as sweat glands activate under stress. This is a direct indicator of autonomic nervous system activity. GSR works through electrodes on the skin that measure the electrical conductivity of the skin.<ref name=":0" /> | ||
Advantages: | Advantages: | ||
| Line 199: | Line 133: | ||
- contact with the skin is needed and proper positioning for accurate results. | - contact with the skin is needed and proper positioning for accurate results. | ||
==== Skin Temperature (ST) ==== | ===== Skin Temperature (ST) ===== | ||
Stress can cause fluctuations in peripheral skin temperature due to changes in blood flow. Wrist-worn thermistors or infrared sensors can detect these changes.<ref name=":1">G. Taskasaplidis, D. A. Fotiadis and P. D. Bamidis, "Review of Stress Detection Methods Using Wearable Sensors," in IEEE Access, vol. 12, pp. 38219-38246, 2024, doi: 10.1109/ACCESS.2024.3373010. | Stress can cause fluctuations in peripheral skin temperature due to changes in blood flow. Wrist-worn thermistors or infrared sensors can detect these changes.<ref name=":1">G. Taskasaplidis, D. A. Fotiadis and P. D. Bamidis, "Review of Stress Detection Methods Using Wearable Sensors," in IEEE Access, vol. 12, pp. 38219-38246, 2024, doi: 10.1109/ACCESS.2024.3373010. | ||
| Line 212: | Line 146: | ||
- It is not always a direct stress indicator. Temperature can fluctuate due to other factors. It is more suitable as a secondary sensor that can complement more accurate sensors. | - It is not always a direct stress indicator. Temperature can fluctuate due to other factors. It is more suitable as a secondary sensor that can complement more accurate sensors. | ||
==== Blood Pressure (BP) and Blood Oxygen Saturation (SpO2) ==== | ===== Blood Pressure (BP) and Blood Oxygen Saturation (SpO2) ===== | ||
Blood pressure increases under stress, however it can also fluctuate due to other physiological factors. | Blood pressure increases under stress, however it can also fluctuate due to other physiological factors. | ||
| Line 223: | Line 157: | ||
- Blood Pressure is linked to cardiovascular health, making it useful beyond stress monitoring. | - Blood Pressure is linked to cardiovascular health, making it useful beyond stress monitoring. | ||
Disadvantages: | |||
- Wrist-based blood pressure measurements lack clinical accuracy | - Wrist-based blood pressure measurements lack clinical accuracy | ||
| Line 229: | Line 163: | ||
- Oxygen saturation fluctuations are not always directly linked to stress. | - Oxygen saturation fluctuations are not always directly linked to stress. | ||
==== Which indicators and sensors to use ==== | ===== Which indicators and sensors to use ===== | ||
Based on the strengths and weaknesses of each technology, the best combination of sensors to incorporate in a wristband would include either measures of heart rate variability (preferably PPG) or sensors of Galvanic skin response (GSR) as primary sensors. As an addition, skin temperature sensors or blood pressure sensors can be implemented as secondary sensors to enhance accuracy. | Based on the strengths and weaknesses of each technology, the best combination of sensors to incorporate in a wristband would include either measures of heart rate variability (HRV) (preferably PPG) or sensors of Galvanic skin response (GSR) as primary sensors. As an addition, skin temperature sensors or blood pressure sensors can be implemented as secondary sensors to enhance accuracy. | ||
== | === The Role of Music in Stress Reduction === | ||
Numerous studies have demonstrated that music can significantly lower stress and anxiety levels. For instance, Nilsson (2008)<ref name=":5">Nilsson U. The anxiety- and pain-reducing effects of music interventions: a systematic review. AORN J. 2008 Apr;87(4):780-807. doi: 10.1016/j.aorn.2007.09.013. PMID: 18395022. | |||
</ref> reviewed 42 randomized control studies and found that soothing music - typically characterized by a tempo of 60 to 80 beats per minute - was particularly effective. Interestingly, the majority of participants responded best to self-selected music, whether it was their favorite songs or choices made from a curated list of genres. | |||
</ref> | |||
Music has an influence on people's mood and stress in several ways. In this section an overview of the effect of music on different aspects of stress and mood will be presented. | Music has an influence on people's mood and stress in several ways. In this section an overview of the effect of music on different aspects of stress and mood will be presented. | ||
===== How Music Affects Brain waves ===== | |||
The relationship between music and brain activity is profound. Research indicates that music can alter brain waves, which reflect mental states. When individuals focus on rhythmic stimuli for an extended period, they can reach new levels of awareness. As they engage with the rhythm, their brain waves synchronize with it, promoting relaxation and reducing stress. | |||
The relationship between music and brain activity is profound. Research indicates that music can alter brain waves, which reflect mental states. When individuals focus on rhythmic stimuli for an extended period, they can reach new levels of awareness. As they engage with the rhythm ,their brain waves synchronize with it, promoting relaxation and reducing stress. | |||
===== Biochemical Effects of Music ===== | |||
Listening to music also impacts brain chemistry. Multiple brain imaging studies have shown that the brain's responses of listening to pleasant music involve the same regions involved in reward and pleasure<ref>Laukka, Petri. (2007). Uses of music and psychological well-being among the elderly. Journal of Happiness Studies. 8. 215-241. 10.1007/s10902-006-9024-3. | Listening to music also impacts brain chemistry. Multiple brain imaging studies have shown that the brain's responses of listening to pleasant music involve the same regions involved in reward and pleasure<ref>Laukka, Petri. (2007). Uses of music and psychological well-being among the elderly. Journal of Happiness Studies. 8. 215-241. 10.1007/s10902-006-9024-3. | ||
</ref>. The neurotransmitter dopamine, associated with the brain's reward system, is released when we enjoy pleasant music, contributing to feelings of happiness. Additionally, serotonin, which regulates mood, is increased by enjoyable music and decreased by unpleasant sounds. Slow music has been shown to lower levels of norepinephrine, a hormone that regulates arousal, further aiding in relaxation. | </ref>. The neurotransmitter dopamine, associated with the brain's reward system, is released when we enjoy pleasant music, contributing to feelings of happiness. Additionally, serotonin, which regulates mood, is increased by enjoyable music and decreased by unpleasant sounds. Slow music has been shown to lower levels of norepinephrine, a hormone that regulates arousal, further aiding in relaxation. | ||
| Line 274: | Line 181: | ||
Endorphins, known for inducing feelings of well-being, are also influenced by music. While techno music may lower endorphin levels, classical music tends to elevate them, showcasing the diverse effects different genres can have on our biochemical state. | Endorphins, known for inducing feelings of well-being, are also influenced by music. While techno music may lower endorphin levels, classical music tends to elevate them, showcasing the diverse effects different genres can have on our biochemical state. | ||
===== Music and Cortisol Levels ===== | |||
A major stress system in the human body is the hypothalamus-pituitary-adrenal (HPA) axis. The main effector of the HPA axis is cortisol, also commonly referred to as the 'stress' hormone. Cortisol levels increase in responses to stress and increased cortisol levels can reflect both psychological and behavioral stress<ref name=":9">Thoma MV, La Marca R, Brönnimann R, Finkel L, Ehlert U, Nater UM (2013) The Effect of Music on the Human Stress Response. PLoS ONE 8(8): e70156. <nowiki>https://doi.org/10.1371/journal.pone.0070156</nowiki> | A major stress system in the human body is the hypothalamus-pituitary-adrenal (HPA) axis. The main effector of the HPA axis is cortisol, also commonly referred to as the 'stress' hormone. Cortisol levels increase in responses to stress and increased cortisol levels can reflect both psychological and behavioral stress<ref name=":9">Thoma MV, La Marca R, Brönnimann R, Finkel L, Ehlert U, Nater UM (2013) The Effect of Music on the Human Stress Response. PLoS ONE 8(8): e70156. <nowiki>https://doi.org/10.1371/journal.pone.0070156</nowiki> | ||
</ref>. | </ref>. | ||
| Line 284: | Line 190: | ||
The impact of music extends to cortisol levels as well. Exposure to music has been shown to reduce elevated cortisol levels, effectively counteracting stress. Notably, major key compositions are more effective in reducing stress and cortisol than minor key pieces. Conversely, techno music can increase stress hormones, while classical music is linked to lower cortisol levels. | The impact of music extends to cortisol levels as well. Exposure to music has been shown to reduce elevated cortisol levels, effectively counteracting stress. Notably, major key compositions are more effective in reducing stress and cortisol than minor key pieces. Conversely, techno music can increase stress hormones, while classical music is linked to lower cortisol levels. | ||
===== Physiological Responses to Music ===== | |||
Musical stimuli, particularly rhythm and tempo, can influence physiological responses through a process known as entrainment. This principle suggests two objects vibrating at similar frequencies will resonate together. For stress reduction, music should ideally have a tempo at or below the resting heart rate (less than 80 beats per minute), predictable dynamics, fluid melodic movement, pleasing harmonies, and regular rhythms. Instruments like strings, flutes, and pianos are particularly effective in creating soothing soundscapes. | Musical stimuli, particularly rhythm and tempo, can influence physiological responses through a process known as entrainment. This principle suggests two objects vibrating at similar frequencies will resonate together. For stress reduction, music should ideally have a tempo at or below the resting heart rate (less than 80 beats per minute), predictable dynamics, fluid melodic movement, pleasing harmonies, and regular rhythms. Instruments like strings, flutes, and pianos are particularly effective in creating soothing soundscapes. | ||
Music with slow, steady and repetitive rhythms can exert hypnotic effects, contributing to relaxation. By occupying the brain's attention channels with meaningful and soothing auditory stimuli, music can effectively distract from stressors in the environment. | Music with slow, steady and repetitive rhythms can exert hypnotic effects, contributing to relaxation. By occupying the brain's attention channels with meaningful and soothing auditory stimuli, music can effectively distract from stressors in the environment. | ||
===== Individual Preferences and Cultural Influences ===== | |||
It is crucial to recognize that responses to music are not uniform; they vary based on individual factors such as familiarity, preference, current mood, and musical training. Research has shown that subjects from diverse cultures can identify emotions conveyed by music, suggesting a universal connection to musical expression. However, personal preference plays a significant role in the effectiveness of music as a stress-relief tool. | It is crucial to recognize that responses to music are not uniform; they vary based on individual factors such as familiarity, preference, current mood, and musical training. Research has shown that subjects from diverse cultures can identify emotions conveyed by music, suggesting a universal connection to musical expression. However, personal preference plays a significant role in the effectiveness of music as a stress-relief tool. | ||
Cultural traditions greatly influence affective responses to music. Therefore, it is recommended that healthcare professionals, such as nurses, consider cultural differences in music preferences when selecting therapeutic music. Studies indicate that participants often prefer no music over prescribed music, highlighting the importance of personal choice in achieving relaxation. The correlation between relaxation and enjoyment of music emphasizes that familiarity and pas experiences can override the inherent qualities of the music itself. | Cultural traditions greatly influence affective responses to music. Therefore, it is recommended that healthcare professionals, such as nurses, consider cultural differences in music preferences when selecting therapeutic music. Studies indicate that participants often prefer no music over prescribed music, highlighting the importance of personal choice in achieving relaxation. The correlation between relaxation and enjoyment of music emphasizes that familiarity and pas experiences can override the inherent qualities of the music itself. | ||
===== Conclusion ===== | |||
In summary, music serves as a powerful tool for stress reduction, influencing brain activity, biochemistry, and physiological responses. The type of music, its tempo, and personal preferences all play critical roles in its effectiveness. Understanding these factors can help individuals harness the therapeutic potential of music to alleviate stress and enhance well-being. | In summary, music serves as a powerful tool for stress reduction, influencing brain activity, biochemistry, and physiological responses. The type of music, its tempo, and personal preferences all play critical roles in its effectiveness. Understanding these factors can help individuals harness the therapeutic potential of music to alleviate stress and enhance well-being. | ||
== Effective types of music == | === Effective types of music === | ||
Not all types of music are equally effective in the reduction of stress. Multiple studies have shown that music that is familiar to the person with dementia has better effects than unknown music. Each person's history, identity and significant moments from their lives are intimately correlated with their musical taste<ref name=":2" />. Furthermore music that the person has come to know in their youth or as young adult has the best effect. This music often elicits strong memories and emotions, which can help in the reduction of stress and mood improvement. It has been shown that both live music and pre-recorded music work in reducing anxiety. | Not all types of music are equally effective in the reduction of stress. Multiple studies have shown that music that is familiar to the person with dementia has better effects than unknown music. Each person's history, identity and significant moments from their lives are intimately correlated with their musical taste<ref name=":2" />. Furthermore music that the person has come to know in their youth or as young adult has the best effect. This music often elicits strong memories and emotions, which can help in the reduction of stress and mood improvement. It has been shown that both live music and pre-recorded music work in reducing anxiety. | ||
| Line 310: | Line 213: | ||
For people with dementia living in elderly residents, another way in which music can be a relaxing factor, is in that relaxing music can buffer the noise coming from various sources and can decrease the resident's perception of these noxious noises. This in turn lessens the physiological and psychological responses to the noise, including agitated behavior. This, however, would only be effective under the condition that the music is a few decibels above the noise level of the noxious noises. This way some of the primary sources of agitation (e.g. personnel helping other residents) may be decreased and a sound source that is intentionally relaxing is introduced. | For people with dementia living in elderly residents, another way in which music can be a relaxing factor, is in that relaxing music can buffer the noise coming from various sources and can decrease the resident's perception of these noxious noises. This in turn lessens the physiological and psychological responses to the noise, including agitated behavior. This, however, would only be effective under the condition that the music is a few decibels above the noise level of the noxious noises. This way some of the primary sources of agitation (e.g. personnel helping other residents) may be decreased and a sound source that is intentionally relaxing is introduced. | ||
===== Key Characteristics of Relaxing Music ===== | |||
# '''Instrumentation''': Relaxing music tends to be acoustic and instrumental, allowing the listener to immerse themselves in the sound without the distraction of lyrics<ref name=":7">Wei-Chun Wang; A study of the type and characteristics of relaxing music for college students. ''Proc. Mtgs. Acoust.'' 5 May 2014; 21 (1): 035001. <nowiki>https://doi.org/10.1121/1.4902001</nowiki></ref>. | # '''Instrumentation''': Relaxing music tends to be acoustic and instrumental, allowing the listener to immerse themselves in the sound without the distraction of lyrics<ref name=":7">Wei-Chun Wang; A study of the type and characteristics of relaxing music for college students. ''Proc. Mtgs. Acoust.'' 5 May 2014; 21 (1): 035001. <nowiki>https://doi.org/10.1121/1.4902001</nowiki></ref>. | ||
# '''Rhythm and Tempo''': The rhythm and pace of music are crucial, with relaxing selections often featuring slow tempos, around 60 beats per minute. This tempo aligns with the natural rhythm of the human heart when at rest<ref name=":7" />. Furthermore, the music should comprise mostly strings with minimal percussion and bass<ref name=":5" />. | # '''Rhythm and Tempo''': The rhythm and pace of music are crucial, with relaxing selections often featuring slow tempos, around 60 beats per minute. This tempo aligns with the natural rhythm of the human heart when at rest<ref name=":7" />. Furthermore, the music should comprise mostly strings with minimal percussion and bass<ref name=":5" />. | ||
| Line 317: | Line 219: | ||
# '''Familiarity''': Familiarity with the music plays a significant role in perceived relaxation. Listeners often prefer music that resonates with their experiences, leading to positive sensory experiences and beneficial chemical changes in the body<ref name=":7" />. | # '''Familiarity''': Familiarity with the music plays a significant role in perceived relaxation. Listeners often prefer music that resonates with their experiences, leading to positive sensory experiences and beneficial chemical changes in the body<ref name=":7" />. | ||
# '''Volume level''': It has been found that loudness is a characteristic of non-relaxing music<ref name=":6" />. Suggested is that music used for relaxation should have a maximum volume level of 60 dB<ref name=":5" /> | # '''Volume level''': It has been found that loudness is a characteristic of non-relaxing music<ref name=":6" />. Suggested is that music used for relaxation should have a maximum volume level of 60 dB<ref name=":5" /> | ||
# '''Timing of onset''': Research has shown that music can best be played at moments in which a patient experiences acute distress, especially when patients show signs of agitation. However, one should be careful that the sudden playing of music is not an additional stressor for the patient. | |||
== | === Interviews === | ||
To get more information and opinions from people that work with people with Dementia, we have decided to conduct interviews. We contacted care homes and caregivers to ask if or how they incorporate music in their care and if they do, how it impacts their patients. We also asked them for their opinion our product proposal so we can get feedback from the people that would be the actual users of the product if it was to be made. | |||
We also contacted the research group Dementia & Technology from the TU/e itself. This way we could ask actual experts on the topic about their opinions on our proposal. | |||
Since caregivers are people with very busy schedules we decided to not only ask them if we can have a conversation but also send them a list of questions that they can answer if they do not have the time to have an actual conversation with us. This way we could still get their opinion, even if they could not meet with us. | |||
For the research group we asked them if they were available to have an in person meeting with us, since we thought they would have more time and be more open to talk with students. We prepared different questions for the people from the research group since we wanted to ask them more about researching people with Dementia and how they deal with the complications that come with it, and if they had any feedback on our product proposal. | |||
In this section we will provide the analysis and most important findings of the surveys and the conducted interview. For a more detailed description of the asked questions and responses, we would like to refer to the appendix. | |||
===== Analysis of caregivers responses to the conducted survey ===== | |||
There were 6 replies to the email we send out. Some were shorter than others, and others answered all questions asked. One person explained that music is almost always a part of dementia patients lives. Music can be personalized and ‘normal’ technologies are used, like headphones, stereo’s, pick-up’s, tv’s, live music and, sometimes also music therapy. | |||
In the surveys we asked for the caregivers personal experience with dementia patients. One of the questions we asked was what are the ways you notice a patient is agitated? Responses were in line with our literature research. Most often body language examples are given like clenching of muscles (in body or face), panic look in their eyes, pushing doors, plucking things, looking around the room, and all caregivers gave the example of restlessness and walking behaviour (‘loopgedrag’). Verbal examples were also given like talking a lot, or talking very little, curt replies, not accepting help or getting emotional. | |||
We also asked if there are certain moments in a day when a patient is most agitated. The caregivers all agreed that it there are many reasons why a patient can get agitated. Multiple caregivers, explained that some reasons a patient can get agitated if something upsetting happened just before or if a feeling of safety is disturbed. Changes are difficult for patients with dementia which can also result in agitated behaviour. A bad night sleep can warrant agitated behaviour or moments of care because these are moments a lot is asked of a patient. Activities can have many stimuli and someone can get overstimulated. After a family visit patients can also tend to get upset. One specific caregiver noted that sometimes dementia patients get agitated around 16.00 in the afternoon. For our design it would be good to help aid with music during these moments to prevent agitation. | |||
Our device should help reduce agitation in dementia patients but to design this in the best way we were interested in what other interventions were most used in these cases. Depending on the personality of a patient some interventions given were to let the resident feel their emotion and leave them alone. Caregivers also try to find out what caused the agitation and if possible remove this causation so the patient feels in control again. Going outside or going to their own room also helps, caregivers try to find a quiet environment to help calm the patient. The last example, and most interesting to us is to play the residents favourite CD’s. This shows the relevance of our device for both patient and caregiver in these situations. | |||
Diverse music is played throughout the day because different patients prefer different music. Most people feel emotions from the music based on their past and/or memories. Even people further along in the dementia process recognise music. Depending on patients music can also trigger sad memories which in turn can make a patient sad or agitated. Music is mainly used as a distraction and the music stimuli should have a positive effect. When someone has too little stimuli music is a useful tool. A caregiver also explained that nature sounds combined with slow music or meditation music, like singing bowls, or handpan can also have a positive effect. This was also corroborated by Karlijn van Rijen. | |||
Sometimes music does not work because if someone is overstimulated music can only add more stimuli which is the problem in the first place. Sometimes the stimuli or negative thoughts are just too strong. Wrong music or too loud of music (/sounds) can be a trigger and instead of having a calming effect music will have a agitative effect. Sometimes a patient (that is further along in the dementia process) cannot say no to the music and this also causes frustration. | |||
Based on the surveys it would be hard for the prototype to be used in group settings. The loudness of the device is a concern, but the caregivers would find it ideal if it could also work in group settings. Based on the information gathered above this would be difficult to make work because every person responds different to different kinds of music. Unless of course in the very unlikely circumstance, all patients in this group setting have the same preference. | |||
Four out of five caregiver saw potential to use this device in practice, whether that was for all patients or for only one. The last caregiver thought it would be better to use this for people who still live at home and thought it would be interesting to have a sensor that measures when a person has ‘bewegingsdrang’ (urge to move/ walking behaviour) and then starts playing music. | |||
The caregivers gave us great feedback and gave us some suggestions to include in the design. The urged us to design the device in such a way that it takes a resident’s life history. The device should have a friendly appearance that should not be too big and can be put down. It should be able to withstand falling and being thrown. The volume should be easily adjusted and the device should be easy to clean | |||
===== Analysis of interview with Karlijn van Rijen from the TUe Dementia & Technology research group ===== | |||
Humesock is a sock that measures stress and visualizes this. Through early warnings, timely reactions are possible before escalation. It might be a possibility for us to try and find what kind of algorithms this device uses for our own product. | |||
It is important to consider whether something is a pacifier technology. We have to be cautious of possible ethical risks. For example, our device should is not to be used as a quick fix, since that would be inhumane. | |||
Furthermore, Karlijn van Rijen indicated that it would also be good to research other audio than just music. For example ambient sounds are also promising in the reduction of stress. | |||
An important thing to consider about the wearable itself is the physical form our device would have. Wearables can be quickly stigmatizing and feel uncomfortable. It might therefore be an idea to do research about what types of wearables we could use (e.g. socks or rings that monitor stress). Furthermore, people with dementia often take of these kinds of wearables, so good research about wristbands used by people with dementia is important. | |||
It is also important to consider how we make sure people want to buy our device. It is good to know the current need for our product and it would be nice to chart this. It is important to consider who our target users are and what they are willing to spend on a device that achieves what we intend our product will be achieving. | |||
== Design Proposal == | |||
[[File:Design Proposal.jpg|thumb|355x355px|Design Proposal]] | |||
Our product, named Zola, is designed to start playing music if the measured HRV and EDA (which is the same as GSR, as noted before) levels of the patient have trespassed a certain level. We will call this stress threshold the ‘stress-level’. The HRV and EDA will be measured by a stress monitor device worn by the patient. The patient should have the Zola app downloaded on their smartphone which will receive and analyze the data measured by the stress monitor. | |||
If stress is detected by the monitor, and thus the stress-level has been reached, the app will start playing music through an external speaker. This speaker can be any device that can be connected to the smartphone via Bluetooth (e.g. portable speakers or hearing devices with Bluetooth). The volume will start from 0% and increase gradually until the preferred volume that the user/caregiver has set in the app is reached. The music will stop playing once the measured data is below the stress-level or if the user/caregiver has clicked the on/off button in the app. If the user’s stress-level has not decreased, caregivers that have connected their Zola account to the patient’s Zola account, will get a notification. | |||
Because our design is using an external speaker, it will be more affordable for users that already own a good speaker. This also makes our design more sustainable, since there is no need for producing a new speaker for our design. | |||
== Actors == | |||
==== Stress monitor device ==== | |||
[[File:Image app.png|thumb]]After researching and comparing different types of stress monitor options, it appears that the best stress monitor for our design is Health eTile's We-Be band. | |||
The We-Be band by Health eTile is a wristband used for precise and continuous monitoring of measurements such as HRV, EDA, temperature and an estimation of blood pressure. We-Be uses Bluetooth Low Energy protocol and offers excellent connection and low-latency data transmission. Furthermore, this wristband has a battery life of up to two weeks. Moreover, the We-Be band has a user-friendly design which is important since our users would have to wear the band throughout the entire day. With the We-Be band, it is possible to use the Health eTile’s iOS/Android APIs to retrieve the raw data from the wristband and develop our own app. | |||
=== | ==== Patient ==== | ||
The patient is required to wear the stress monitor device throughout the day. If the patient is still able to do so, despite their dementia. They can indicate their preferred choice of music and maximum volume settings during the initial setup of the application and device. | |||
==== Caregiver ==== | |||
Caregivers play a crucial role in ensuring that the We-Be band and the patient's smartphone remain adequately charged. Given that the We-Be band has a battery life of up to two weeks, maintaining its charge should add to much to their workload. Additionally, caregivers are responsible for setting up the app and the device by configuring the preferred settings in the patient's account. In instances where the patient is unable to put on or remove the wristband as needed, caregivers must also assist with this task. Finally, caregivers are required to create their own Zola accounts. This step is essential for enabling them to receive notifications regarding the patient's stress levels, thereby making it possible to intervene when necessary. | |||
=== | ==== Smartphone app ==== | ||
[[File:Image Zola app.png|thumb|525x525px|Preview of the Zola app]] | |||
The app on the smartphone of the user collects and analyses the data received from the stress monitor device. If the HRV and the EDA data is above a certain stress level threshold, the app will start playing music from volume 0% up to the maximum set volume through Bluetooth via an external speaker. Furthermore, the user can set the maximum playing time. Once the music has been playing longer than the max. playing time, a notification will be send to the caregiver's account. The app also has the option to let the user add their own preferred music. Furthermore the user or caregiver can set up a timeframe referred to as "Quiet time", during which no music will be played if the measured data shows signs of stress. This can be helpful for users that do not want to be disturbed by music while they are sleeping. | |||
In the figure from left to right is showcased: | |||
The sign-up screen, the screen where caregivers can be connected to the patients, the settings that the patients can set on their account, and the notification chat that the caregivers will receive when a patient is stressed longer than the set maximum amount of time. | |||
==== Bluetooth speaker ==== | |||
The speaker will play the audio that is set in the app by the user starting at volume 0% and increasing to the set maximum volume. In our design, any speaker that can be connected to the user's smartphone through Bluetooth can be used. Think of a portable speaker but also for example hearing aids with Bluetooth can be connected. | |||
== Design requirements == | |||
* The app should automatically connect to the external speaker via Bluetooth when the patient is within it's range. | |||
* | * The data measured by the stress monitoring device should be used only for this device purposes and should be saved securely without scolding the user’s privacy. | ||
* The user or caregiver should be able to easily stop the audio through a ‘stop’ button in the app. | |||
* | * If there is no speaker currently available, the app should continue playing music through the smartphone instead. | ||
* The app should have a clear User Interface | |||
== Scenario == | |||
==== | ==== Phase 1: Start measurements ==== | ||
* | * The user or caregiver downloads the app and makes sure the wristband is charged. | ||
* The monitoring device starts measuring the HRV and the EDA of the patient. | |||
* The measurements are sent in real-time to the smartphone app | |||
==== | ==== Phase 2: Monitoring & analyzing measurements ==== | ||
* | * The app analyzes the received raw data and compares it to the stress level threshold. | ||
* If the received data does not exceed the threshold, nothing happens. | |||
=== | ==== Phase 3: Stress detected ==== | ||
* If the received data is above the threshold, the app will connect to the external speaker through Bluetooth. | |||
* The speaker will play the audio that is given by the user in the app. The volume will increase from 0% to the maximum volume that is set by the user in the app. | |||
==== Phase 4: Stop measurements ==== | |||
* The music will stop playing if: | |||
** The ‘stop’ button in the app is pressed. | |||
** The measured stress levels decrease and are under the threshold stress levels | |||
== | == Analysis of Data == | ||
When the We-Be band is connected to a gateway, which could be either a mobile phone or a PC, the data is automatically analyzed and users can visualize the data in real-time. The We-Be band monitors a wide range of bodily functions. Some of these are particularly relevant for assessing stress, including EDA (electrodermal activity), HRV (Heart rate variability) and temperature. The monitoring of these physiological signals and machine learning are integrated by implementing state-of-the art algorithms. This ensures real-time stress evaluation can be provided. | |||
In order to measure HRV, the We-Be band uses photoplethysmography (PPG). The band is equipped with four channels of PPG signals which offer accurate and stable measurement. Multiple automatic PPG annotation modules are integrated in the We-Be platform to clean the raw PPG signals and provide clean signals which can be analyzed<ref name=":10">''Science behind – Healthetile''. (z.d.). <nowiki>https://healthetile.io/science-behind/</nowiki></ref>. | |||
To illustrate in a bit more detail how the We-Be band accomplishes the analysis raw signals, the analysis of EDA signals is detailed in the section below. | |||
=== EDA analysis === | |||
Electrodermal activity (EDA) is one of the most sensitive indicators of emotional responses, arising from the spontaneous activation of sweat glands in the skin. It is intricately linked to mood, arousal, and attention. Due to its high stability, ease of measurement, and great sensitivity, EDA has become the most effective physiological parameter for reflecting changes in sympathetic nerve activity<ref name=":10" />. | |||
EDA signals are composed of two main components: a tonic component (skin conductance level - SCL), which is a slowly varying signal that establishes the baseline level of EDA, and a phasic component (skin conductance response - SCR), which is a rapidly fluctuating signal directly associated with the activity of the sweat glands, which respond to stimuli such as stress or emotional changes<ref>Bartolomé-Tomás, A., Sánchez-Reolid, R., Fernández-Sotos, A., Latorre, J. M., & Fernández-Caballero, A. (2020). Arousal Detection in Elderly People from Electrodermal Activity Using Musical Stimuli. ''Sensors'', ''20''(17), 4788. <nowiki>https://doi.org/10.3390/s20174788</nowiki></ref>. | |||
https:// | The We-Be band incorporates pyEDA, which is an open-source toolkit that can be used to process EDA signals using statistical analysis and automatic feature extraction. It is noteworthy that EDA in pyEDA should not be confused with EDA - GSR (Galvanic Skin Response). In this context, EDA refers to Electronic Design Automation, a field focused on optimizing productivity in the design and manufacturing of electronic components<ref>''Overview — Python EDA Documentation''. (z.d.). <nowiki>https://pyeda.readthedocs.io/en/latest/overview.html</nowiki></ref>. | ||
'''Processing EDA Signals using pyEDA''' | |||
The | The EDA signals collected by the We-Be band come in a raw format and contain motion artifacts. To effectively use the EDA signal to predict stress, several crucial processing steps need to be undertaken to remove noise and extract a clean signal. An article by Aqajari explains how the pyEDA toolkit does this<ref>Aqajari, S. (2021). pyEDA: An Open-Source and Versatile Feature Extraction Python Toolkit for Electrodermal Activity. ''UC Irvine''. ProQuest ID: Aqajari_uci_0030M_17382. Merritt ID: ark:/13030/m57q5w81. Retrieved from <nowiki>https://escholarship.org/uc/item/3xq0084m</nowiki></ref>. | ||
[[File:Figure 2..png|thumb|557x557px|Processing Pipeline Architecture for pyEDA<ref>Aqajari, S. (2021). pyEDA: An Open-Source and Versatile Feature Extraction Python Toolkit for Electrodermal Activity. ''UC Irvine''. ProQuest ID: Aqajari_uci_0030M_17382. Merritt ID: ark:/13030/m57q5w81. Retrieved from <nowiki>https://escholarship.org/uc/item/3xq0084m</nowiki></ref>]] | |||
The pyEDA toolkit processes EDA signals through a structured pipeline that includes a pre-processing and feature extraction stage. | |||
The | In the pre-processing stage, the raw EDA data undergoes several steps to enhance its quality. The first step is down-sampling. EDA data is typically sampled at a higher frequency than necessary. By reducing the sampling rate, the memory usage and processing can be decreased, while retaining essential information. The next step is moving averaging. This technique smooths the data, helping to eliminate artifacts caused by physical movements and gestures, ensuring that the signal reflects true physiological responses. | ||
Once the data is pre-processed, the meaningful features critical for stress detection are extracted in the feature extraction stage. Features can either be extracted by statistical feature extraction or automatic feature extraction. A key component of statistical feature extraction is the cvxEDA algorithm, which separates the EDA signal into its tonic and phasic components. This is needed because then rapid changes in the EDA signal which correlate with stress responses can be accurately identified. | |||
After the EDA signals have been processed and features extracted, machine learning algorithms are used to build predictive models. These analyze the extracted features to identify patterns associated with stress. | |||
== Testing Possibility == | |||
===== Technical tests ===== | |||
Multiple technical tests should be performed to test the functionality of the prototype. These technical tests should: | |||
* test whether the data is send to the smartphone continuously. | |||
* test whether the app retrieves the real-time data. | |||
* test the Bluetooth connection between the app and the speaker. | |||
* test whether the app connects to the speaker when the data reaches the stress level. | |||
* test whether the on/off button and the volume button work in the app. | |||
This | ===== User test ===== | ||
Once all technical tests have been performed, user tests can be conducted. This test will evaluate what the effect of our prototype is on the stress levels of the patients with dementia. The user test contains a control group and a test group. | |||
'''Test group:''' | |||
The participants will be wearing the We-Be band. If the measured data reaches the stress threshold, a connection will be made between the app and the speaker allowing the speaker to start playing music. | |||
'''Control group:''' | |||
The participants will be wearing the We-Be band. If the patients reach the stress level, no music will start playing. | |||
After conducting this experiment, data will be analyzed to find whether the stress level of the patients in the test group will decrease faster than the stress level in the control group. Furthermore, interviews or questionaries would be conducted with the caregivers and/or family of the patients. From this data, we will be able to have an insight of the effect of our prototype on the patients and the caregivers workload from the caregivers’ point of view. | |||
== Limitations and future additions == | |||
==== Stress measurement ==== | |||
This technology greatly depends on the accuracy of the stress measurement. If the stress is not measured accurately, the device could turn on at undesirable moments. The effectiveness of the music intervention depends on different factors. Firstly, the sensor placement of the wearable is important, especially when measuring HRV and EDA. To get accurate measurements the wearable should have proper skin contact. If the wearer moves around a lot, that can have a negative effect. Additionally, the EDA data can be influenced by external factors such as humidity. | |||
==== Music choice ==== | |||
Based on the research we conducted, it was found that reactions to music are not uniform. This implies that a song can make one user very calm, whereas it can have the complete opposite effect on someone else. Because of this, the family and caregivers should be able to curate their own playlist. This can however be difficult if no one know what music a patient used to listen too, or what music used to calm others down. For future additions, we could implement AI to create music. It can start out with music that is generally found to be "calming" and adjust the music based on the physiological reactions of the user. | |||
Furthermore, music | Furthermore, it has been found that other auditory cues rather than just music can exert the desired relaxing effects. For example sounds as the flowing of rivers or the falling of raindrops can also work for stress relieve. In further research and development in this device the playing of these sounds rather than music when stress is detected could be a valuable extension<ref name=":9" />. | ||
==== Different stages of dementia ==== | |||
The way that the product can be implemented also greatly depends on the stage of dementia that we focus on. In our case, we decided to focus on medium to late stage dementia. This makes it hard for the patient to remember what music they like, so they will most likely not be able to express their preferences themselves. Based on our research<ref name=":11" /> we found that late stage dementia patients might have diminished response to music. Even if the effect is small, it always seems to be neutral to positive. | |||
==== Wearable ==== | |||
Research indicates that individuals with dementia often struggle to accept new devices, such as wearables. A study focusing on nursing home residents and their formal and informal caregivers explored perceptions of wearable technologies. The findings revealed that for a wearable device to be accepted by residents, it must meet a specific set of criteria<ref name=":8">Peeters, M. W. H., Schouten, G., & Wouters, E. J. M. (2021). Wearables for residents of nursing homes with dementia and challenging behaviour: Values, attitudes, and needs. ''Gerontechnology'', ''20''(2), 1-13. <nowiki>https://doi.org/10.4017/gt.2021.20.2.7.06</nowiki> | |||
</ref>. | |||
On key consideration is the size of the wearable; it should be compact and unobtrusive to avoid drawing excessive attention, which could lead to resistance from users. Additionally, the design is crucial. If the wearable resembles a watch, but does not look like a traditional watch, it may not be perceived as suitable for individuals with dementia. Caregivers noted that familiarity in design can significantly impact acceptance, as recognizable forms tend to foster comfort and ease of use<ref name=":8" />. | |||
Another important consideration is the placement of the on and off button. If this button is easily accessible to the individual wearing the device, there is a risk that the wearable could be accidentally turned off. People often have a natural tendency to fiddle with objects around them, and a button located on a wristband becomes an inviting target for such behavior. This highlights the need for careful design to prevent unintended disruptions in the device's functionality<ref name=":8" />. | |||
Overall, these insights highlight the importance of thoughtful design and user-centric features in developing wearable technologies for dementia patients. The WeBe band, which is used in this project, does not adhere to all these specifications. The WeBe band is quite big and it contains buttons which are easy to be reached by the person wearing it. Further research could explore other wristbands or other types of wearables to measure stress that might be more suitable for individuals with dementia. | |||
https:// | ==== Pavlov effect ==== | ||
During research and brainstorming about ideas for this device, the question arose whether a Pavlov effect could occur, creating an association between once loved music and stress. In other words, whether the music could become a stressor in itself due to the association between music and stress. The Pavlov effect is a consequence of classical conditioning, which can be described as the learning mechanism through which certain stimuli become associated with relevant events. These can be either appetitive or aversive. When a Pavlov effect occurs, a person has thus learned that a certain cue predicts a pleasant or unpleasant event<ref>Hermann, C., Sperl, M.F.J. (2023). Classical Conditioning. In: Matson, J.L. (eds) Handbook of Clinical Child Psychology. Autism and Child Psychopathology Series. Springer, Cham. <nowiki>https://doi.org/10.1007/978-3-031-24926-6_21</nowiki></ref>. | |||
During the project, concerns arose whether the music played when stress is detected, could be interpreted as such a cue predicting an the occurrence of a certain event - in our project, stress. In that case, the music that is supposed to be relaxing could have the opposite effect of being a sign the user is stressed, possibly making the individual even more stressed. | |||
Of course these are only speculations and further research would be necessary to fully understand if this is indeed a legitimate concern. | |||
==== Survey ==== | |||
In order to gather opinions about our device from individuals who have direct contact with dementia patients, we distributed surveys to several care homes and caregivers. We also sent surveys to the research group Dementia & Technology from the TU/e itself. For a more detailed overview of the questions asked in these surveys, please refer to the section "Interviews", which can be found further down this Wiki page. | |||
While we received some valuable responses, the number of participants in our surveys was limited. With more time allocated to this project, we could have conducted more extensive interviews to gain additional insights from those closely interacting with patients. | |||
Furthermore, we were unable to engage directly with individuals living with dementia. this would have been a significant addition to our research, and in future studies, it would be an excellent opportunity to investigate the actual effects and functioning of our device among dementia patients. | |||
From the interviews we gathered information that we were able to implement into the design, such as the familiarity of a watch as wearable. This is also sturdy like advised in the interviews/ survey. The biggest limitation of our device is the fact that music can help with agitation but it can also have a negative effect if a patient is already feeling overstimulated. This depends on the situation and cannot always be gauged before. | |||
==== Prototype ==== | |||
Perhaps the most significant limitation of this project is that no physical prototype has been constructed, which hindered the ability to test the device effectively. Our group's academic backgrounds resulted in a lack of expertise in protype development, preventing us from creating a functional and testable model. Consequently, our assumptions about the workings of the device, for example what type of music should be played and the timing of it, are solely based on literature research and insights gathered from our interviews. | |||
In future research, developing and testing a physical prototype would be invaluable for refining the device and enhancing its effectiveness. This hands-on approach could provide critical feedback and insights that are essential for the successful development of our device. | |||
[[File:NASA technology readiness levels.png|thumb|213x213px|[https://en.wikipedia.org/wiki/Technology_readiness_level NASA Technology Readiness levels]]] | |||
==== Technology Readiness Level<ref>Wikipedia contributors. (2024, 21 oktober). ''Technology readiness level''. Wikipedia. <nowiki>https://en.wikipedia.org/wiki/Technology_readiness_level</nowiki> </ref> ==== | |||
In the interview with Karlijn van Rijen, she advised us to look at the TRLs (Technology readiness levels) of our idea. TRLs are a method for estimating the maturity of technologies during the acquisition phase. The TRL is determined during a technology readiness assessment (TRA). It has 9 levels and they are described in the following categories: | |||
* Basic Technology Research | |||
* Research to Prove Feasibility | |||
* Technology Development | |||
* Technology Demonstration | |||
* System/ Subsystem Development | |||
* System Test, Launch & Operations | |||
Looking at the TRLs and our device, we made the following assessment. The first level is passed as we have observed and reported the basic principles. The second level is also examined as we have formulated a technological concept and its application. The third level requires experimental proof of concept which we have started by designing what functions we want our device to have and how to apply these functions in practice. We started by looking at the sensors and wearable we want to use. The next steps are not yet taken, our technology is not validated in a lab (level 4) nor in relevant environment (level 5). The technology is also not demonstrated in relevant environment (level 6) nor has a system prototype demonstration in operational environment taken place (level 7). Lastly the system is not complete and qualified (level 8) and it the actual system has not been proven in operational environment (level 9). Ideally these are steps taken in the future developmental phases of the device. | |||
==State of the art== | |||
We performed a literature study on the current state of the art on several relevant topics. | |||
- | ===== Technology in dementia care ===== | ||
We found this <ref>Astell, A. J., Bouranis, N., Hoey, J., Lindauer, A., Mihailidis, A., Nugent, C., & Robillard, J. M. (2019). Technology and Dementia: The Future is Now. ''Dementia and Geriatric Cognitive Disorders'', ''47''(3), 131–139. <nowiki>https://doi.org/10.1159/000497800</nowiki></ref> article on using technology in care for dementia patients. This article summarizes several key areas of technological development in dementia care. The main domains in which there is a lot of technological advancement include: 1) diagnosis assessment and monitoring, 2) maintenance of functioning, 3) leisure and activity, and 4) caregiving and management. Examples of technological advances in the domain of leisure and activity also include systems that use music to soothe patients. In the paper a one-button radio is mentioned, but also a simple interface for making music and systems for collaborative music making. The article ends with the conclusion that, despite numerous technological initiatives in dementia care, adoption rates remain low. Contributing factors include a lack of awareness, challenges in accessibility and insufficient support. The paper emphasizes the need for policies, funding, and practices that go beyond a purely medical approach, advocating for a holistic perspective that includes prevention strategies and ways to support a meaningful life with dementia. | |||
===== Effects of music with Dementia patients ===== | |||
A lot of studies have been done to research the effects of music on dementia patients. We found several analyses and studies related to the topic. | |||
- | We found a meta-analysis that looks at four different factors in music therapy for dementia patients <ref>Pedersen, S. K. A., Andersen, P. N., Lugo, R. G., Andreassen, M., & Sütterlin, S. (2017). Effects of Music on Agitation in Dementia: A Meta-Analysis. ''Frontiers in Psychology'', ''8''. <nowiki>https://doi.org/10.3389/fpsyg.2017.00742</nowiki></ref>. Pedersen et al. performed a meta-analysis to (1) investigate whether music therapy has a positive effect on reducing agitation for patients with dementia. Furthermore, they (2) compare personalized and group music intervention. Besides that, Pedersen (3) evaluates the effect of preferences in music by comparing music based on patient preference without prior consultation with patients or caregivers. Lastly, the study (4) focusses on comparing the benefits of active versus passive music intervention. In active music intervention, participants actively engage by singing, dancing, or playing an instrument. In passive music intervention, participants listen to live or recorded music without actively engaging. The results of this meta-analysis indicate that (1) music intervention does significantly decrease agitation in patients with dementia. Furthermore, the analysis (2) shows that personalized music therapy may have a larger effect in certain cases, however the effect is less consistent across the different studies used in this research. Both individual and prescribed music preferences (3) show a medium effect size. Finally, both active and passive music interventions have similar effects. Passive interventions may work better in different settings. The study performed by Pedersen et al. indicated that music intervention has a reducing effect on agitation of patients with dementia. | ||
- | We also found a study on the impact of music on the self in dementia patients <ref>Baird, Amee & Thompson, William. (2018). The Impact of Music on the Self in Dementia. Journal of Alzheimer’s Disease. 61. 827-841. 10.3233/JAD-170737. </ref>. This study proposes a theoretical framework which enhances the sense self in patients with dementia. To explain this framework, numerous features of music have been mentioned: Engaging, Persuasive, Social, Synchronization, Physical, Emotional, and Personal. This framework explains how music engages the five aspects of one’s self, namely ecological, interpersonal, private, extended, and conceptual self. The ecological self is the self has it is perceived through sensory information and the environment. Numerous features of music, such as physical, synchronous, engaging, and emotional, are important for this self. The interpersonal self can be explained as the self that socially interacts with others. Here the persuasive and engaging aspects of music play a key role. The extended self shows how the self was in the past and how it might be in the future. The different way of engaging with music, and the personal and emotional features of music contributed to engaging the extended self for people with dementia. The private self exists of experiences that others do not have access to, such as thoughts, beliefs, and experiences. Music can help this self as a new way to express themselves. Finally, the conceptual self is indicated the concept that the individual has of themselves, for example self-identity, roles, and social identity. The researchers of this paper identify the music features and the aspects of the self using two case studies and conclude that music has a unique ability to engage with multiple aspects of the self. | ||
This research paper <ref>Spiro, N. (2010). Music and dementia: Observing effects and searching for underlying theories. ''Aging & Mental Health'', ''14''(8), 891–899. <nowiki>https://doi.org/10.1080/13607863.2010.519328</nowiki></ref> studies whether the effect of music on dementia is beneficial and if so, why that is the case. The article focusses on three key areas, namely “music and memory”, “music and depression”, and “Agitation and aggressive behaviors”. The article states that some people with dementia remember music longer than they remember and respond to other types of information. Reminiscence music therapy, music therapy that uses familiar songs to trigger memories of the individual with dementia, has reduced working on symptoms of depression. This could be explained by the fact that music induced physical and emotional changes. Furthermore, music could help reduce stress, sooth pain and energize the body. Therefore, music could be used as an aid for mood regulations. Moreover, music has a beneficial influence on reducing agitated and aggressive behaviors of individuals with dementia during various activities and various times. Playing music that is preferred by the participant has the biggest outcome. Music makes sounds more familiar and predictable. This could lead to creating a positive emotional state as people retrieve positive memories. | |||
In this study <ref>Gibson, Grant. (2007). Music and the wellbeing of people with dementia. Ageing and Society. 27. 127 - 145. <nowiki>https://doi.org/10.1017/S0144686X06005228</nowiki>. </ref>, Sixsmith and Gibson perform qualitative research on the influence that music has on the everyday life of participants with dementia. In-depth interviews were conducted with a sample size consisting of 26 patients with dementia living in either their own homes or in residential care. This paper highlights the benefits of music but also the problems that could arise while listening or actively participating in musical activities. The data from the interviews shows that the beneficial effect of having music in the lives of people with dementia could enhance the feelings of wellbeing. Music could make people with dementia ready to express their happiness both physically and emotionally. Furthermore, music supports valued activities. Playing music in the background while working on a task could make the task more enjoyable for people with dementia. Moreover, music encourages social interaction. During musical activities, most of the participants were accompanied by their family, carers or by other people with dementia. Music therefore is a way for people with dementia to communicate with other sand have meaningful social interactions. Lastly, music gives people with dementia a higher degree of empowerment and control over their own lives. Sixsmith and Gibson state multiple challenges that arise when people with dementia engage with music, such as difficulties expressing their preferences, hearing difficulties, the loss of confidence, and social barriers in care homes. | |||
This research paper <ref>McDermott, O., Orrell, M., & Ridder, H. M. (2014). The importance of music for people with dementia: the perspectives of people with dementia, family carers, staff and music therapists. ''Aging & Mental Health'', ''18''(6), 706–716. <nowiki>https://doi.org/10.1080/13607863.2013.875124</nowiki></ref> focused on the meaning and value of musical intervention for not only people with dementia, but also their families, care home staff and music therapists. McDermott et al. are aiming to explore the meaning and value of music from the people with dementia point of view. The paper also analyses how families, care home staff and music therapists view the effects of music. Furthermore, the paper aims to find a link between psychosocial factors and the results of the study to be able to develop a theoretical musical framework of music in dementia. The qualitative data was ‘gotten’ from conducting focus groups and interviews with care home residents with dementia and their families, care home staff, music therapies, and day hospital clients with dementia. From the data received, it can be concluded that meaningful musical experience could result in people with dementia feeling emotionally connected with other people. Moreover, musical activities lead to social interaction between residents and staff in care homes. That has resulted in a more positive impact on the environment of the care home. The researchers also state that music is linked to personal identity and life history of people with dementia. | |||
''' | This paper <ref name=":4">Soufineyestani, M., Khan, A., & Sufineyestani, M. (2021). Impacts of Music Intervention on Dementia: A Review using Meta-Narrative Method and Agenda for Future Research. ''Neurology International'', ''13''(1), 1–17. <nowiki>https://doi.org/10.3390/neurolint13010001</nowiki></ref> shows a meta analysis of the effect of music on dementia patients. Several positive effects of music on patients with dementia have been established in different fields, namely biologically (hr, etc.), behaviorally (less stress, agression, etc.), cognitively (better speech e.g.) and emotionally (more enjoyment in life). It is however, mainly focused on guided music intervention, where the patient is encouraged to sing along, etc. | ||
To gain more insight into the results of trials done with music therapy on patients we found this systematic review <ref>Lam, H. L., Li, W. T. V., Laher, I., & Wong, R. Y. (2020). Effects of Music Therapy on Patients with Dementia—A Systematic Review. ''Geriatrics'', ''5''(4), 62. <nowiki>https://doi.org/10.3390/geriatrics5040062</nowiki></ref> . The review was conducted on clinical trials reported from 1 January 1946 to 1 May 2020. The results showed that 13 studies reported overall cognition as an outcome. With 4 showing significant improvements, 6 showing no improvements and 1 with a mixed effect. The studies also showed that effects of music therapy on the memory of patients living with dementia were mixed, with 4 out of 5 studies reporting significant improvements. Music therapy also showed significant improvements for language or verbal fluency. Two studies explored the effects of singing on BPSD and it showed significant reductions in BPSD in patients with dementia. The results were mixed for listening to music and using musical instruments. Most studies also showed a significant reduction in either anxiety or depression or both. Five studies showed that music listening significantly improved mood, while 2 studies did not show this. There were mixed results for the studies of the effect of music therapy on agitation. Six out of eight studies reported significantly reduced agitation when music listening was the primary intervention, but mixed results were observed for the effects of combined music therapy. In one crossover trial in which Baroque music was played an adverse effect was observed and there was a significant increase in the number of episodes of agitated behaviour when music was played. Levels of were reduced in two of the rials and daily functioning reported no significant improvements. Mixed results were reported on the effects of music therapy on the quality of life. | |||
- | Similarly, we found this review <ref>Thompson, N., Odell-Miller, H., Underwood, B. R., Wolverson, E., & Hsu, M. (2024). How and why music therapy reduces distress and improves well-being in advanced dementia care: a realist review. ''Nature Mental Health''. <nowiki>https://doi.org/10.1038/s44220-024-00342-x</nowiki></ref> on how and why music therapy reduces distress and improves well-being in advanced dementia care. The review is mainly focused on music therapy with a music therapist present. According to the review, the music therapy has positive effects on patients. | ||
This study <ref>Ragneskog, H., & Kihlgren, M. (1997). Music and Other Strategies to Improve the Care of Agitated Patients with Dementia. ''Scandinavian Journal of Caring Sciences'', ''11''(3), 176–182. <nowiki>https://doi.org/10.1111/j.1471-6712.1997.tb00451.x</nowiki></ref> from 1997 shows that interest in the topic of using music for care of agitated dementia patients has been there for a long time.[[File:Table 1 as shown in the article.png|thumb|512x512px]] | |||
https:// | |||
[[File:Table 1 as shown in the article.png|thumb|512x512px]] | |||
Agitation is defined as a clinical term for inappropriate verbal or motor activity that is not an obvious expression of need or confusion. Repetitions of words, restlessness and aggression are examples of symptoms that can be included in the concept of agitation. The nursing directors of five nursing homes selected 13 staff from six different wards and the directors of four collective residential units selected four staffs. Interviews were conducted with all responders, they lasted about 45 minutes and the following questions were asked: | Agitation is defined as a clinical term for inappropriate verbal or motor activity that is not an obvious expression of need or confusion. Repetitions of words, restlessness and aggression are examples of symptoms that can be included in the concept of agitation. The nursing directors of five nursing homes selected 13 staff from six different wards and the directors of four collective residential units selected four staffs. Interviews were conducted with all responders, they lasted about 45 minutes and the following questions were asked: | ||
| Line 620: | Line 475: | ||
· What are your opinions and experiences regarding pharmacological treatment of these patients and which psychopharmacological drugs would you suggest for an elderly patient showing irritability and aggression? | · What are your opinions and experiences regarding pharmacological treatment of these patients and which psychopharmacological drugs would you suggest for an elderly patient showing irritability and aggression? | ||
And they were also asked to summarize what they regarded as the most important aspect of caring, and to draw up strategies for caring of this group of patients. The | And they were also asked to summarize what they regarded as the most important aspect of caring, and to draw up strategies for caring of this group of patients. The themes shown in the table were found as strategies to manage agitation in patients with dementia: | ||
We found this analysis <ref name=":11">Ragneskog, H., Asplund, K., Kihlgren, M., & Norberg, A. (2001). Individualized music played for agitated patients with dementia: Analysis of video‐recorded sessions. ''International Journal of Nursing Practice'', ''7''(3), 146–155. <nowiki>https://doi.org/10.1046/j.1440-172x.2001.00254.x</nowiki></ref> on video-recorded sessions where individualized music was played for agitated dementia patients. Agitation is one of the symptoms patients with dementia suffer from. This study investigated whether individualized music could be used as a nursing intervention to reduce such symptoms. The study was done on four patients. There were video recordings during four sessions in four periods. There was a control period without music and then two periods where individualized music was played, and lastly one period where classical music was played. The documented sessions were analysed and the author noted in a protocol if the patient was calm or agitated. To be considered agitated, the patient would be showing signs of being upset, such as beating the table: shrieking/shouting, trying to stand up, irritability, and/or restlessness. Samples of segments were then analysed by KA by means of Facial Action Coding System technique. This technique is used to identify distinct facial muscle movements. The music seemed to affect all patients, but the two who were most affected by dementia reacted the least to the music. Some days a patient was clearly in a bad mood and then the music did not affect them. When asked the patients told the researchers that they liked the music. The study found a decrease in agitation after individualized music was played. The effect of classical music was not as evident. | |||
https:// | This article <ref>Vuijk, J. G. J., Brinke, J. K., & Sharma, N. (2023). Utilising Emotion Monitoring for Developing Music Interventions for People with Dementia: A State-of-the-Art Review. ''Sensors'', ''23''(13), 5834. <nowiki>https://doi.org/10.3390/s23135834</nowiki></ref> presents a comprehensive analysis of current methodologies that employ emotion monitoring to create music-based interventions for dementia patients. The article examines various technologies and approaches used to assess emotional responses in dementia patients, aiming to enhance the effectiveness of music therapy interventions. By synthesizing existing research, the review highlights the potential benefits and challenges associated with integrating emotion monitoring into therapeutic practices for dementia care. The study underscores the importance of personalized interventions and suggests directions for future research to optimize outcomes for individuals affected by dementia. | ||
===== Stress measurement technology ===== | |||
Since our product is designed to detect stress in dementia patients through a wearable, we also did research on that topic. We found this article <ref>Yanan Ding, Kaiwen Tan, Li Sheng, Huiwen Ren, Zhen Su, Hongying Yang, Xin Zhang, Jianyang Li, PingAn Hu (2024). Integrated mental stress smartwatch based on sweat cortisol and HRV sensors. Biosensors and Bioelectronics, Volume 265, 2024, 116691, ISSN 0956-5663. <nowiki>https://doi.org/10.1016/j.bios.2024.116691</nowiki></ref> on using a smartwatch to detect stress through sweat cortisol levels and a person's heart rate variability (HRV). According to the article, the technique works quite well to measure stress. This research was not done on dementia patients specifically, but it does show potential in detecting stress in people with a wearable device that measures biological functions. [[File:Table 1 as shown in the article (2).png|thumb|370x370px]]Similarly, we found this article <ref>Siirtola, P. (2019). ''Continuous stress detection using the sensors of commercial smartwatch''. <nowiki>https://doi.org/10.1145/3341162.3344831</nowiki></ref> on using the sensors in a commercial smartwatch for stress detection. Stress detection using wrist-worn sensors has recently been studied widely and it has been shown that it can detect stress quite reliably. An example is given where stress was measured accurately at a level of 83% at laboratory conditions. It was measured using skin temperature, electrodermal activity, heart rate, blood volume pulse and accelerometer signals. Most studies use, among other bio-sensors, electrodermal activity (EDA or galvanic skin response). The article concentrates on studying how well stress can be detected using the sensors included to commercial smartwatches. The study concludes that the best recognition rate was obtained using a combination of skin temperature, BVP, and heart rate signals ((LDA: 87.4%, QDA: 84.9%, RF: 82.4%). It concludes that EDA signals are not necessary to use in the recognition process. The article also investigates the effect of window size to the recognition rates and finds that long windows, result in better recognition rates rather than short ones. In their case the best window was 120 seconds. | |||
''' | In this study <ref>Chalmers, T., Hickey, B. A., Newton, P., Lin, C., Sibbritt, D., McLachlan, C. S., Clifton-Bligh, R., Morley, J., & Lal, S. (2021). Stress Watch: The use of heart rate and heart rate variability to detect stress: A pilot study using smart watch wearables. ''Sensors'', ''22''(1), 151. <nowiki>https://doi.org/10.3390/s22010151</nowiki></ref> a fitbit was used to record heart rate data alone. ECG was used to generate HRV parameters. A statistical analysis was done on the results of the participants (medical students). Participants completed the DASS and the general population has significantly higher scores on all of the DASS subscales than the medical students. But it was found that both resting and stress phase HR were significantly higher in the medical student population than the general population. The study is relevant for us because it shows that HRV could be used to predict the quality of response to acute stress. This may aid in developing a physiological algorithm for stress that could be incorporated into wearable technologies. According to the article there were no devices on the market at the time (2021) that have a rigorously validated algorithm for stress detection. | ||
https:// | This paper <ref>''A review on mental stress detection using wearable sensors and machine learning techniques''. (2021). IEEE Journals & Magazine | IEEE Xplore. <nowiki>https://ieeexplore.ieee.org/abstract/document/9445082</nowiki></ref> provides a review of several methods for detecting mental stress in different environments using wearable sensors and machine learning techniques. Stress is defined as a psycho-physiological response to challenges that can lead to severe health issues. Wearable sensors collect biological signals that reflect the body's response to stressors. Advantages of wearable sensors include real-time monitoring and non-intrusiveness. In the article, various physiological signals which have potential to be a measure of stress are considered. Each signal provides unique insights into how the body responds to stress. Some wearables integrate multiple of these sensors to measure stress more effectively. The article also discusses some challenges and limitations of wearable sensor-based stress detection. | ||
The | This article <ref>Alshamrani, M. (2021). An Advanced Stress Detection Approach based on Processing Data from Wearable Wrist Devices. ''International Journal of Advanced Computer Science and Applications'', ''12''(7). <nowiki>https://doi.org/10.14569/ijacsa.2021.0120745</nowiki></ref> presents a novel method for real-time stress detection using data from smartwatches. The study utilizes an open-source dataset that includes motion and physiological signals, such as heart rate and accelerometer data, collected from wrist-worn devices. After preprocessing the raw data to remove noise and enhance quality, the study applies two deep learning models: a Fully Convolutional Network (FCN) and a Residual Network (ResNet). The results indicate that the FCN model performs better than ResNet and traditional machine learning approaches, achieving high accuracy in distinguishing stress from non-stress conditions. The findings highlight the potential of smartwatches combined with advanced deep learning techniques as effective tools for continuous and unobtrusive stress monitoring. The study concludes that such systems could significantly improve stress management and well-being, particularly in real-world applications. | ||
''' | ===== Wearables for dementia patients ===== | ||
Using wearable technology devices with dementia patients can be difficult. We found this article <ref>Peeters, M. W. H., Schouten, G., & Wouters, E. J. (2021). Wearables for residents of nursing homes with dementia and challenging behaviour: Values, attitudes, and needs. ''Gerontechnology'', ''20''(2), 1–13. <nowiki>https://doi.org/10.4017/gt.2021.20.2.7.06</nowiki></ref> that discusses the values, attitudes and needs for using wearables for residents of nursing homes. The paper specifically focuses on using wearables with dementia patients and what their needs are. According to the paper, devices that are mounted on the wrist cannot be too tight, as to not hurt the patients. They should be recognizable for dementia patiens, something like a watch. The patient should not be able to turn the device off themselves by a button on the outside, as there were some patients in the research that turned off the device. The device should be water resistant and should not be too bulky. Finally, it would be good for the device to be customizable to fit different patients' needs. All of these requirements are taken into account with our design. The most important thing is the perceived usefullness and comfortability for the patients. | |||
https:// | We found another study <ref>Adam, E., Meiland, F., Frielink, N., Meinders, E., Smits, R., Embregts, P., & Smaling, H. (2024). User Requirements and Perceptions of a sensor system for early stress detection in people with dementia and people with intellectual disability: Qualitative study. ''JMIR Formative Research'', ''8'', e52248. <nowiki>https://doi.org/10.2196/52248</nowiki></ref> on what is needed for a stress sensor for dementia patients. The study concludes that a wearable could be integrated into clothing or wristbands for familiarity purposes, it should also be comfortable and it could be customizable to increase user acceptance. To increase acceptance and decrease negative perception the device should be as discreet as possible. The device should also be easy to put on and take off, again to increase patient comfort. According to the study, it is most important that the wearable is washable and safe. The study also provides several perceived positives for stress sensors for dementia patients. Namely, that stress can be identified and early intervention methods can be used to quickly alleviate it. Similarly, the study also provides several perceived negatics that should be taken into account. It is possible that the sensor is not accepted by the user and it could replace the human aspect of care. Both of these possibilities should be taken into account when using stress sensors with dementia patients. | ||
This article <ref>Olmedo-Aguirre, J. O., Reyes-Campos, J., Alor-Hernández, G., Machorro-Cano, I., Rodríguez-Mazahua, L., & Sánchez-Cervantes, J. L. (2022). Remote healthcare for elderly people using wearables: a review. ''Biosensors'', ''12''(2), 73. <nowiki>https://doi.org/10.3390/bios12020073</nowiki></ref> discusses the use of wearable sensors for the remote monitoring of elderly individuals. There is a specific focus on how wearables can contribute to healthcare. Several physiological variables that can be measured are discussed, among which heart rate (variability), blood pressure and oxygen saturation. The article makes a distinction between commercial wearables such as smart watches and research prototypes such as smart textiles. It is stated that the commercial wearables are increasing in their reliability of sensors. Several benefits and challenges of wearables in elderly care are discussed. Some of the challenges include the limited battery life of wearables and user acceptance. It is however concluded that wearables provide a promising solution for elderly healthcare by enabling continuous monitoring and early disease detection. | |||
https:// | This systematic review <ref>Husebo, B. S., Heintz, H. L., Berge, L. I., Owoyemi, P., Rahman, A. T., & Vahia, I. V. (2020). Sensing technology to monitor behavioral and psychological symptoms and to assess treatment response in people with dementia. A systematic review. ''Frontiers in Pharmacology'', ''10''. <nowiki>https://doi.org/10.3389/fphar.2019.01699</nowiki></ref> examines how sensor-based technologies can be used to track behavioral and psychological symptoms of dementia (BPSD) and assess treatment responses. Analyzing 34 studies, the review highlights the use of wearable sensors such as accelerometers and gyroscopes to monitor physical activity, sleep disturbances, and agitation. It also discusses non-wearable motion sensors and smart home technologies that track movement patterns and behavioral changes in real-world settings. The findings suggest that these technologies are generally effective in detecting agitation, restlessness, and wandering, and they have been well-received as non-intrusive monitoring tools. Some studies also explored the potential of motion data for early detection of mild cognitive impairment. However, the review identifies key challenges, including concerns about data privacy, ethical considerations, and the need for greater user involvement in system design to ensure practical implementation. Overall, the review concludes that sensor-based monitoring holds great promise for improving dementia care, but further research is needed to validate these technologies, address ethical concerns, and develop frameworks for their safe and effective integration into healthcare settings. | ||
===== Stress in dementia patients ===== | |||
We also found an article on stress in dementia patients in general. In this paper <ref>Sharp, B. K. (2017). Stress as Experienced by People with Dementia: An Interpretative Phenomenological Analysis. ''Dementia'', ''18''(4), 1427–1445. <nowiki>https://doi.org/10.1177/1471301217713877</nowiki></ref>, a study is described on the subject of stress as experienced by people with dementia. The study contributes to the supporting of people with dementia, by creating a greater understanding about how people with dementia make meaning from their experience of stress. The questions of interest where how people with dementia perceive their experiences of stress and how they cope with these. It was found that individual personality traits and established coping styles persist and sustain influence in managing stress. This is contrary to previous assumptions that dementia is paired with an inevitable decline and progressive vulnerability to stress. It was furthermore demonstrated that people with Alzheimer's disease demonstrate a preference for "emotion focused" over "problem solving" approaches. | |||
To see if the stress aleviation aspect of our idea is feasible, we found this article <ref>Sung, H., Chang, A. M., & Lee, W. (2010). A preferred music listening intervention to reduce anxiety in older adults with dementia in nursing homes. ''Journal of Clinical Nursing'', ''19''(7–8), 1056–1064. <nowiki>https://doi.org/10.1111/j.1365-2702.2009.03016.x</nowiki></ref> that describes the usage of preffered music to reduce anxiety for dementia patients. The article investigates the effectiveness of personalized music sessions in alleviating anxiety among elderly nursing home residents with dementia. Utilizing a quasi-experimental pretest and posttest design, the study involved 52 participants divided into two groups: | |||
* Experimental Group: 29 individuals received 30-minute sessions of music tailored to their personal preferences, delivered by trained nursing staff twice a week for six weeks. | |||
* Control Group: 23 individuals continued with standard care without any music intervention. | |||
Anxiety levels were assessed using the Rating Anxiety in Dementia scale at both the beginning and end of the study. The results demonstrated that the experimental group experienced a significant reduction in anxiety compared to the control group. The authors conclude that implementing preferred music listening is a cost-effective and viable strategy for reducing anxiety in older adults with dementia, emphasizing the importance of individualized care approaches in nursing home settings. | |||
https:// | This pilot study <ref>Nesbitt, C., Gupta, A., Jain, S., Maly, K., & Okhravi, H. R. (2018). ''Reliability of Wearable Sensors to Detect Agitation in Patients with Dementia'' (pp. 73–77). <nowiki>https://doi.org/10.1145/3232059.3232067</nowiki></ref> explores the feasibility of using wearable technology to monitor and detect agitation in individuals with dementia. The research involved eight participants residing in an assisted living facility, each equipped with off-the-shelf smartwatches and smartphones capable of tracking location, limb movements, vocalizations, and heart rate. Data collected over four-hour observation periods were compared against observations using the Cohen-Mansfield Agitation Inventory (CMAI). The findings indicated that increases in limb movements and heart rate, as detected by the wearable sensors, correlated with observed agitation episodes. However, vocalization data were less reliable due to background noise in the communal environment. The study concludes that wearable sensors hold promise for detecting agitation in dementia patients, suggesting that personalized profiles could enhance detection accuracy. Further research is recommended to refine these technologies for broader application. This study uses | ||
Finally, this paper <ref>Kikhia, B., Stavropoulos, T., Andreadis, S., Karvonen, N., Kompatsiaris, I., Sävenstedt, S., Pijl, M., & Melander, C. (2016). Utilizing a Wristband Sensor to Measure the Stress Level for People with Dementia. ''Sensors'', ''16''(12), 1989. <nowiki>https://doi.org/10.3390/s16121989</nowiki></ref> describes a study in which the effectiveness of measuring the stress levels in people with dementia using a single wristband sensor is explored. Stress is a common issue for individuals with dementia, and it is traditionally assessed through questionnaires completed by a caregiver. This is a time-consuming and subjective process. In this research, a wearable sensor that tracks galvanic skin response (GSR) and movement is assessed in its effectiveness of detecting stress episodes. During the study, the sensor continuously recorded physiological data, which was processed using an online platform to classify the stress levels on a scale from 0 to 5. The goal was to find out if the identified stress episodes by the sensor correlated with those observed by the caregiver. The results showed that there was a strong correlation between the data from the sensor and the caregiver observations. There were, however, strong variations in stress levels among individuals, which highlights the need for personalized stress thresholds. This can improve accuracy in detection. The conclusion of the researchers is that a wristband sensor is a promising tool for monitoring stress. It provides objective, real-time data, which can help caregivers in for example recognizing stress patterns and intervening more effectively. | |||
==References== | |||
<references /> | |||
== Appendix == | |||
== | |||
=== Interviews === | |||
==== Questions for caregivers ==== | ==== Questions for caregivers ==== | ||
| Line 762: | Line 553: | ||
* familyoffice@domusvaluas.nl | * familyoffice@domusvaluas.nl | ||
* servicedesk@zorginoktober.nl | * servicedesk@zorginoktober.nl | ||
* woonzorg@bloezem.nl | * woonzorg@bloezem.nl | ||
* info@elkedageenfijnedag.nl | * info@elkedageenfijnedag.nl | ||
* contact@pietervanforeest.nl | * contact@pietervanforeest.nl | ||
| Line 772: | Line 563: | ||
* adviesteam@pleyade.nl | * adviesteam@pleyade.nl | ||
* info@hetlaar.nl | * info@hetlaar.nl | ||
===== Responses summarized ===== | |||
· Waar aan merkt u bij een patiënt dat die rusteloos/ geïrriteerd is? | |||
{| class="wikitable" | |||
|'''Reply 1''' | |||
|'''Reply 2''' | |||
|'''Reply 3''' | |||
|'''Reply 4''' | |||
|'''Reply 5''' | |||
|- | |||
|Boos kijken | |||
|Houding | |||
|Lichaamshouding | |||
|Kort-af reageren | |||
|Stilletjes worden | |||
|- | |||
|Rusteloos dwalen | |||
|Lichaamstaal | |||
|Spanning in de spieren/ gezicht | |||
|Verdriet | |||
|Geïrriteerd | |||
|- | |||
|Aan deuren trekken | |||
|Emotioneel | |||
|Onrust in de ogen (paniekblik) | |||
|Afsluiten voor je | |||
|Boos | |||
|- | |||
|Weglopen | |||
|Boosheid | |||
|Loopgedrag | |||
|Geen hulp aanvaarden | |||
|Blijven lopen | |||
|- | |||
|Korte antwoorden geven | |||
|Teruggetrokken | |||
|Wiebelen | |||
|Boos gedrag | |||
|Geen rust vinden | |||
|- | |||
|Op zich heen kijken | |||
|Loopgedrag | |||
|Veel praten | |||
|lopen | |||
| | |||
|- | |||
|Plukken | |||
| | |||
|Elke client vertoont zijn eigen tekenen van onrust | |||
|Geen rust in het lichaam hebben | |||
| | |||
|} | |||
· Op wat voor momenten merkt dat een patiënt rusteloos/ geïrriteerd is? | |||
{| class="wikitable" | |||
|'''Reply 1''' | |||
|'''Reply 2''' | |||
|'''Reply 3''' | |||
|'''Reply 4''' | |||
|'''Reply 5''' | |||
|- | |||
|Als de nabije veiligheid weg is | |||
|Kunnen heel divers zijn | |||
|Als er iets voorgevallen is | |||
|Als er net familie/ visite is geweest en deze weer weg gaan. | |||
|Verschillende momenten op de dag | |||
|- | |||
| | |||
|Tijdens zorgmomenten want dan wordt er van alles gevraagd van een cliënt en dit zorgt voor onrust en irritatie | |||
|Als iets anders dan ander is. | |||
|Rond 16u in de middag | |||
| | |||
|- | |||
| | |||
|Bij de dagbesteding als iemand nieuw is en/of eigenlijk niet wil komen kan er onrust zijn. | |||
|Een slechte nacht | |||
|Na een activiteit beneden in de gasterij (ontmoetingsruimte/ restaurant) die te veel prikkels hebben gegeven. | |||
| | |||
|- | |||
| | |||
|Of als er vooraf iets voorgevallen is, dit kan iets kleins zijn maar ook groot, dit kan aan de persoon zelf liggen in welke fase van dementie dit is of psychische aandoening. | |||
|Een cliënt wil gewoon niet op de dagopvang zijn maar thuis. | |||
| | |||
| | |||
|} | |||
· Wat zijn uw interventies normaal gesproken wanneer een patiënt gefrustreerd of rusteloos is? | |||
{| class="wikitable" | |||
|'''Reply 1''' | |||
|'''Reply 2''' | |||
|'''Reply 3''' | |||
|'''Reply 4''' | |||
|'''Reply 5''' | |||
|- | |||
|Emotie laten uiten | |||
|Achterhalen waar het aan ligt door 1 op 1 gesprek of in de rapportage terug te lezen wat het kan zijn | |||
|Afhankelijk van persoonlijkheid van patiënt | |||
|Inschatten wat de patiënt nodig heeft soms: praatje, soms knuffel. Soms poosje laten, rust op kamer | |||
|Laat de bewoner even | |||
|- | |||
|Naar buiten gaan | |||
|Extra ruimte geven, door apart te zitten of naar eigen kamer brengen | |||
|Nabijheid bieden | |||
|Onrustmedicatie geven | |||
|Veel 1 op 1 contact in rustige omgeving | |||
|- | |||
|Als je de trigger van boosheid weet, deze weghalen | |||
|Zorgen voor afleiding | |||
|Uit de situatie halen of ‘meebewegen’ zodat de client het gevoel krijgt weer de regie in handen te hebben | |||
| | |||
|Favoriete CD voor bewoner aanzetten. | |||
|} | |||
· Wordt er al wel eens muziek afgespeeld bij patiënten (ook als ze rustig zijn)? Zo ja, | |||
{| class="wikitable" | |||
|'''Reply 1''' | |||
|'''Reply 2''' | |||
|'''Reply 3''' | |||
|'''Reply 4''' | |||
|'''Reply 5''' | |||
|- | |||
|Ja, heel zachtjes op de achtergrond | |||
|Divers muziekaanbod | |||
|De meeste mensen krijgen emotie van muziek blij, verdrietig en gaan vaak terug naar het verleden/herinneringen | |||
Als de mensen nog "taal" tot hun beschikking hebben vertellen ze vaak verhalen over vroeger naar aanleiding van muziek. Of lichaamstaal aflezen welke emotie bepaalde muziek bij mensen teweeg brengt | |||
|Bij sommige cliënten helpt dit zeker. Het meeste effect zien wij dan als we de client een koptelefoon op kunnen geven, zodat alle andere geluiden uit de omgeving weg zijn. Toch heb ik het nog niet meegemaakt dat het DE oplossing is. Niet voor een langere periode op een dag. | |||
|Muziek zorgt voor ontspanning en genieten van bewoners | |||
|- | |||
|Afwisseling van muziek want niet iedereen houdt van hetzelfde | |||
|Heeft positief effect, maar kan ook emotioneel effect hebben | |||
|Mensen die al verder in het dementie proces zijn herkennen muziek die ze vroeger luisterden. Ook reageren deze mensen goed op natuurgeluiden gecombineerd met rustige muziek. Meditatie-muziek, klankschalen, handpan etc | |||
|Muziek is verschillend per mens | |||
|Verwisselt per bewoner | |||
|- | |||
|Ook bij onrust muziek opzetten, en dit is niet altijd rustige muziek maar vooral herkenbare muziek want door herkenning worden ze rustig | |||
|Klassiek, jaren 50/60, Nederlandstalig, rustgevende muziek of op aanvraag van de cliënt. | |||
|Ja bij rustige muziek kunnen mensen ook verdrietig worden of onrustig. Je weet nooit welke herinneringen muziek teweeg brengt, er bestaat geen recept voor een bepaalde reactie, muziek en emotie is zeer persoonsgebonden | |||
|Muziek gaat vooral om afleiding. De prikkel moet een positief effect hebben. | |||
|Als het de bewoner niet aanstaat dan kan hier ook weer irritatie uit voortkomen. | |||
|- | |||
| | |||
|Jazeker, er komen stofjes (oxytocine) vrij in de hersenen en deze zorgen voor een positief effect (geluk stofje). De muziek zorgt voor het stukje samenhorigheid/verbinding, betere motoriek. | |||
Maar kan ook een emotionele kant hebben, bijvoorbeeld als iemand in het verleden iets vervelens meegemaakt heeft en dit wordt dan ook weer teruggehaald, door een bepaald liedje. | |||
| | |||
| | |||
| | |||
|} | |||
o Wat voor effect heeft het? | |||
o Wat voor muziek zou dat dan zijn? | |||
o Heeft verschillende muziek dan ook een ander effect? | |||
· Zou muziek afspelen werken terwijl een patiënt al gefrustreerd is om ze te kalmeren? Of is het beter om al eerder muziek af te spelen wanneer patiënten nog kalm zijn? | |||
{| class="wikitable" | |||
|'''Reply 1''' | |||
|'''Reply 2''' | |||
|'''Reply 3''' | |||
|'''Reply 4''' | |||
|'''Reply 5''' | |||
|- | |||
|Muziek kan helpen maar kan dan ook te vel prikkels geven | |||
|Muziek helpt tegen rusteloosheid want het zorgt voor afleiding | |||
| | |||
|Soms wel maar niet altijd want soms zijn de prikkels/ negatieve gedachtes te sterk | |||
|Het mooiste zou zijn als je het voor bent, dat je al muziek afspeelt als de bewoner nog kalm is. | |||
|- | |||
|Als iemand onderprikkeld is dan helpt muziek juist | |||
|Hoeft niet echt daarvoor want rust is ook fijn | |||
| | |||
| | |||
| | |||
|} | |||
· Zou muziek afspelen op momenten dat een patiënt rusteloos/ geïrriteerd is ook een averechts effect kunnen hebben? Zo, ja op welke manier? | |||
{| class="wikitable" | |||
|'''Reply 1''' | |||
|'''Reply 2''' | |||
|'''Reply 3''' | |||
|'''Reply 4''' | |||
|'''Reply 5''' | |||
|- | |||
|Ja en het is echt aftasten. Wat nu werk werkt morgen misschien niet | |||
|Ja als het te hard staat of verkeerde muziekkeuze, of al overprikkeld, dan werkt het niet meer | |||
|Kan te veel zijn, vooral harde geluiden zijn meestal een trigger | |||
| | |||
|Muziek kan emotie versterken, te veel prikkels, niet bij machte zijn om nee te zeggen waardoor frustratie | |||
|} | |||
· Zou dit prototype ook werken in een groepssetting? | |||
{| class="wikitable" | |||
|'''Reply 1''' | |||
|'''Reply 2''' | |||
|'''Reply 3''' | |||
|'''Reply 4''' | |||
|'''Reply 5''' | |||
|- | |||
|Moeilijk te zeggen vanwege groepsdynamiek maar beter 1 op 1 | |||
|Yes | |||
| | |||
|Groepsverband is moeilijk maar als iemand alleen woont en je een sensor zou hebben waarop te zien is dat iemand veel bewegingsdrang heeft dat dan de muziek automatisch aangaat. | |||
|Kan als het niet te luid is maar andere bewoners kunnen er wel van schrikken. | |||
|} | |||
· Zou u een mogelijkheid zien om van ons boven benoemde prototype ook gebruik van maken in de praktijk? | |||
{| class="wikitable" | |||
|'''Reply 1''' | |||
|'''Reply 2''' | |||
|'''Reply 3''' | |||
|'''Reply 4''' | |||
|'''Reply 5''' | |||
|- | |||
|Zeker lijkt fijn | |||
|Ja is het proberen waard | |||
|Ideaal zou zijn een prototype wat zelf onrust kan detecteren, waar muziek uitkomt waar mensen geen herinnering aan hebben maar wel kalmerend werkt. Bv solfeggio frequenties, mantra's , natuurgeluiden. maar ook liedjes die mensen kennen. | |||
|Nee meer mogelijkheden waar mensen nog zelfstandig wonen. | |||
|1 bewoner die wisselende stemming heeft, wellicht zou muziek iets voor haar zijn. | |||
|} | |||
· Zijn er bij z’n soort prototype dingen waar we rekening mee moeten houden waar we nu nog niet aan hebben gedacht? | |||
{| class="wikitable" | |||
|'''Reply 1''' | |||
|'''Reply 2''' | |||
|'''Reply 3''' | |||
|'''Reply 4''' | |||
|'''Reply 5''' | |||
|- | |||
|Goed rekening houden met de levensgeschiedenis van de bewoner | |||
|Vriendelijke uitstraling | |||
|Makkelijk en klein neer te zetten | |||
| | |||
|Volume moet makkelijk te gelen zijn zonder dat we aan bewoner moeten zitten | |||
|- | |||
| | |||
| | |||
|Tegen vallen/ gooien bestand zijn. | |||
| | |||
|Makkelijk schoon te maken | |||
|} | |||
==== Questions for research group ==== | ==== Questions for research group ==== | ||
| Line 780: | Line 826: | ||
* What are things we should take into account in the implementation of our prototype? | * What are things we should take into account in the implementation of our prototype? | ||
==== Mail for research group ==== | ===== Mail for research group ===== | ||
<blockquote>Dear {name}, | <blockquote>Dear {name}, | ||
| Line 828: | Line 874: | ||
Slim om als je echt met mensen in de zorg onderzoek wil doen, zoals dementie patiënten dat je zorgt dat je wat terug doet voor zorgtehuizen, dan willen ze sneller mee werken. Dus maak er een leuke dag van bijv. | Slim om als je echt met mensen in de zorg onderzoek wil doen, zoals dementie patiënten dat je zorgt dat je wat terug doet voor zorgtehuizen, dan willen ze sneller mee werken. Dus maak er een leuke dag van bijv. | ||
Goed om te weten wat ons product als belang is in de realiteit, moeten we goed in beeld brengen. TRL zijn technological | Goed om te weten wat ons product als belang is in de realiteit, moeten we goed in beeld brengen. TRL zijn technological readiness levels over hoe ver je bent met je product en wat voor stappen je hiervoor moet ondernemen. Misschien wel slim om dat uit te werken om te kunnen laten zien. Stappen zijn bijv ook zo snel mogelijk funders aantrekken en nwo subsidies, hierna investeerders. Zorg ook dat we goed in beeld hebben wie onze eingebruikers zijn. Kinderen betalen vaak voor zulk soort producten of verzekeraars. Voor wie is het, markt of zorg. Maak dit van te voren duidelijk. Denk aan dat sommige dingen te duur zijn zoals robots die rond het huis lopen maar die wel daarvoor eigenlijk bedoeld zijn. | ||
Hoe zie je dit business model voor je? Aan welke kanalen ga je het verkopen? Is allemaal goed om duidelijk te hebben in je design process. | Hoe zie je dit business model voor je? Aan welke kanalen ga je het verkopen? Is allemaal goed om duidelijk te hebben in je design process. | ||
== | === Approach === | ||
< | Start by ature study. We want to make/ build a prototype and then interview healthcare workers on their opinions on our idea.doing a liter | ||
{| class="wikitable" | |||
|+ | |||
!Week 1 | |||
!Week 2 | |||
!Week 3 | |||
!Week 4 | |||
!Week 5 | |||
!Week 6 | |||
!Week 7 | |||
!Week 8 | |||
|- | |||
|13/02 Mail with topic and group | |||
|Start looking for interviewees | |||
|Set up interview schedule | |||
|Research all components necessary for a working product | |||
|Make a plan on how to integrate the components of our product into a working device. | |||
|Interpret results from the | |||
|Design an Inteface of app | |||
|Complete Wiki page | |||
|- | |||
|Set up project | |||
|Research possibilities for prototype design | |||
|Gather parts necessary for prototype | |||
|Conduct interviews and send surveys | |||
|Conduct interviews and send surveys | |||
|Research how data is being analyzed by chosen monitoring device | |||
|Prepare presentation | |||
| | |||
|- | |||
|Search and summarize 25 research papers | |||
|Literature Research about types of stress measurement | |||
|Literature Research about dementia, stress and music | |||
|Literature research about what types of music to use | |||
| | |||
|Design visualization of the workings of our device. | |||
|Presentation | |||
| | |||
|- | |||
|Work on Problem statement, Objectives, Users, approach, Milestones, Deliverables, | |||
and Planning | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|} | |||
<nowiki>*</nowiki>rough estimate in planning | |||
=== Milestones === | |||
What are the big checkpoints, so how long will we be working on each section e.g. | |||
====== Week 1: ====== | |||
* Finish Problem statement, Objectives, Users, approach, Milestones, Deliverables, and Planning sections | |||
* Finish State of the art section | |||
====== Week 2: ====== | |||
* Finish making sketches | |||
* Finalise the prototype design | |||
====== Week 4: ====== | |||
* Finalise Informed consent form | |||
* Finalise interview schedule | |||
====== Week 5: ====== | |||
* Finalise the idea of our product and receive feedback | |||
====== Week 6: ====== | |||
* Receive all data from the interviews | |||
====== Week 7: ====== | |||
* Give final presentation | |||
=== Deliverables === | |||
What we will be handing in (so are we making a prototype, literature study, etc.) | |||
- Complete concept of the workings of our product and it's parts | |||
- Result of the interviews | |||
- Report about the project in this Wiki | |||
=== Logbook === | === Logbook === | ||
{| class="wikitable" | {| class="wikitable" | ||
|+'''Marysia Huige''' | |+'''Marysia Huige''' | ||
| Line 902: | Line 1,030: | ||
|- | |- | ||
| | | | ||
| | |Brainstorm design | ||
|4 | |||
|- | |||
| | |||
|Research about Bluetooth connections | |||
|2 | |||
|- | |||
| | |||
!'''Total''' | |||
!7 | |||
|- | |||
|4 | |||
|Meeting Monday | |||
|1 | |1 | ||
|- | |||
| | |||
|Write design requirements | |||
|2 | |||
|- | |- | ||
| | | | ||
| Line 912: | Line 1,056: | ||
!'''Total''' | !'''Total''' | ||
! | ! | ||
|- | |||
|5 | |||
|Meeting Monday | |||
|1 | |||
|- | |||
| | |||
|Research stress monitor devices | |||
|3 | |||
|- | |||
| | |||
|Write design proposal | |||
|2 | |||
|- | |||
| | |||
|Actors section | |||
|2 | |||
|- | |||
| | |||
!'''Total''' | |||
!8 | |||
|- | |||
|6 | |||
|Meeting Monday | |||
|1 | |||
|- | |||
| | |||
|Write Testing possibilities | |||
|2 | |||
|- | |||
| | |||
|Make app designs | |||
|2 | |||
|- | |||
| | |||
!'''Total''' | |||
!4 | |||
|- | |||
|7 | |||
|Meeting Monday | |||
|1 | |||
|- | |||
| | |||
|Finish design proposal | |||
|2 | |||
|- | |||
| | |||
|Finish Actors | |||
|2 | |||
|- | |||
| | |||
|Presentations | |||
|3 | |||
|- | |||
| | |||
!'''Total''' | |||
!8 | |||
|} | |} | ||
{| class="wikitable" | {| class="wikitable" | ||
| Line 958: | Line 1,158: | ||
!Total | !Total | ||
!8 | !8 | ||
|- | |||
|3 | |||
|Meeting monday | |||
|1 | |||
|- | |||
| | |||
|Research about dementia and music | |||
|3 | |||
|- | |||
| | |||
|Researching when to play music | |||
|2 | |||
|- | |||
| | |||
|Research about the stages of dementia | |||
|3 | |||
|- | |||
| | |||
|Summarizing findings | |||
|3 | |||
|- | |||
| | |||
!Total | |||
!12 | |||
|- | |||
|4 | |||
|Meeting monday | |||
|1 | |||
|- | |||
| | |||
|Research about relaxing music | |||
|4 | |||
|- | |||
| | |||
|Summarizing findings | |||
|3 | |||
|- | |||
| | |||
|Meeting friday | |||
|1 | |||
|- | |||
| | |||
!Total | |||
!9 | |||
|- | |||
|5 | |||
|Meeting monday | |||
|1 | |||
|- | |||
| | |||
|More research on characteristics of relaxing music | |||
|4 | |||
|- | |||
| | |||
|Research effects of music in brain dementia patient | |||
|4 | |||
|- | |||
| | |||
|Summarizing findings | |||
|2 | |||
|- | |||
| | |||
|Meeting friday | |||
|1 | |||
|- | |||
| | |||
!Total | |||
!12 | |||
|- | |||
|6 | |||
|Meeting monday | |||
|2 | |||
|- | |||
| | |||
|Research about We-Be band | |||
|4 | |||
|- | |||
| | |||
|Research about how physiological data is analyzed | |||
|4 | |||
|- | |||
| | |||
|Summarizing findings | |||
|3 | |||
|- | |||
| | |||
|Working on explaining limitations of our project | |||
|4 | |||
|- | |||
| | |||
|Meeting friday | |||
|1 | |||
|- | |||
| | |||
!Total | |||
!18 | |||
|- | |||
|7 | |||
|Meeting monday | |||
|1 | |||
|- | |||
| | |||
|Research about specific target users | |||
|2 | |||
|- | |||
| | |||
|Cleaning up Wiki | |||
|2 | |||
|- | |||
| | |||
|Write text for presentation | |||
|3 | |||
|- | |||
| | |||
|Prepare for presentation | |||
|4 | |||
|} | |} | ||
{| class="wikitable" | {| class="wikitable" | ||
| Line 1,011: | Line 1,327: | ||
| | | | ||
|Finish summarizing (not yet finished) | |Finish summarizing (not yet finished) | ||
|4 | |||
|- | |||
| | |||
!Total | |||
!12 | |||
|- | |||
|3 | |||
|Meeting monday | |||
|2 | |||
|- | |||
| | |||
|Research wearables | |||
|4 | |||
|- | |||
| | |||
|Brainstorm prototype | |||
|3 | |||
|- | |||
| | |||
|Meeting friday | |||
|2 | |||
|- | |||
| | |||
!Total | |||
!11 | |||
|- | |||
|4 | |||
|Meeting monday | |||
|1 | |||
|- | |||
| | |||
|Research group settings | |||
|4 | |||
|- | |||
| | |||
|Set up mailing list (with Lisa) | |||
|3 | |||
|- | |||
| | |||
|Finalize emails | |||
|2 | |||
|- | |||
| | |||
|Meeting friday | |||
|2 | |||
|- | |||
| | |||
!Total | |||
!12 | |||
|- | |||
|5 | |||
|Meeting monday | |||
|2 | |||
|- | |||
| | |||
|Brainstorm new setup | |||
|2 | |||
|- | |||
| | |||
|Research limitations | |||
|4 | |||
|- | |||
| | | | ||
|Meeting friday | |||
|1 | |||
|- | |- | ||
| | | | ||
!Total | !Total | ||
! | !9 | ||
|- | |||
|6 | |||
|Meeting monday | |||
|1 | |||
|- | |||
| | |||
|Write limitations | |||
|3 | |||
|- | |||
| | |||
|Clean up wiki | |||
|2.5 | |||
|- | |||
| | |||
|Meeting friday | |||
|1 | |||
|- | |||
| | |||
|(I was sick this week) | |||
| | |||
|- | |||
| | |||
!Total | |||
!7.5 | |||
|- | |||
|7 | |||
|Meeting monday | |||
|1 | |||
|- | |||
| | |||
|Make visualizations | |||
|3 | |||
|- | |||
| | |||
|Meeting wednesday | |||
|3 | |||
|- | |||
| | |||
|Presentations and prep meeting | |||
|4 | |||
|- | |||
| | |||
|Evaluation | |||
|2 | |||
|- | |||
| | |||
!Total | |||
!13 | |||
|} | |} | ||
{| class="wikitable" | {| class="wikitable" | ||
| Line 1,026: | Line 1,454: | ||
|Brainstorm | |Brainstorm | ||
|1 | |1 | ||
|- | |||
| | |||
|Planning | |||
|2 | |||
|- | |- | ||
| | | | ||
|Search literature | |Search literature | ||
|3 | |||
|- | |||
| | |||
!Total | |||
!6 | |||
|- | |||
|2 | |||
|meeting monday | |||
|2 | |||
|- | |||
| | |||
|Summarize literature | |||
|3 | |||
|- | |||
| | |||
|meeting friday | |||
|1 | |||
|- | |||
| | |||
|Research sensors | |||
|3 | |||
|- | |||
| | |||
!Total | |||
!9 | |||
|- | |||
|3 | |||
|Meeting Monday | |||
|2 | |||
|- | |||
| | |||
|Summarize research | |||
|3 | |||
|- | |||
| | |||
|Meeting Friday | |||
|1 | |1 | ||
|- | |||
| | |||
|Heart rate variability research | |||
|3 | |||
|- | |- | ||
| | | | ||
!Total | !Total | ||
!2 | !9 | ||
|- | |||
|4 | |||
|Meeting Monday | |||
|1 | |||
|- | |||
| | |||
|Set up mailing list (with agnes) | |||
|3 | |||
|- | |||
| | |||
|Research Dementia & Technology centre | |||
|3 | |||
|- | |||
| | |||
|Set up interview questions | |||
|2 | |||
|- | |- | ||
| | |||
|Send emails | |||
|2 | |||
|- | |||
| | |||
|Meeting Friday | |||
|2 | |2 | ||
|- | |||
| | | | ||
!Total | |||
!13 | |||
|- | |||
|5 | |||
|Meeting Monday | |||
|3 | |||
|- | |||
| | | | ||
|Research Karlijn van Rijen | |||
|3 | |||
|- | |||
| | |||
|Interview Karlijn van Rijen | |||
|3 | |||
|- | |||
| | |||
|Write notes on interview | |||
|1 | |||
|- | |||
| | |||
|Send more emails | |||
|1 | |||
|- | |||
| | |||
|Look into information gathered from interview | |||
|3 | |||
|- | |||
| | |||
|Meeting Friday | |||
|1 | |||
|- | |||
| | |||
!Total | |||
!15 | |||
|- | |||
|6 | |||
|Meeting Monday | |||
|1 | |||
|- | |||
| | |||
|Summarize Interviews with healthcare workers | |||
|6 | |||
|- | |||
| | |||
|Limitations | |||
|2 | |||
|- | |||
| | |||
|Meeting Friday | |||
|1 | |||
|- | |||
| | |||
!Total | |||
!10 | |||
|- | |||
|7 | |||
|Meeting monday | |||
|1 | |||
|- | |||
| | |||
|Meeting Wednesday | |||
|2 | |||
|- | |||
| | |||
|Make & prepare presentation | |||
|5 | |||
|- | |||
| | |||
|Meeting Thursday (also before presentations) | |||
|5 | |||
|- | |||
| | |||
!Total | |||
!13 | |||
|} | |} | ||
{| class="wikitable" | {| class="wikitable" | ||
| Line 1,051: | Line 1,619: | ||
| | | | ||
|Search literature | |Search literature | ||
|1.5 | |2.5 | ||
|- | |||
| | |||
|Summarize literature | |||
|6 | |||
|- | |||
| | |||
!Total | |||
!9.5 | |||
|- | |||
|2 | |||
|Meeting Monday | |||
|1 | |||
|- | |||
| | |||
|Research prototype | |||
|4 | |||
|- | |||
| | |||
|Summarize findings | |||
|3 | |||
|- | |||
| | |||
|Meeting Friday | |||
|1 | |||
|- | |||
| | |||
|Brainstorm after meeting | |||
|1 | |||
|- | |||
| | |||
!Total | |||
!10 | |||
|- | |||
|3 | |||
|Meeting Monday | |||
|1 | |||
|- | |||
| | |||
|Brainstorm design | |||
|4 | |||
|- | |||
| | |||
|Clean up the wiki | |||
|2.5 | |||
|- | |||
| | |||
|Meeting Friday | |||
|1 | |||
|- | |||
| | |||
!Total | |||
!8.5 | |||
|- | |||
|4 | |||
|Meeting Monday | |||
|1 | |||
|- | |||
| | |||
|Update approach, milestones and deliverables | |||
|3 | |||
|- | |||
| | |||
|Clean up wiki | |||
|4 | |||
|- | |||
| | |||
|Meeting Friday | |||
|1 | |||
|- | |||
| | |||
!Total | |||
!9 | |||
|- | |||
|5 | |||
|Meeting Monday | |||
|1 | |||
|- | |||
| | |||
|Restructure Wiki | |||
|3 | |||
|- | |||
| | |||
|Rewrite problem statement | |||
|1 | |||
|- | |||
| | |||
|Help with design proposal | |||
|2 | |||
|- | |||
| | |||
|Start on cleaning up state of the art | |||
|2 | |||
|- | |||
| | |||
|Meeting Friday | |||
|1 | |||
|- | |||
| | |||
!Total | |||
!10 | |||
|- | |||
|6 | |||
|Meeting Monday | |||
|1 | |||
|- | |||
| | |||
|Clean up state of the art | |||
|5 | |||
|- | |||
| | |||
|Find new articles for state of the art | |||
|3 | |||
|- | |||
| | |||
|Summarize new articles | |||
|2 | |||
|- | |||
| | |||
|Meeting Friday | |||
|1 | |||
|- | |- | ||
| | | | ||
!Total | !Total | ||
! | !12 | ||
|- | |- | ||
|7 | |||
|Meeting Monday | |||
|1 | |||
|- | |||
| | |||
|Prepare presentation | |||
|4 | |||
|- | |||
| | |||
|Practice presentation | |||
|2 | |2 | ||
|- | |||
| | | | ||
|Presentations | |||
|3 | |||
|- | |||
| | | | ||
!Total | |||
!10 | |||
|} | |} | ||
Latest revision as of 22:27, 10 April 2025
Group members
| Name | Student Number | Study |
|---|---|---|
| Marysia Huige | 1896431 | PT |
| Mare Hulshof | 1754440 | PT |
| Agnes Kiekebeld | 1882511 | PT |
| Lisa van den Berg | 1497456 | PT |
| Stijn Schroijen | 1840150 | CS |
Problem Statement
In 2020, 55 million people were diagnosed with dementia worldwide. This number is expected to grow to 139 million people in 2050[1]. Two thirds of people living in care homes have dementia[2]. Dementia is a general term for a syndrome that affects memory, thinking and the ability to perform daily tasks. A common symptom of dementia is agitation. When someone is agitated, they feel irritable and restless. People are uncooperative and have difficulties focusing when feeling agitated. They can also show violent or disruptive behavior and have a lack of impulse control. This negative and dangerous behavior could cause dangerous and unpleasant situations for both people with dementia but also for their family, friends, and staff of care homes.
Research has shown that music can have a positive effect on people with dementia. It can help to use music during therapy sessions with a licensed music therapist. Research also shows that music can help outside of therapy sessions. It can help agitated patients feel more calm and it can have a positive impact on a patients heart rate or blood pressure.
Dementia is typically characterized by a disturbance of the higher cortical functions. However, people with dementia can often still remember the lyrics of songs they used to listen to in the earlier stages of life. It seems that the long-term memory for music is often still in tact, even in people in the later stages of dementia and is less affected by the typical metabolic disorders and nerve cell loss. This is the case, because long-term music memory is not located in the hippocampal area, which is were most ordinary memories are stored, but in the supplementary motor cortex, which is responsible for complex motor movements[3].
Currently, music needs to be played by a caregiver or a therapist; there has to be someone to start the music. But what if there is no one present? Then there is no one to play music for a patient when they are stressed or agitated. This is what our project aims to solve. Instead of needing someone to be present, our proposal is that a wearable device will monitor a patient and start playing music when applicable.
So, this project aims to create a well researched design proposal to help agitated dementia patients without needing immediate assistance of a caregiver, by monitoring a patient's stress level and playing music when they are stressed.
Objectives
The main objective of this research is to find a way to calm dementia patients down when they are feeling stressed. It is quite common for people with dementia to be distressed, which can be caused by feeling disoriented, having unmet needs, as well as many other factors[4]. It has been found that music interventions lower anxiety levels and generally make patients (and even caregivers) feel more relaxed [5]. That is why music will be implemented in the design to alleviate stress. In order to further assess what we want our design to achieve, we will be using the MoSCoW method.
Must have
- A calming effect on the patient
- A stress sensor of some kind to determine when the music should be turned on
Should have
- Music from the patients youth
- Comfortability (if the stress sensor is wearable)
Could have
- A calming effect on the caregiver
- Slowly increase volume to limit the shock
- A wearable stress sensor, e.g. using HRV in the same way that a watch measures stress [6]
- A stress sensor based on sound
Will not have
- Scaring the patient by sudden loud music
Users (and their requirements)
The target users of this design are people with dementia, particularly those in the mid-to-late stages of the condition. Dementia affects cognitive functions such as reasoning, memory, and emotional regulation, making patients more prone to stress, anxiety, and agitation. This has detrimental effects on their well-being.
It has been found that in the brains of people with Alzheimer's Disease the musical memory regions are largely spared and well-preserved. For this reason, music can be very effective in retrieving musical memories for these people and reducing stress. One study studied the effect of music intervention on patients with severe dementia and found there is a short-term improvement in emotional state [7]. Recognition of familiar music was particularly considered as emotionally meaningful for people in the late stages of dementia [8].
Given the cognitive impairments associated with dementia, the design of the aid to measure stress and play music must function autonomously with minimal user input. Furthermore, as most individuals with dementia belong to an older demographic, potential physical limitations should be taken into account. It is essential that the stress sensor is easy to use and imposes minimal physical constraints to ensure comfort and practicality. Potential perceptual limitations are also important to consider. The volume of the device for playing music must be able to be adjusted to an appropriate level. The music should be loud enough for the patient to actually perceive the music, but it should not be too loud, since this could only contribute to the distress.
Another crucial user requirement is the personalization of the aid. Both in the measurement of stress and for the intervention in the form of playing music, personalization is needed. Personalization allows the aid to calibrate to a user's unique stress patterns, ensuring more accurate responses. Furthermore, since music preferences vary from person to person, the system must be capable of playing the specific music that elicits positive emotions for each individual. This personalization is essential for effectively reducing stress levels and providing a soothing experience.
Since the caregivers of people with dementia are often also affected by distress of these individuals, they can be considered secondary users. They play a vital role in setting up and managing the device, selecting appropriate music and monitoring its effectiveness. To avoid adding to their workload, the system must be as simple to use as possible. They might also be the people buying the device so it would be beneficial for us to take their wishes into account (from a marketing perspective).
From our interviews it became apparent that the device is most likely to be a success when used by people still living at home. For people living at nursing residencies the device can only be of use when they are in their own room. Since the music will be played on an external speaker, it is not feasible to use the device in group settings such as the dining hall of a nursing residency. Furthermore, in such group settings, there are always caregivers who can also help calm down the agitated patient, whereas the purpose of this device is to help patients with dementia calm down when there is no one around to immediately help them. Elderly people still living at home are more often in the situation that there are no caregivers around, that is why they are our main target group.
Research
Possible Stress Measurement Techniques for Wearable Devices
Stress is a physiological and psychological response to external stimuli, influencing various bodily functions such as skin conductance, heart rate and brain activity. Wearable sensors for monitoring stress are increasingly incorporated in consumer products such as smart watches. However, selecting the right combination of sensors for a wristband involves balancing accuracy, comfort, and practicality. In this section we explore several different stress measurement techniques and evaluate which are the best options to implement in wrist-worn wearables. This way we can make the optimal choice of features to incoporate in our design proposal.
Electrocardiography (ECG) - Heart Activity Measurement
ECG measures the electrical activity of the heart, specifically heart rate variability (HRV). A lower HVR often indicates higher stress levels. In order to be able to conduct an ECG, electrodes are placed on the skin, commonly in the form of a chest strap or adhesive patches.[9]
Advantages
- It offers a highly accurate form of stress detection
- It directly measures heart rate fluctuations related to autonomic nervous system activity.
Disadvantages
- It requires precise placement, which is difficult when used in daily life
- It produces large amounts of data, requiring professional interpretation
- It is not easily integrated into a wristband due to placement limitations
Photoplethysmography (PPG) - Optical Heart Rate Monitoring
PPG uses LED light reflection to measure blood volume changes in the capillaries, indirectly determining heart rate and HRV. An LED-light is shown onto the skin and a sensor measures the amount of light that is reflected back. The more light is reflected back, the lower the blood volume. This technology is widely integrated into smartwatches and wristbands.[9]
Advantages:
- The sensor is small, requires little power and is suitable for wearables.
- Provides real-time heart rate and HRV data
Disadvantages:
- less accurate than ECG, especially in high-motion environments
- Affected by skin tone, environmental light, and sensor placement
Galvanic Skin Response (GSR) - Skin Conductance Measurement
GSR is also referred to as electrodermal activity (EDA). GSR measures skin conductivity, which increases as sweat glands activate under stress. This is a direct indicator of autonomic nervous system activity. GSR works through electrodes on the skin that measure the electrical conductivity of the skin.[9]
Advantages:
- Quick detection of emotional responses
- Works well for short-term stress measurement
Disadvantages:
- It is sensitive to environmental factors like humidity and temperature
- contact with the skin is needed and proper positioning for accurate results.
Skin Temperature (ST)
Stress can cause fluctuations in peripheral skin temperature due to changes in blood flow. Wrist-worn thermistors or infrared sensors can detect these changes.[10]
Advantages:
- Non-invasive and easy to integrate.
Disadvantages:
- It is not always a direct stress indicator. Temperature can fluctuate due to other factors. It is more suitable as a secondary sensor that can complement more accurate sensors.
Blood Pressure (BP) and Blood Oxygen Saturation (SpO2)
Blood pressure increases under stress, however it can also fluctuate due to other physiological factors.
Stress and anxiety can alter an individual's breathing, thereby altering the oxygen saturation in the blood. [10]
Advantages:
- Provides additional physiological insights
- Blood Pressure is linked to cardiovascular health, making it useful beyond stress monitoring.
Disadvantages:
- Wrist-based blood pressure measurements lack clinical accuracy
- Oxygen saturation fluctuations are not always directly linked to stress.
Which indicators and sensors to use
Based on the strengths and weaknesses of each technology, the best combination of sensors to incorporate in a wristband would include either measures of heart rate variability (HRV) (preferably PPG) or sensors of Galvanic skin response (GSR) as primary sensors. As an addition, skin temperature sensors or blood pressure sensors can be implemented as secondary sensors to enhance accuracy.
The Role of Music in Stress Reduction
Numerous studies have demonstrated that music can significantly lower stress and anxiety levels. For instance, Nilsson (2008)[11] reviewed 42 randomized control studies and found that soothing music - typically characterized by a tempo of 60 to 80 beats per minute - was particularly effective. Interestingly, the majority of participants responded best to self-selected music, whether it was their favorite songs or choices made from a curated list of genres.
Music has an influence on people's mood and stress in several ways. In this section an overview of the effect of music on different aspects of stress and mood will be presented.
How Music Affects Brain waves
The relationship between music and brain activity is profound. Research indicates that music can alter brain waves, which reflect mental states. When individuals focus on rhythmic stimuli for an extended period, they can reach new levels of awareness. As they engage with the rhythm, their brain waves synchronize with it, promoting relaxation and reducing stress.
Biochemical Effects of Music
Listening to music also impacts brain chemistry. Multiple brain imaging studies have shown that the brain's responses of listening to pleasant music involve the same regions involved in reward and pleasure[12]. The neurotransmitter dopamine, associated with the brain's reward system, is released when we enjoy pleasant music, contributing to feelings of happiness. Additionally, serotonin, which regulates mood, is increased by enjoyable music and decreased by unpleasant sounds. Slow music has been shown to lower levels of norepinephrine, a hormone that regulates arousal, further aiding in relaxation.
Endorphins, known for inducing feelings of well-being, are also influenced by music. While techno music may lower endorphin levels, classical music tends to elevate them, showcasing the diverse effects different genres can have on our biochemical state.
Music and Cortisol Levels
A major stress system in the human body is the hypothalamus-pituitary-adrenal (HPA) axis. The main effector of the HPA axis is cortisol, also commonly referred to as the 'stress' hormone. Cortisol levels increase in responses to stress and increased cortisol levels can reflect both psychological and behavioral stress[13].
Cortisol levels are commonly elevated in the elderly. These higher cortisol levels are associated with poorer cognitive abilities, a higher risk of cognitive decline and also faster cognitive decline[14]. It is thus of reasonable importance to try and lower these levels as much as possible.
The impact of music extends to cortisol levels as well. Exposure to music has been shown to reduce elevated cortisol levels, effectively counteracting stress. Notably, major key compositions are more effective in reducing stress and cortisol than minor key pieces. Conversely, techno music can increase stress hormones, while classical music is linked to lower cortisol levels.
Physiological Responses to Music
Musical stimuli, particularly rhythm and tempo, can influence physiological responses through a process known as entrainment. This principle suggests two objects vibrating at similar frequencies will resonate together. For stress reduction, music should ideally have a tempo at or below the resting heart rate (less than 80 beats per minute), predictable dynamics, fluid melodic movement, pleasing harmonies, and regular rhythms. Instruments like strings, flutes, and pianos are particularly effective in creating soothing soundscapes.
Music with slow, steady and repetitive rhythms can exert hypnotic effects, contributing to relaxation. By occupying the brain's attention channels with meaningful and soothing auditory stimuli, music can effectively distract from stressors in the environment.
Individual Preferences and Cultural Influences
It is crucial to recognize that responses to music are not uniform; they vary based on individual factors such as familiarity, preference, current mood, and musical training. Research has shown that subjects from diverse cultures can identify emotions conveyed by music, suggesting a universal connection to musical expression. However, personal preference plays a significant role in the effectiveness of music as a stress-relief tool.
Cultural traditions greatly influence affective responses to music. Therefore, it is recommended that healthcare professionals, such as nurses, consider cultural differences in music preferences when selecting therapeutic music. Studies indicate that participants often prefer no music over prescribed music, highlighting the importance of personal choice in achieving relaxation. The correlation between relaxation and enjoyment of music emphasizes that familiarity and pas experiences can override the inherent qualities of the music itself.
Conclusion
In summary, music serves as a powerful tool for stress reduction, influencing brain activity, biochemistry, and physiological responses. The type of music, its tempo, and personal preferences all play critical roles in its effectiveness. Understanding these factors can help individuals harness the therapeutic potential of music to alleviate stress and enhance well-being.
Effective types of music
Not all types of music are equally effective in the reduction of stress. Multiple studies have shown that music that is familiar to the person with dementia has better effects than unknown music. Each person's history, identity and significant moments from their lives are intimately correlated with their musical taste[7]. Furthermore music that the person has come to know in their youth or as young adult has the best effect. This music often elicits strong memories and emotions, which can help in the reduction of stress and mood improvement. It has been shown that both live music and pre-recorded music work in reducing anxiety.
It seems that specifically the rhythm and melody of the music stimulate calming effects, promoting relaxation and reducing stress levels [8].
Research indicates that relaxing music often scores high in aesthetic value, familiarity, and acoustic features. In contrast, non-relaxing music is typically marked by higher energy, loudness, and word density. While relaxing music may contain lyrics, their emotional impact is often overshadowed by melodic elements. Studies suggest that melodies, rather than lyrics, primarily influence emotional perceptions[15].
For people with dementia living in elderly residents, another way in which music can be a relaxing factor, is in that relaxing music can buffer the noise coming from various sources and can decrease the resident's perception of these noxious noises. This in turn lessens the physiological and psychological responses to the noise, including agitated behavior. This, however, would only be effective under the condition that the music is a few decibels above the noise level of the noxious noises. This way some of the primary sources of agitation (e.g. personnel helping other residents) may be decreased and a sound source that is intentionally relaxing is introduced.
Key Characteristics of Relaxing Music
- Instrumentation: Relaxing music tends to be acoustic and instrumental, allowing the listener to immerse themselves in the sound without the distraction of lyrics[16].
- Rhythm and Tempo: The rhythm and pace of music are crucial, with relaxing selections often featuring slow tempos, around 60 beats per minute. This tempo aligns with the natural rhythm of the human heart when at rest[16]. Furthermore, the music should comprise mostly strings with minimal percussion and bass[11].
- Dynamic Range: Sedative music typically exhibits a small dynamic range, with sustained melodic lines and minimal fluctuations in volume. Gaston (1952) noted that sedative music features slow attacks and simple rhythms with significant repetition[16].
- Familiarity: Familiarity with the music plays a significant role in perceived relaxation. Listeners often prefer music that resonates with their experiences, leading to positive sensory experiences and beneficial chemical changes in the body[16].
- Volume level: It has been found that loudness is a characteristic of non-relaxing music[15]. Suggested is that music used for relaxation should have a maximum volume level of 60 dB[11]
- Timing of onset: Research has shown that music can best be played at moments in which a patient experiences acute distress, especially when patients show signs of agitation. However, one should be careful that the sudden playing of music is not an additional stressor for the patient.
Interviews
To get more information and opinions from people that work with people with Dementia, we have decided to conduct interviews. We contacted care homes and caregivers to ask if or how they incorporate music in their care and if they do, how it impacts their patients. We also asked them for their opinion our product proposal so we can get feedback from the people that would be the actual users of the product if it was to be made.
We also contacted the research group Dementia & Technology from the TU/e itself. This way we could ask actual experts on the topic about their opinions on our proposal.
Since caregivers are people with very busy schedules we decided to not only ask them if we can have a conversation but also send them a list of questions that they can answer if they do not have the time to have an actual conversation with us. This way we could still get their opinion, even if they could not meet with us.
For the research group we asked them if they were available to have an in person meeting with us, since we thought they would have more time and be more open to talk with students. We prepared different questions for the people from the research group since we wanted to ask them more about researching people with Dementia and how they deal with the complications that come with it, and if they had any feedback on our product proposal.
In this section we will provide the analysis and most important findings of the surveys and the conducted interview. For a more detailed description of the asked questions and responses, we would like to refer to the appendix.
Analysis of caregivers responses to the conducted survey
There were 6 replies to the email we send out. Some were shorter than others, and others answered all questions asked. One person explained that music is almost always a part of dementia patients lives. Music can be personalized and ‘normal’ technologies are used, like headphones, stereo’s, pick-up’s, tv’s, live music and, sometimes also music therapy.
In the surveys we asked for the caregivers personal experience with dementia patients. One of the questions we asked was what are the ways you notice a patient is agitated? Responses were in line with our literature research. Most often body language examples are given like clenching of muscles (in body or face), panic look in their eyes, pushing doors, plucking things, looking around the room, and all caregivers gave the example of restlessness and walking behaviour (‘loopgedrag’). Verbal examples were also given like talking a lot, or talking very little, curt replies, not accepting help or getting emotional.
We also asked if there are certain moments in a day when a patient is most agitated. The caregivers all agreed that it there are many reasons why a patient can get agitated. Multiple caregivers, explained that some reasons a patient can get agitated if something upsetting happened just before or if a feeling of safety is disturbed. Changes are difficult for patients with dementia which can also result in agitated behaviour. A bad night sleep can warrant agitated behaviour or moments of care because these are moments a lot is asked of a patient. Activities can have many stimuli and someone can get overstimulated. After a family visit patients can also tend to get upset. One specific caregiver noted that sometimes dementia patients get agitated around 16.00 in the afternoon. For our design it would be good to help aid with music during these moments to prevent agitation.
Our device should help reduce agitation in dementia patients but to design this in the best way we were interested in what other interventions were most used in these cases. Depending on the personality of a patient some interventions given were to let the resident feel their emotion and leave them alone. Caregivers also try to find out what caused the agitation and if possible remove this causation so the patient feels in control again. Going outside or going to their own room also helps, caregivers try to find a quiet environment to help calm the patient. The last example, and most interesting to us is to play the residents favourite CD’s. This shows the relevance of our device for both patient and caregiver in these situations.
Diverse music is played throughout the day because different patients prefer different music. Most people feel emotions from the music based on their past and/or memories. Even people further along in the dementia process recognise music. Depending on patients music can also trigger sad memories which in turn can make a patient sad or agitated. Music is mainly used as a distraction and the music stimuli should have a positive effect. When someone has too little stimuli music is a useful tool. A caregiver also explained that nature sounds combined with slow music or meditation music, like singing bowls, or handpan can also have a positive effect. This was also corroborated by Karlijn van Rijen.
Sometimes music does not work because if someone is overstimulated music can only add more stimuli which is the problem in the first place. Sometimes the stimuli or negative thoughts are just too strong. Wrong music or too loud of music (/sounds) can be a trigger and instead of having a calming effect music will have a agitative effect. Sometimes a patient (that is further along in the dementia process) cannot say no to the music and this also causes frustration.
Based on the surveys it would be hard for the prototype to be used in group settings. The loudness of the device is a concern, but the caregivers would find it ideal if it could also work in group settings. Based on the information gathered above this would be difficult to make work because every person responds different to different kinds of music. Unless of course in the very unlikely circumstance, all patients in this group setting have the same preference.
Four out of five caregiver saw potential to use this device in practice, whether that was for all patients or for only one. The last caregiver thought it would be better to use this for people who still live at home and thought it would be interesting to have a sensor that measures when a person has ‘bewegingsdrang’ (urge to move/ walking behaviour) and then starts playing music.
The caregivers gave us great feedback and gave us some suggestions to include in the design. The urged us to design the device in such a way that it takes a resident’s life history. The device should have a friendly appearance that should not be too big and can be put down. It should be able to withstand falling and being thrown. The volume should be easily adjusted and the device should be easy to clean
Analysis of interview with Karlijn van Rijen from the TUe Dementia & Technology research group
Humesock is a sock that measures stress and visualizes this. Through early warnings, timely reactions are possible before escalation. It might be a possibility for us to try and find what kind of algorithms this device uses for our own product.
It is important to consider whether something is a pacifier technology. We have to be cautious of possible ethical risks. For example, our device should is not to be used as a quick fix, since that would be inhumane.
Furthermore, Karlijn van Rijen indicated that it would also be good to research other audio than just music. For example ambient sounds are also promising in the reduction of stress.
An important thing to consider about the wearable itself is the physical form our device would have. Wearables can be quickly stigmatizing and feel uncomfortable. It might therefore be an idea to do research about what types of wearables we could use (e.g. socks or rings that monitor stress). Furthermore, people with dementia often take of these kinds of wearables, so good research about wristbands used by people with dementia is important.
It is also important to consider how we make sure people want to buy our device. It is good to know the current need for our product and it would be nice to chart this. It is important to consider who our target users are and what they are willing to spend on a device that achieves what we intend our product will be achieving.
Design Proposal
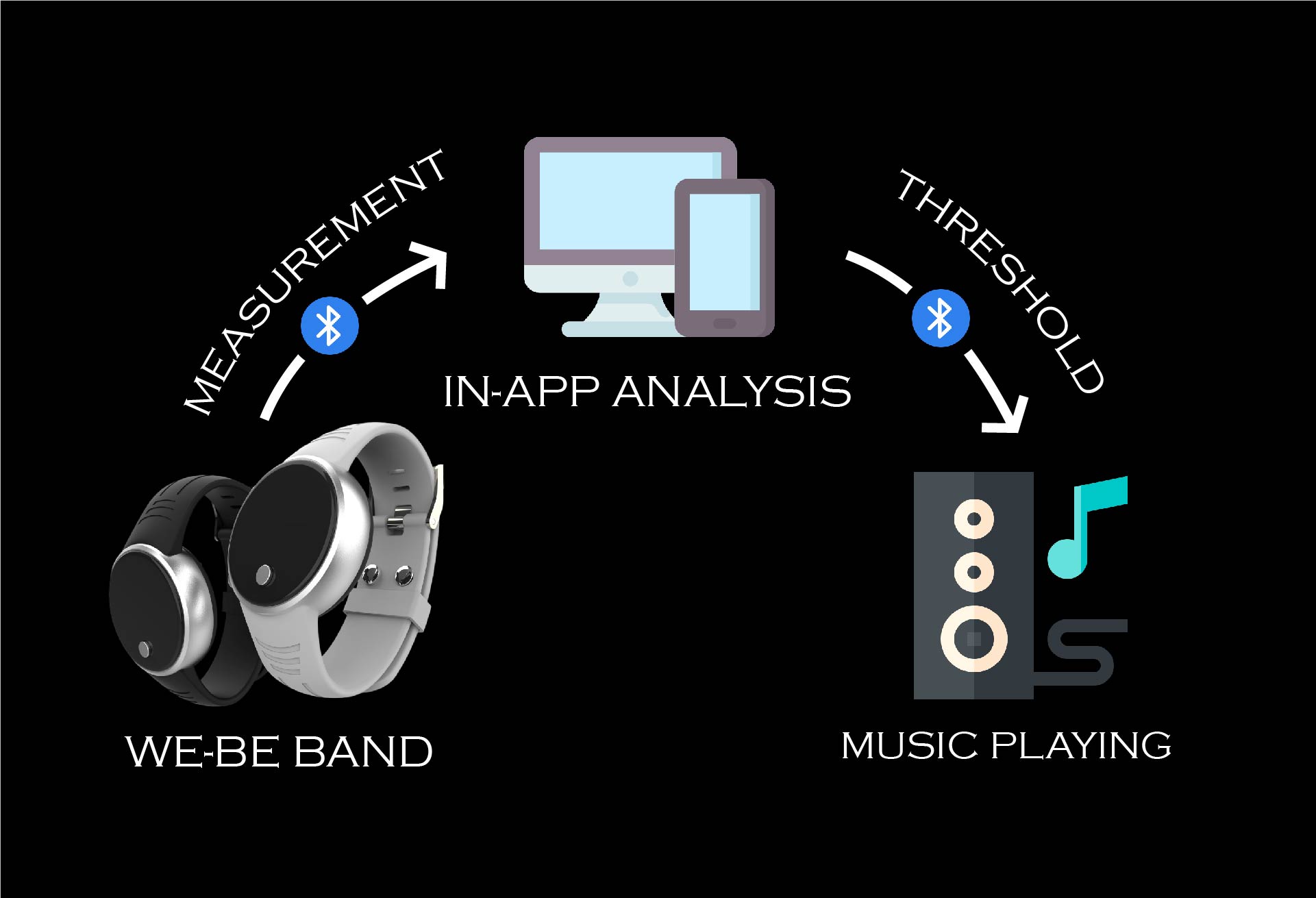
Our product, named Zola, is designed to start playing music if the measured HRV and EDA (which is the same as GSR, as noted before) levels of the patient have trespassed a certain level. We will call this stress threshold the ‘stress-level’. The HRV and EDA will be measured by a stress monitor device worn by the patient. The patient should have the Zola app downloaded on their smartphone which will receive and analyze the data measured by the stress monitor.
If stress is detected by the monitor, and thus the stress-level has been reached, the app will start playing music through an external speaker. This speaker can be any device that can be connected to the smartphone via Bluetooth (e.g. portable speakers or hearing devices with Bluetooth). The volume will start from 0% and increase gradually until the preferred volume that the user/caregiver has set in the app is reached. The music will stop playing once the measured data is below the stress-level or if the user/caregiver has clicked the on/off button in the app. If the user’s stress-level has not decreased, caregivers that have connected their Zola account to the patient’s Zola account, will get a notification.
Because our design is using an external speaker, it will be more affordable for users that already own a good speaker. This also makes our design more sustainable, since there is no need for producing a new speaker for our design.
Actors
Stress monitor device
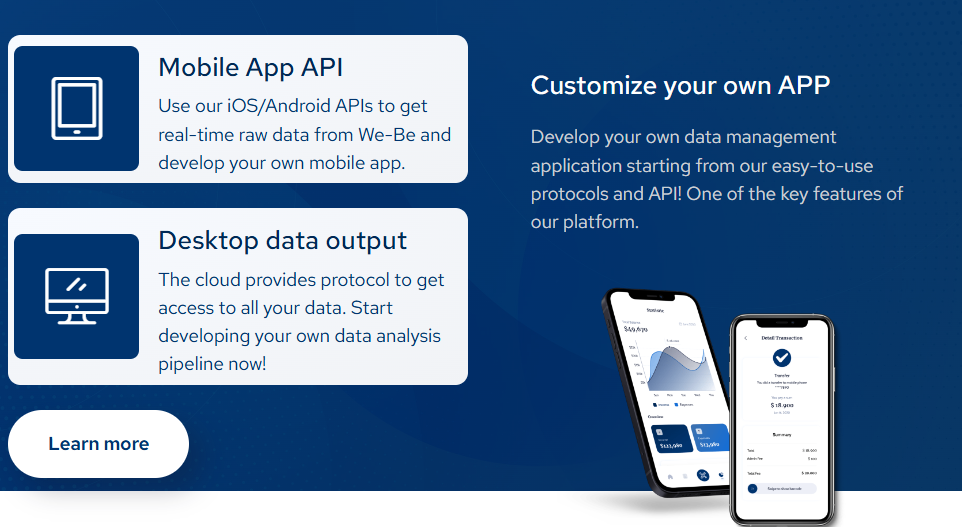
After researching and comparing different types of stress monitor options, it appears that the best stress monitor for our design is Health eTile's We-Be band.
The We-Be band by Health eTile is a wristband used for precise and continuous monitoring of measurements such as HRV, EDA, temperature and an estimation of blood pressure. We-Be uses Bluetooth Low Energy protocol and offers excellent connection and low-latency data transmission. Furthermore, this wristband has a battery life of up to two weeks. Moreover, the We-Be band has a user-friendly design which is important since our users would have to wear the band throughout the entire day. With the We-Be band, it is possible to use the Health eTile’s iOS/Android APIs to retrieve the raw data from the wristband and develop our own app.
Patient
The patient is required to wear the stress monitor device throughout the day. If the patient is still able to do so, despite their dementia. They can indicate their preferred choice of music and maximum volume settings during the initial setup of the application and device.
Caregiver
Caregivers play a crucial role in ensuring that the We-Be band and the patient's smartphone remain adequately charged. Given that the We-Be band has a battery life of up to two weeks, maintaining its charge should add to much to their workload. Additionally, caregivers are responsible for setting up the app and the device by configuring the preferred settings in the patient's account. In instances where the patient is unable to put on or remove the wristband as needed, caregivers must also assist with this task. Finally, caregivers are required to create their own Zola accounts. This step is essential for enabling them to receive notifications regarding the patient's stress levels, thereby making it possible to intervene when necessary.
Smartphone app
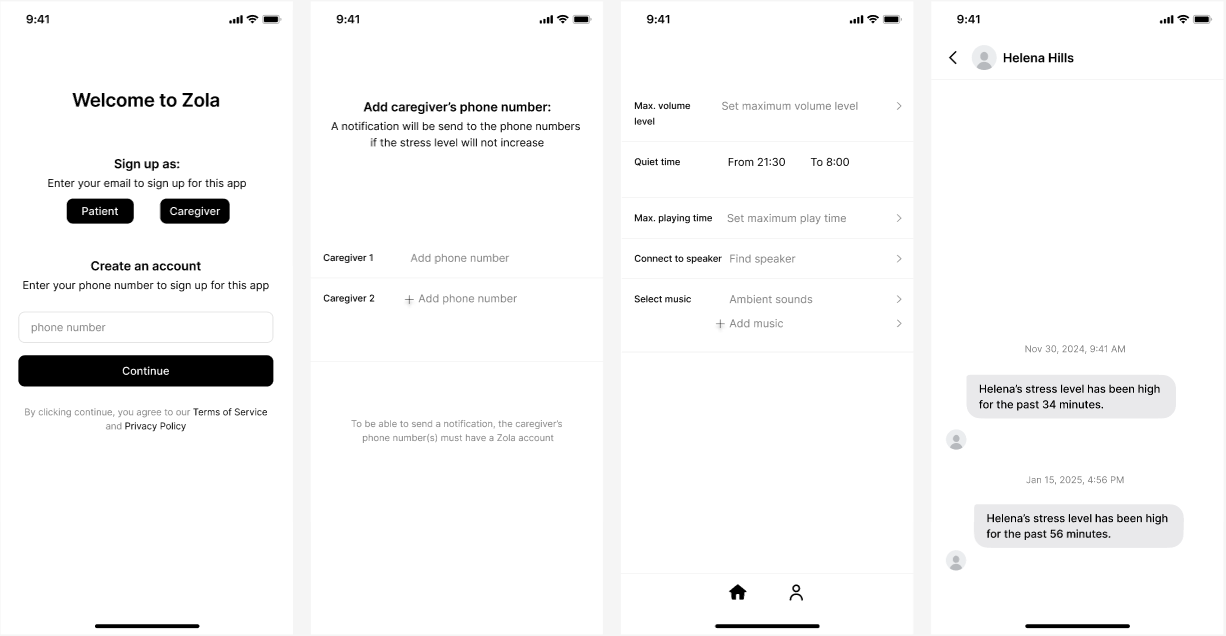
The app on the smartphone of the user collects and analyses the data received from the stress monitor device. If the HRV and the EDA data is above a certain stress level threshold, the app will start playing music from volume 0% up to the maximum set volume through Bluetooth via an external speaker. Furthermore, the user can set the maximum playing time. Once the music has been playing longer than the max. playing time, a notification will be send to the caregiver's account. The app also has the option to let the user add their own preferred music. Furthermore the user or caregiver can set up a timeframe referred to as "Quiet time", during which no music will be played if the measured data shows signs of stress. This can be helpful for users that do not want to be disturbed by music while they are sleeping.
In the figure from left to right is showcased:
The sign-up screen, the screen where caregivers can be connected to the patients, the settings that the patients can set on their account, and the notification chat that the caregivers will receive when a patient is stressed longer than the set maximum amount of time.
Bluetooth speaker
The speaker will play the audio that is set in the app by the user starting at volume 0% and increasing to the set maximum volume. In our design, any speaker that can be connected to the user's smartphone through Bluetooth can be used. Think of a portable speaker but also for example hearing aids with Bluetooth can be connected.
Design requirements
- The app should automatically connect to the external speaker via Bluetooth when the patient is within it's range.
- The data measured by the stress monitoring device should be used only for this device purposes and should be saved securely without scolding the user’s privacy.
- The user or caregiver should be able to easily stop the audio through a ‘stop’ button in the app.
- If there is no speaker currently available, the app should continue playing music through the smartphone instead.
- The app should have a clear User Interface
Scenario
Phase 1: Start measurements
- The user or caregiver downloads the app and makes sure the wristband is charged.
- The monitoring device starts measuring the HRV and the EDA of the patient.
- The measurements are sent in real-time to the smartphone app
Phase 2: Monitoring & analyzing measurements
- The app analyzes the received raw data and compares it to the stress level threshold.
- If the received data does not exceed the threshold, nothing happens.
Phase 3: Stress detected
- If the received data is above the threshold, the app will connect to the external speaker through Bluetooth.
- The speaker will play the audio that is given by the user in the app. The volume will increase from 0% to the maximum volume that is set by the user in the app.
Phase 4: Stop measurements
- The music will stop playing if:
- The ‘stop’ button in the app is pressed.
- The measured stress levels decrease and are under the threshold stress levels
Analysis of Data
When the We-Be band is connected to a gateway, which could be either a mobile phone or a PC, the data is automatically analyzed and users can visualize the data in real-time. The We-Be band monitors a wide range of bodily functions. Some of these are particularly relevant for assessing stress, including EDA (electrodermal activity), HRV (Heart rate variability) and temperature. The monitoring of these physiological signals and machine learning are integrated by implementing state-of-the art algorithms. This ensures real-time stress evaluation can be provided.
In order to measure HRV, the We-Be band uses photoplethysmography (PPG). The band is equipped with four channels of PPG signals which offer accurate and stable measurement. Multiple automatic PPG annotation modules are integrated in the We-Be platform to clean the raw PPG signals and provide clean signals which can be analyzed[17].
To illustrate in a bit more detail how the We-Be band accomplishes the analysis raw signals, the analysis of EDA signals is detailed in the section below.
EDA analysis
Electrodermal activity (EDA) is one of the most sensitive indicators of emotional responses, arising from the spontaneous activation of sweat glands in the skin. It is intricately linked to mood, arousal, and attention. Due to its high stability, ease of measurement, and great sensitivity, EDA has become the most effective physiological parameter for reflecting changes in sympathetic nerve activity[17].
EDA signals are composed of two main components: a tonic component (skin conductance level - SCL), which is a slowly varying signal that establishes the baseline level of EDA, and a phasic component (skin conductance response - SCR), which is a rapidly fluctuating signal directly associated with the activity of the sweat glands, which respond to stimuli such as stress or emotional changes[18].
The We-Be band incorporates pyEDA, which is an open-source toolkit that can be used to process EDA signals using statistical analysis and automatic feature extraction. It is noteworthy that EDA in pyEDA should not be confused with EDA - GSR (Galvanic Skin Response). In this context, EDA refers to Electronic Design Automation, a field focused on optimizing productivity in the design and manufacturing of electronic components[19].
Processing EDA Signals using pyEDA
The EDA signals collected by the We-Be band come in a raw format and contain motion artifacts. To effectively use the EDA signal to predict stress, several crucial processing steps need to be undertaken to remove noise and extract a clean signal. An article by Aqajari explains how the pyEDA toolkit does this[20].
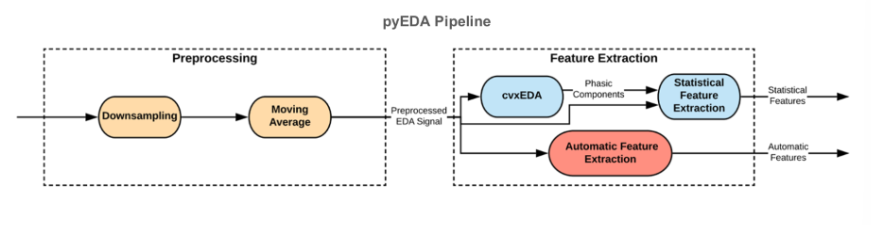
The pyEDA toolkit processes EDA signals through a structured pipeline that includes a pre-processing and feature extraction stage.
In the pre-processing stage, the raw EDA data undergoes several steps to enhance its quality. The first step is down-sampling. EDA data is typically sampled at a higher frequency than necessary. By reducing the sampling rate, the memory usage and processing can be decreased, while retaining essential information. The next step is moving averaging. This technique smooths the data, helping to eliminate artifacts caused by physical movements and gestures, ensuring that the signal reflects true physiological responses.
Once the data is pre-processed, the meaningful features critical for stress detection are extracted in the feature extraction stage. Features can either be extracted by statistical feature extraction or automatic feature extraction. A key component of statistical feature extraction is the cvxEDA algorithm, which separates the EDA signal into its tonic and phasic components. This is needed because then rapid changes in the EDA signal which correlate with stress responses can be accurately identified.
After the EDA signals have been processed and features extracted, machine learning algorithms are used to build predictive models. These analyze the extracted features to identify patterns associated with stress.
Testing Possibility
Technical tests
Multiple technical tests should be performed to test the functionality of the prototype. These technical tests should:
- test whether the data is send to the smartphone continuously.
- test whether the app retrieves the real-time data.
- test the Bluetooth connection between the app and the speaker.
- test whether the app connects to the speaker when the data reaches the stress level.
- test whether the on/off button and the volume button work in the app.
User test
Once all technical tests have been performed, user tests can be conducted. This test will evaluate what the effect of our prototype is on the stress levels of the patients with dementia. The user test contains a control group and a test group.
Test group:
The participants will be wearing the We-Be band. If the measured data reaches the stress threshold, a connection will be made between the app and the speaker allowing the speaker to start playing music.
Control group:
The participants will be wearing the We-Be band. If the patients reach the stress level, no music will start playing.
After conducting this experiment, data will be analyzed to find whether the stress level of the patients in the test group will decrease faster than the stress level in the control group. Furthermore, interviews or questionaries would be conducted with the caregivers and/or family of the patients. From this data, we will be able to have an insight of the effect of our prototype on the patients and the caregivers workload from the caregivers’ point of view.
Limitations and future additions
Stress measurement
This technology greatly depends on the accuracy of the stress measurement. If the stress is not measured accurately, the device could turn on at undesirable moments. The effectiveness of the music intervention depends on different factors. Firstly, the sensor placement of the wearable is important, especially when measuring HRV and EDA. To get accurate measurements the wearable should have proper skin contact. If the wearer moves around a lot, that can have a negative effect. Additionally, the EDA data can be influenced by external factors such as humidity.
Music choice
Based on the research we conducted, it was found that reactions to music are not uniform. This implies that a song can make one user very calm, whereas it can have the complete opposite effect on someone else. Because of this, the family and caregivers should be able to curate their own playlist. This can however be difficult if no one know what music a patient used to listen too, or what music used to calm others down. For future additions, we could implement AI to create music. It can start out with music that is generally found to be "calming" and adjust the music based on the physiological reactions of the user.
Furthermore, it has been found that other auditory cues rather than just music can exert the desired relaxing effects. For example sounds as the flowing of rivers or the falling of raindrops can also work for stress relieve. In further research and development in this device the playing of these sounds rather than music when stress is detected could be a valuable extension[13].
Different stages of dementia
The way that the product can be implemented also greatly depends on the stage of dementia that we focus on. In our case, we decided to focus on medium to late stage dementia. This makes it hard for the patient to remember what music they like, so they will most likely not be able to express their preferences themselves. Based on our research[22] we found that late stage dementia patients might have diminished response to music. Even if the effect is small, it always seems to be neutral to positive.
Wearable
Research indicates that individuals with dementia often struggle to accept new devices, such as wearables. A study focusing on nursing home residents and their formal and informal caregivers explored perceptions of wearable technologies. The findings revealed that for a wearable device to be accepted by residents, it must meet a specific set of criteria[23].
On key consideration is the size of the wearable; it should be compact and unobtrusive to avoid drawing excessive attention, which could lead to resistance from users. Additionally, the design is crucial. If the wearable resembles a watch, but does not look like a traditional watch, it may not be perceived as suitable for individuals with dementia. Caregivers noted that familiarity in design can significantly impact acceptance, as recognizable forms tend to foster comfort and ease of use[23].
Another important consideration is the placement of the on and off button. If this button is easily accessible to the individual wearing the device, there is a risk that the wearable could be accidentally turned off. People often have a natural tendency to fiddle with objects around them, and a button located on a wristband becomes an inviting target for such behavior. This highlights the need for careful design to prevent unintended disruptions in the device's functionality[23].
Overall, these insights highlight the importance of thoughtful design and user-centric features in developing wearable technologies for dementia patients. The WeBe band, which is used in this project, does not adhere to all these specifications. The WeBe band is quite big and it contains buttons which are easy to be reached by the person wearing it. Further research could explore other wristbands or other types of wearables to measure stress that might be more suitable for individuals with dementia.
Pavlov effect
During research and brainstorming about ideas for this device, the question arose whether a Pavlov effect could occur, creating an association between once loved music and stress. In other words, whether the music could become a stressor in itself due to the association between music and stress. The Pavlov effect is a consequence of classical conditioning, which can be described as the learning mechanism through which certain stimuli become associated with relevant events. These can be either appetitive or aversive. When a Pavlov effect occurs, a person has thus learned that a certain cue predicts a pleasant or unpleasant event[24].
During the project, concerns arose whether the music played when stress is detected, could be interpreted as such a cue predicting an the occurrence of a certain event - in our project, stress. In that case, the music that is supposed to be relaxing could have the opposite effect of being a sign the user is stressed, possibly making the individual even more stressed.
Of course these are only speculations and further research would be necessary to fully understand if this is indeed a legitimate concern.
Survey
In order to gather opinions about our device from individuals who have direct contact with dementia patients, we distributed surveys to several care homes and caregivers. We also sent surveys to the research group Dementia & Technology from the TU/e itself. For a more detailed overview of the questions asked in these surveys, please refer to the section "Interviews", which can be found further down this Wiki page.
While we received some valuable responses, the number of participants in our surveys was limited. With more time allocated to this project, we could have conducted more extensive interviews to gain additional insights from those closely interacting with patients.
Furthermore, we were unable to engage directly with individuals living with dementia. this would have been a significant addition to our research, and in future studies, it would be an excellent opportunity to investigate the actual effects and functioning of our device among dementia patients.
From the interviews we gathered information that we were able to implement into the design, such as the familiarity of a watch as wearable. This is also sturdy like advised in the interviews/ survey. The biggest limitation of our device is the fact that music can help with agitation but it can also have a negative effect if a patient is already feeling overstimulated. This depends on the situation and cannot always be gauged before.
Prototype
Perhaps the most significant limitation of this project is that no physical prototype has been constructed, which hindered the ability to test the device effectively. Our group's academic backgrounds resulted in a lack of expertise in protype development, preventing us from creating a functional and testable model. Consequently, our assumptions about the workings of the device, for example what type of music should be played and the timing of it, are solely based on literature research and insights gathered from our interviews.
In future research, developing and testing a physical prototype would be invaluable for refining the device and enhancing its effectiveness. This hands-on approach could provide critical feedback and insights that are essential for the successful development of our device.

Technology Readiness Level[25]
In the interview with Karlijn van Rijen, she advised us to look at the TRLs (Technology readiness levels) of our idea. TRLs are a method for estimating the maturity of technologies during the acquisition phase. The TRL is determined during a technology readiness assessment (TRA). It has 9 levels and they are described in the following categories:
- Basic Technology Research
- Research to Prove Feasibility
- Technology Development
- Technology Demonstration
- System/ Subsystem Development
- System Test, Launch & Operations
Looking at the TRLs and our device, we made the following assessment. The first level is passed as we have observed and reported the basic principles. The second level is also examined as we have formulated a technological concept and its application. The third level requires experimental proof of concept which we have started by designing what functions we want our device to have and how to apply these functions in practice. We started by looking at the sensors and wearable we want to use. The next steps are not yet taken, our technology is not validated in a lab (level 4) nor in relevant environment (level 5). The technology is also not demonstrated in relevant environment (level 6) nor has a system prototype demonstration in operational environment taken place (level 7). Lastly the system is not complete and qualified (level 8) and it the actual system has not been proven in operational environment (level 9). Ideally these are steps taken in the future developmental phases of the device.
State of the art
We performed a literature study on the current state of the art on several relevant topics.
Technology in dementia care
We found this [26] article on using technology in care for dementia patients. This article summarizes several key areas of technological development in dementia care. The main domains in which there is a lot of technological advancement include: 1) diagnosis assessment and monitoring, 2) maintenance of functioning, 3) leisure and activity, and 4) caregiving and management. Examples of technological advances in the domain of leisure and activity also include systems that use music to soothe patients. In the paper a one-button radio is mentioned, but also a simple interface for making music and systems for collaborative music making. The article ends with the conclusion that, despite numerous technological initiatives in dementia care, adoption rates remain low. Contributing factors include a lack of awareness, challenges in accessibility and insufficient support. The paper emphasizes the need for policies, funding, and practices that go beyond a purely medical approach, advocating for a holistic perspective that includes prevention strategies and ways to support a meaningful life with dementia.
Effects of music with Dementia patients
A lot of studies have been done to research the effects of music on dementia patients. We found several analyses and studies related to the topic.
We found a meta-analysis that looks at four different factors in music therapy for dementia patients [27]. Pedersen et al. performed a meta-analysis to (1) investigate whether music therapy has a positive effect on reducing agitation for patients with dementia. Furthermore, they (2) compare personalized and group music intervention. Besides that, Pedersen (3) evaluates the effect of preferences in music by comparing music based on patient preference without prior consultation with patients or caregivers. Lastly, the study (4) focusses on comparing the benefits of active versus passive music intervention. In active music intervention, participants actively engage by singing, dancing, or playing an instrument. In passive music intervention, participants listen to live or recorded music without actively engaging. The results of this meta-analysis indicate that (1) music intervention does significantly decrease agitation in patients with dementia. Furthermore, the analysis (2) shows that personalized music therapy may have a larger effect in certain cases, however the effect is less consistent across the different studies used in this research. Both individual and prescribed music preferences (3) show a medium effect size. Finally, both active and passive music interventions have similar effects. Passive interventions may work better in different settings. The study performed by Pedersen et al. indicated that music intervention has a reducing effect on agitation of patients with dementia.
We also found a study on the impact of music on the self in dementia patients [28]. This study proposes a theoretical framework which enhances the sense self in patients with dementia. To explain this framework, numerous features of music have been mentioned: Engaging, Persuasive, Social, Synchronization, Physical, Emotional, and Personal. This framework explains how music engages the five aspects of one’s self, namely ecological, interpersonal, private, extended, and conceptual self. The ecological self is the self has it is perceived through sensory information and the environment. Numerous features of music, such as physical, synchronous, engaging, and emotional, are important for this self. The interpersonal self can be explained as the self that socially interacts with others. Here the persuasive and engaging aspects of music play a key role. The extended self shows how the self was in the past and how it might be in the future. The different way of engaging with music, and the personal and emotional features of music contributed to engaging the extended self for people with dementia. The private self exists of experiences that others do not have access to, such as thoughts, beliefs, and experiences. Music can help this self as a new way to express themselves. Finally, the conceptual self is indicated the concept that the individual has of themselves, for example self-identity, roles, and social identity. The researchers of this paper identify the music features and the aspects of the self using two case studies and conclude that music has a unique ability to engage with multiple aspects of the self.
This research paper [29] studies whether the effect of music on dementia is beneficial and if so, why that is the case. The article focusses on three key areas, namely “music and memory”, “music and depression”, and “Agitation and aggressive behaviors”. The article states that some people with dementia remember music longer than they remember and respond to other types of information. Reminiscence music therapy, music therapy that uses familiar songs to trigger memories of the individual with dementia, has reduced working on symptoms of depression. This could be explained by the fact that music induced physical and emotional changes. Furthermore, music could help reduce stress, sooth pain and energize the body. Therefore, music could be used as an aid for mood regulations. Moreover, music has a beneficial influence on reducing agitated and aggressive behaviors of individuals with dementia during various activities and various times. Playing music that is preferred by the participant has the biggest outcome. Music makes sounds more familiar and predictable. This could lead to creating a positive emotional state as people retrieve positive memories.
In this study [30], Sixsmith and Gibson perform qualitative research on the influence that music has on the everyday life of participants with dementia. In-depth interviews were conducted with a sample size consisting of 26 patients with dementia living in either their own homes or in residential care. This paper highlights the benefits of music but also the problems that could arise while listening or actively participating in musical activities. The data from the interviews shows that the beneficial effect of having music in the lives of people with dementia could enhance the feelings of wellbeing. Music could make people with dementia ready to express their happiness both physically and emotionally. Furthermore, music supports valued activities. Playing music in the background while working on a task could make the task more enjoyable for people with dementia. Moreover, music encourages social interaction. During musical activities, most of the participants were accompanied by their family, carers or by other people with dementia. Music therefore is a way for people with dementia to communicate with other sand have meaningful social interactions. Lastly, music gives people with dementia a higher degree of empowerment and control over their own lives. Sixsmith and Gibson state multiple challenges that arise when people with dementia engage with music, such as difficulties expressing their preferences, hearing difficulties, the loss of confidence, and social barriers in care homes.
This research paper [31] focused on the meaning and value of musical intervention for not only people with dementia, but also their families, care home staff and music therapists. McDermott et al. are aiming to explore the meaning and value of music from the people with dementia point of view. The paper also analyses how families, care home staff and music therapists view the effects of music. Furthermore, the paper aims to find a link between psychosocial factors and the results of the study to be able to develop a theoretical musical framework of music in dementia. The qualitative data was ‘gotten’ from conducting focus groups and interviews with care home residents with dementia and their families, care home staff, music therapies, and day hospital clients with dementia. From the data received, it can be concluded that meaningful musical experience could result in people with dementia feeling emotionally connected with other people. Moreover, musical activities lead to social interaction between residents and staff in care homes. That has resulted in a more positive impact on the environment of the care home. The researchers also state that music is linked to personal identity and life history of people with dementia.
This paper [5] shows a meta analysis of the effect of music on dementia patients. Several positive effects of music on patients with dementia have been established in different fields, namely biologically (hr, etc.), behaviorally (less stress, agression, etc.), cognitively (better speech e.g.) and emotionally (more enjoyment in life). It is however, mainly focused on guided music intervention, where the patient is encouraged to sing along, etc.
To gain more insight into the results of trials done with music therapy on patients we found this systematic review [32] . The review was conducted on clinical trials reported from 1 January 1946 to 1 May 2020. The results showed that 13 studies reported overall cognition as an outcome. With 4 showing significant improvements, 6 showing no improvements and 1 with a mixed effect. The studies also showed that effects of music therapy on the memory of patients living with dementia were mixed, with 4 out of 5 studies reporting significant improvements. Music therapy also showed significant improvements for language or verbal fluency. Two studies explored the effects of singing on BPSD and it showed significant reductions in BPSD in patients with dementia. The results were mixed for listening to music and using musical instruments. Most studies also showed a significant reduction in either anxiety or depression or both. Five studies showed that music listening significantly improved mood, while 2 studies did not show this. There were mixed results for the studies of the effect of music therapy on agitation. Six out of eight studies reported significantly reduced agitation when music listening was the primary intervention, but mixed results were observed for the effects of combined music therapy. In one crossover trial in which Baroque music was played an adverse effect was observed and there was a significant increase in the number of episodes of agitated behaviour when music was played. Levels of were reduced in two of the rials and daily functioning reported no significant improvements. Mixed results were reported on the effects of music therapy on the quality of life.
Similarly, we found this review [33] on how and why music therapy reduces distress and improves well-being in advanced dementia care. The review is mainly focused on music therapy with a music therapist present. According to the review, the music therapy has positive effects on patients.
This study [34] from 1997 shows that interest in the topic of using music for care of agitated dementia patients has been there for a long time.
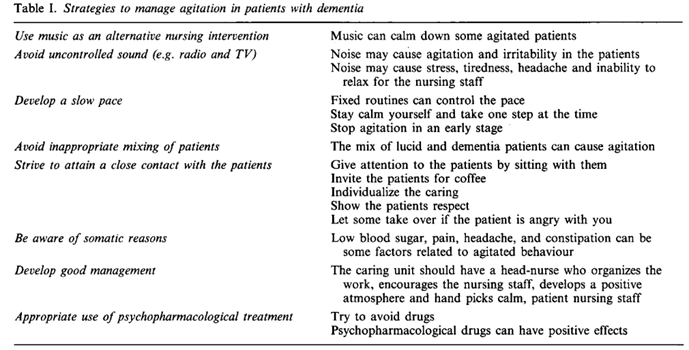
Agitation is defined as a clinical term for inappropriate verbal or motor activity that is not an obvious expression of need or confusion. Repetitions of words, restlessness and aggression are examples of symptoms that can be included in the concept of agitation. The nursing directors of five nursing homes selected 13 staff from six different wards and the directors of four collective residential units selected four staffs. Interviews were conducted with all responders, they lasted about 45 minutes and the following questions were asked:
· Can music be used as a nursing intervention for this group of patients?
· Do you play radio and TV or other forms of music on the ward? If so, in what way does it influence the patients and the nursing staff?
· What are your opinions and experiences regarding pharmacological treatment of these patients and which psychopharmacological drugs would you suggest for an elderly patient showing irritability and aggression?
And they were also asked to summarize what they regarded as the most important aspect of caring, and to draw up strategies for caring of this group of patients. The themes shown in the table were found as strategies to manage agitation in patients with dementia:
We found this analysis [22] on video-recorded sessions where individualized music was played for agitated dementia patients. Agitation is one of the symptoms patients with dementia suffer from. This study investigated whether individualized music could be used as a nursing intervention to reduce such symptoms. The study was done on four patients. There were video recordings during four sessions in four periods. There was a control period without music and then two periods where individualized music was played, and lastly one period where classical music was played. The documented sessions were analysed and the author noted in a protocol if the patient was calm or agitated. To be considered agitated, the patient would be showing signs of being upset, such as beating the table: shrieking/shouting, trying to stand up, irritability, and/or restlessness. Samples of segments were then analysed by KA by means of Facial Action Coding System technique. This technique is used to identify distinct facial muscle movements. The music seemed to affect all patients, but the two who were most affected by dementia reacted the least to the music. Some days a patient was clearly in a bad mood and then the music did not affect them. When asked the patients told the researchers that they liked the music. The study found a decrease in agitation after individualized music was played. The effect of classical music was not as evident.
This article [35] presents a comprehensive analysis of current methodologies that employ emotion monitoring to create music-based interventions for dementia patients. The article examines various technologies and approaches used to assess emotional responses in dementia patients, aiming to enhance the effectiveness of music therapy interventions. By synthesizing existing research, the review highlights the potential benefits and challenges associated with integrating emotion monitoring into therapeutic practices for dementia care. The study underscores the importance of personalized interventions and suggests directions for future research to optimize outcomes for individuals affected by dementia.
Stress measurement technology
Since our product is designed to detect stress in dementia patients through a wearable, we also did research on that topic. We found this article [36] on using a smartwatch to detect stress through sweat cortisol levels and a person's heart rate variability (HRV). According to the article, the technique works quite well to measure stress. This research was not done on dementia patients specifically, but it does show potential in detecting stress in people with a wearable device that measures biological functions.
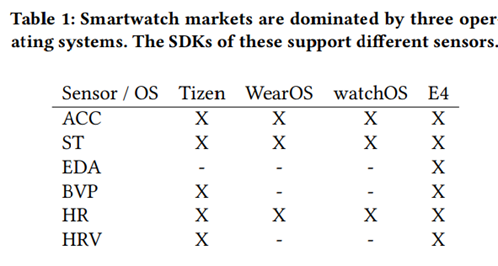
Similarly, we found this article [37] on using the sensors in a commercial smartwatch for stress detection. Stress detection using wrist-worn sensors has recently been studied widely and it has been shown that it can detect stress quite reliably. An example is given where stress was measured accurately at a level of 83% at laboratory conditions. It was measured using skin temperature, electrodermal activity, heart rate, blood volume pulse and accelerometer signals. Most studies use, among other bio-sensors, electrodermal activity (EDA or galvanic skin response). The article concentrates on studying how well stress can be detected using the sensors included to commercial smartwatches. The study concludes that the best recognition rate was obtained using a combination of skin temperature, BVP, and heart rate signals ((LDA: 87.4%, QDA: 84.9%, RF: 82.4%). It concludes that EDA signals are not necessary to use in the recognition process. The article also investigates the effect of window size to the recognition rates and finds that long windows, result in better recognition rates rather than short ones. In their case the best window was 120 seconds.
In this study [38] a fitbit was used to record heart rate data alone. ECG was used to generate HRV parameters. A statistical analysis was done on the results of the participants (medical students). Participants completed the DASS and the general population has significantly higher scores on all of the DASS subscales than the medical students. But it was found that both resting and stress phase HR were significantly higher in the medical student population than the general population. The study is relevant for us because it shows that HRV could be used to predict the quality of response to acute stress. This may aid in developing a physiological algorithm for stress that could be incorporated into wearable technologies. According to the article there were no devices on the market at the time (2021) that have a rigorously validated algorithm for stress detection.
This paper [39] provides a review of several methods for detecting mental stress in different environments using wearable sensors and machine learning techniques. Stress is defined as a psycho-physiological response to challenges that can lead to severe health issues. Wearable sensors collect biological signals that reflect the body's response to stressors. Advantages of wearable sensors include real-time monitoring and non-intrusiveness. In the article, various physiological signals which have potential to be a measure of stress are considered. Each signal provides unique insights into how the body responds to stress. Some wearables integrate multiple of these sensors to measure stress more effectively. The article also discusses some challenges and limitations of wearable sensor-based stress detection.
This article [40] presents a novel method for real-time stress detection using data from smartwatches. The study utilizes an open-source dataset that includes motion and physiological signals, such as heart rate and accelerometer data, collected from wrist-worn devices. After preprocessing the raw data to remove noise and enhance quality, the study applies two deep learning models: a Fully Convolutional Network (FCN) and a Residual Network (ResNet). The results indicate that the FCN model performs better than ResNet and traditional machine learning approaches, achieving high accuracy in distinguishing stress from non-stress conditions. The findings highlight the potential of smartwatches combined with advanced deep learning techniques as effective tools for continuous and unobtrusive stress monitoring. The study concludes that such systems could significantly improve stress management and well-being, particularly in real-world applications.
Wearables for dementia patients
Using wearable technology devices with dementia patients can be difficult. We found this article [41] that discusses the values, attitudes and needs for using wearables for residents of nursing homes. The paper specifically focuses on using wearables with dementia patients and what their needs are. According to the paper, devices that are mounted on the wrist cannot be too tight, as to not hurt the patients. They should be recognizable for dementia patiens, something like a watch. The patient should not be able to turn the device off themselves by a button on the outside, as there were some patients in the research that turned off the device. The device should be water resistant and should not be too bulky. Finally, it would be good for the device to be customizable to fit different patients' needs. All of these requirements are taken into account with our design. The most important thing is the perceived usefullness and comfortability for the patients.
We found another study [42] on what is needed for a stress sensor for dementia patients. The study concludes that a wearable could be integrated into clothing or wristbands for familiarity purposes, it should also be comfortable and it could be customizable to increase user acceptance. To increase acceptance and decrease negative perception the device should be as discreet as possible. The device should also be easy to put on and take off, again to increase patient comfort. According to the study, it is most important that the wearable is washable and safe. The study also provides several perceived positives for stress sensors for dementia patients. Namely, that stress can be identified and early intervention methods can be used to quickly alleviate it. Similarly, the study also provides several perceived negatics that should be taken into account. It is possible that the sensor is not accepted by the user and it could replace the human aspect of care. Both of these possibilities should be taken into account when using stress sensors with dementia patients.
This article [43] discusses the use of wearable sensors for the remote monitoring of elderly individuals. There is a specific focus on how wearables can contribute to healthcare. Several physiological variables that can be measured are discussed, among which heart rate (variability), blood pressure and oxygen saturation. The article makes a distinction between commercial wearables such as smart watches and research prototypes such as smart textiles. It is stated that the commercial wearables are increasing in their reliability of sensors. Several benefits and challenges of wearables in elderly care are discussed. Some of the challenges include the limited battery life of wearables and user acceptance. It is however concluded that wearables provide a promising solution for elderly healthcare by enabling continuous monitoring and early disease detection.
This systematic review [44] examines how sensor-based technologies can be used to track behavioral and psychological symptoms of dementia (BPSD) and assess treatment responses. Analyzing 34 studies, the review highlights the use of wearable sensors such as accelerometers and gyroscopes to monitor physical activity, sleep disturbances, and agitation. It also discusses non-wearable motion sensors and smart home technologies that track movement patterns and behavioral changes in real-world settings. The findings suggest that these technologies are generally effective in detecting agitation, restlessness, and wandering, and they have been well-received as non-intrusive monitoring tools. Some studies also explored the potential of motion data for early detection of mild cognitive impairment. However, the review identifies key challenges, including concerns about data privacy, ethical considerations, and the need for greater user involvement in system design to ensure practical implementation. Overall, the review concludes that sensor-based monitoring holds great promise for improving dementia care, but further research is needed to validate these technologies, address ethical concerns, and develop frameworks for their safe and effective integration into healthcare settings.
Stress in dementia patients
We also found an article on stress in dementia patients in general. In this paper [45], a study is described on the subject of stress as experienced by people with dementia. The study contributes to the supporting of people with dementia, by creating a greater understanding about how people with dementia make meaning from their experience of stress. The questions of interest where how people with dementia perceive their experiences of stress and how they cope with these. It was found that individual personality traits and established coping styles persist and sustain influence in managing stress. This is contrary to previous assumptions that dementia is paired with an inevitable decline and progressive vulnerability to stress. It was furthermore demonstrated that people with Alzheimer's disease demonstrate a preference for "emotion focused" over "problem solving" approaches.
To see if the stress aleviation aspect of our idea is feasible, we found this article [46] that describes the usage of preffered music to reduce anxiety for dementia patients. The article investigates the effectiveness of personalized music sessions in alleviating anxiety among elderly nursing home residents with dementia. Utilizing a quasi-experimental pretest and posttest design, the study involved 52 participants divided into two groups:
- Experimental Group: 29 individuals received 30-minute sessions of music tailored to their personal preferences, delivered by trained nursing staff twice a week for six weeks.
- Control Group: 23 individuals continued with standard care without any music intervention.
Anxiety levels were assessed using the Rating Anxiety in Dementia scale at both the beginning and end of the study. The results demonstrated that the experimental group experienced a significant reduction in anxiety compared to the control group. The authors conclude that implementing preferred music listening is a cost-effective and viable strategy for reducing anxiety in older adults with dementia, emphasizing the importance of individualized care approaches in nursing home settings.
This pilot study [47] explores the feasibility of using wearable technology to monitor and detect agitation in individuals with dementia. The research involved eight participants residing in an assisted living facility, each equipped with off-the-shelf smartwatches and smartphones capable of tracking location, limb movements, vocalizations, and heart rate. Data collected over four-hour observation periods were compared against observations using the Cohen-Mansfield Agitation Inventory (CMAI). The findings indicated that increases in limb movements and heart rate, as detected by the wearable sensors, correlated with observed agitation episodes. However, vocalization data were less reliable due to background noise in the communal environment. The study concludes that wearable sensors hold promise for detecting agitation in dementia patients, suggesting that personalized profiles could enhance detection accuracy. Further research is recommended to refine these technologies for broader application. This study uses
Finally, this paper [48] describes a study in which the effectiveness of measuring the stress levels in people with dementia using a single wristband sensor is explored. Stress is a common issue for individuals with dementia, and it is traditionally assessed through questionnaires completed by a caregiver. This is a time-consuming and subjective process. In this research, a wearable sensor that tracks galvanic skin response (GSR) and movement is assessed in its effectiveness of detecting stress episodes. During the study, the sensor continuously recorded physiological data, which was processed using an online platform to classify the stress levels on a scale from 0 to 5. The goal was to find out if the identified stress episodes by the sensor correlated with those observed by the caregiver. The results showed that there was a strong correlation between the data from the sensor and the caregiver observations. There were, however, strong variations in stress levels among individuals, which highlights the need for personalized stress thresholds. This can improve accuracy in detection. The conclusion of the researchers is that a wristband sensor is a promising tool for monitoring stress. It provides objective, real-time data, which can help caregivers in for example recognizing stress patterns and intervening more effectively.
References
- ↑ ADI - Dementia statistics. (z.d.). ADI - Dementia Statistics. https://www.alzint.org/about/dementia-facts-figures/dementia-statistics/
- ↑ Sharp S. Home from home : a report highlighting opportunities for improving standards of dementia care in care homes.. Alzheimer's Society; 2007.
- ↑ Rebecca Dahms, Cornelia Eicher, Marten Haesner, Ursula Mueller-Werdan, Influence of Music Therapy and Music-Based Interventions on Dementia: A Pilot Study, Journal of Music Therapy, Volume 58, Issue 3, Fall 2021, Pages e12–e36, https://doi.org/10.1093/jmt/thab005
- ↑ Dementia UK. (2025, 21 maart). Coping with distress - Dementia UK. https://www.dementiauk.org/information-and-support/health-advice/coping-with-distress/
- ↑ 5.0 5.1 Soufineyestani, M., Khan, A., & Sufineyestani, M. (2021). Impacts of Music Intervention on Dementia: A Review using Meta-Narrative Method and Agenda for Future Research. Neurology International, 13(1), 1–17. https://doi.org/10.3390/neurolint13010001
- ↑ https://support.garmin.com/en-US/?faq=WT9BmhjacO4ZpxbCc0EKn9
- ↑ 7.0 7.1 Ekra EMR, Dale B. Systematic Use of Song and Music in Dementia Care: Health Care Providers’ Experiences. J Multidiscip Healthc. 2020;13:143-151 https://doi.org/10.2147/JMDH.S231440
- ↑ 8.0 8.1 Ting B, Chen DT, Hsu WT, Liang CS, Malau IA, Li WC, Lee SL, Jingling L, Su KP. Does Music Intervention Improve Anxiety in Dementia Patients? A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J Clin Med. 2023 Aug 24;12(17):5497. doi: 10.3390/jcm12175497. PMID: 37685564; PMCID: PMC10488399.
- ↑ 9.0 9.1 9.2 S. Gedam and S. Paul, "A Review on Mental Stress Detection Using Wearable Sensors and Machine Learning Techniques," in IEEE Access, vol. 9, pp. 84045-84066, 2021, doi: 10.1109/ACCESS.2021.3085502. keywords: {Stress;Heart rate variability;Resonant frequency;Wearable sensors;Heart rate;Skin;Frequency estimation;Mental stress detection;machine learning;physiological signals;wearable sensor;feature extraction},
- ↑ 10.0 10.1 G. Taskasaplidis, D. A. Fotiadis and P. D. Bamidis, "Review of Stress Detection Methods Using Wearable Sensors," in IEEE Access, vol. 12, pp. 38219-38246, 2024, doi: 10.1109/ACCESS.2024.3373010. keywords: {Human factors;Temperature measurement;Stress measurement;Stress;Heart rate;Anxiety disorders;Wearable devices;Detection algorithms;Wearable sensors;Stress analysis;stress detection;stress response;wearable sensors},
- ↑ 11.0 11.1 11.2 Nilsson U. The anxiety- and pain-reducing effects of music interventions: a systematic review. AORN J. 2008 Apr;87(4):780-807. doi: 10.1016/j.aorn.2007.09.013. PMID: 18395022.
- ↑ Laukka, Petri. (2007). Uses of music and psychological well-being among the elderly. Journal of Happiness Studies. 8. 215-241. 10.1007/s10902-006-9024-3.
- ↑ 13.0 13.1 Thoma MV, La Marca R, Brönnimann R, Finkel L, Ehlert U, Nater UM (2013) The Effect of Music on the Human Stress Response. PLoS ONE 8(8): e70156. https://doi.org/10.1371/journal.pone.0070156
- ↑ Rasing, N. L., Janus, S. I. M., Kreutz, G., Sveinsdottir, V., Gold, C., Nater, U. M., & Zuidema, S. U. (2022). The Impact of Music on Stress Biomarkers: Protocol of a Substudy of the Cluster-Randomized Controlled Trial Music Interventions for Dementia and Depression in ELderly Care (MIDDEL). Brain Sciences, 12(4), 485. https://doi.org/10.3390/brainsci12040485
- ↑ 15.0 15.1 Baltazar, Margarida & Västfjäll, Daniel. (2019). Songs perceived as relaxing: Musical features, lyrics, and contributing mechanisms. 10.13140/RG.2.2.29658.82880.
- ↑ 16.0 16.1 16.2 16.3 Wei-Chun Wang; A study of the type and characteristics of relaxing music for college students. Proc. Mtgs. Acoust. 5 May 2014; 21 (1): 035001. https://doi.org/10.1121/1.4902001
- ↑ 17.0 17.1 Science behind – Healthetile. (z.d.). https://healthetile.io/science-behind/
- ↑ Bartolomé-Tomás, A., Sánchez-Reolid, R., Fernández-Sotos, A., Latorre, J. M., & Fernández-Caballero, A. (2020). Arousal Detection in Elderly People from Electrodermal Activity Using Musical Stimuli. Sensors, 20(17), 4788. https://doi.org/10.3390/s20174788
- ↑ Overview — Python EDA Documentation. (z.d.). https://pyeda.readthedocs.io/en/latest/overview.html
- ↑ Aqajari, S. (2021). pyEDA: An Open-Source and Versatile Feature Extraction Python Toolkit for Electrodermal Activity. UC Irvine. ProQuest ID: Aqajari_uci_0030M_17382. Merritt ID: ark:/13030/m57q5w81. Retrieved from https://escholarship.org/uc/item/3xq0084m
- ↑ Aqajari, S. (2021). pyEDA: An Open-Source and Versatile Feature Extraction Python Toolkit for Electrodermal Activity. UC Irvine. ProQuest ID: Aqajari_uci_0030M_17382. Merritt ID: ark:/13030/m57q5w81. Retrieved from https://escholarship.org/uc/item/3xq0084m
- ↑ 22.0 22.1 Ragneskog, H., Asplund, K., Kihlgren, M., & Norberg, A. (2001). Individualized music played for agitated patients with dementia: Analysis of video‐recorded sessions. International Journal of Nursing Practice, 7(3), 146–155. https://doi.org/10.1046/j.1440-172x.2001.00254.x
- ↑ 23.0 23.1 23.2 Peeters, M. W. H., Schouten, G., & Wouters, E. J. M. (2021). Wearables for residents of nursing homes with dementia and challenging behaviour: Values, attitudes, and needs. Gerontechnology, 20(2), 1-13. https://doi.org/10.4017/gt.2021.20.2.7.06
- ↑ Hermann, C., Sperl, M.F.J. (2023). Classical Conditioning. In: Matson, J.L. (eds) Handbook of Clinical Child Psychology. Autism and Child Psychopathology Series. Springer, Cham. https://doi.org/10.1007/978-3-031-24926-6_21
- ↑ Wikipedia contributors. (2024, 21 oktober). Technology readiness level. Wikipedia. https://en.wikipedia.org/wiki/Technology_readiness_level
- ↑ Astell, A. J., Bouranis, N., Hoey, J., Lindauer, A., Mihailidis, A., Nugent, C., & Robillard, J. M. (2019). Technology and Dementia: The Future is Now. Dementia and Geriatric Cognitive Disorders, 47(3), 131–139. https://doi.org/10.1159/000497800
- ↑ Pedersen, S. K. A., Andersen, P. N., Lugo, R. G., Andreassen, M., & Sütterlin, S. (2017). Effects of Music on Agitation in Dementia: A Meta-Analysis. Frontiers in Psychology, 8. https://doi.org/10.3389/fpsyg.2017.00742
- ↑ Baird, Amee & Thompson, William. (2018). The Impact of Music on the Self in Dementia. Journal of Alzheimer’s Disease. 61. 827-841. 10.3233/JAD-170737.
- ↑ Spiro, N. (2010). Music and dementia: Observing effects and searching for underlying theories. Aging & Mental Health, 14(8), 891–899. https://doi.org/10.1080/13607863.2010.519328
- ↑ Gibson, Grant. (2007). Music and the wellbeing of people with dementia. Ageing and Society. 27. 127 - 145. https://doi.org/10.1017/S0144686X06005228.
- ↑ McDermott, O., Orrell, M., & Ridder, H. M. (2014). The importance of music for people with dementia: the perspectives of people with dementia, family carers, staff and music therapists. Aging & Mental Health, 18(6), 706–716. https://doi.org/10.1080/13607863.2013.875124
- ↑ Lam, H. L., Li, W. T. V., Laher, I., & Wong, R. Y. (2020). Effects of Music Therapy on Patients with Dementia—A Systematic Review. Geriatrics, 5(4), 62. https://doi.org/10.3390/geriatrics5040062
- ↑ Thompson, N., Odell-Miller, H., Underwood, B. R., Wolverson, E., & Hsu, M. (2024). How and why music therapy reduces distress and improves well-being in advanced dementia care: a realist review. Nature Mental Health. https://doi.org/10.1038/s44220-024-00342-x
- ↑ Ragneskog, H., & Kihlgren, M. (1997). Music and Other Strategies to Improve the Care of Agitated Patients with Dementia. Scandinavian Journal of Caring Sciences, 11(3), 176–182. https://doi.org/10.1111/j.1471-6712.1997.tb00451.x
- ↑ Vuijk, J. G. J., Brinke, J. K., & Sharma, N. (2023). Utilising Emotion Monitoring for Developing Music Interventions for People with Dementia: A State-of-the-Art Review. Sensors, 23(13), 5834. https://doi.org/10.3390/s23135834
- ↑ Yanan Ding, Kaiwen Tan, Li Sheng, Huiwen Ren, Zhen Su, Hongying Yang, Xin Zhang, Jianyang Li, PingAn Hu (2024). Integrated mental stress smartwatch based on sweat cortisol and HRV sensors. Biosensors and Bioelectronics, Volume 265, 2024, 116691, ISSN 0956-5663. https://doi.org/10.1016/j.bios.2024.116691
- ↑ Siirtola, P. (2019). Continuous stress detection using the sensors of commercial smartwatch. https://doi.org/10.1145/3341162.3344831
- ↑ Chalmers, T., Hickey, B. A., Newton, P., Lin, C., Sibbritt, D., McLachlan, C. S., Clifton-Bligh, R., Morley, J., & Lal, S. (2021). Stress Watch: The use of heart rate and heart rate variability to detect stress: A pilot study using smart watch wearables. Sensors, 22(1), 151. https://doi.org/10.3390/s22010151
- ↑ A review on mental stress detection using wearable sensors and machine learning techniques. (2021). IEEE Journals & Magazine | IEEE Xplore. https://ieeexplore.ieee.org/abstract/document/9445082
- ↑ Alshamrani, M. (2021). An Advanced Stress Detection Approach based on Processing Data from Wearable Wrist Devices. International Journal of Advanced Computer Science and Applications, 12(7). https://doi.org/10.14569/ijacsa.2021.0120745
- ↑ Peeters, M. W. H., Schouten, G., & Wouters, E. J. (2021). Wearables for residents of nursing homes with dementia and challenging behaviour: Values, attitudes, and needs. Gerontechnology, 20(2), 1–13. https://doi.org/10.4017/gt.2021.20.2.7.06
- ↑ Adam, E., Meiland, F., Frielink, N., Meinders, E., Smits, R., Embregts, P., & Smaling, H. (2024). User Requirements and Perceptions of a sensor system for early stress detection in people with dementia and people with intellectual disability: Qualitative study. JMIR Formative Research, 8, e52248. https://doi.org/10.2196/52248
- ↑ Olmedo-Aguirre, J. O., Reyes-Campos, J., Alor-Hernández, G., Machorro-Cano, I., Rodríguez-Mazahua, L., & Sánchez-Cervantes, J. L. (2022). Remote healthcare for elderly people using wearables: a review. Biosensors, 12(2), 73. https://doi.org/10.3390/bios12020073
- ↑ Husebo, B. S., Heintz, H. L., Berge, L. I., Owoyemi, P., Rahman, A. T., & Vahia, I. V. (2020). Sensing technology to monitor behavioral and psychological symptoms and to assess treatment response in people with dementia. A systematic review. Frontiers in Pharmacology, 10. https://doi.org/10.3389/fphar.2019.01699
- ↑ Sharp, B. K. (2017). Stress as Experienced by People with Dementia: An Interpretative Phenomenological Analysis. Dementia, 18(4), 1427–1445. https://doi.org/10.1177/1471301217713877
- ↑ Sung, H., Chang, A. M., & Lee, W. (2010). A preferred music listening intervention to reduce anxiety in older adults with dementia in nursing homes. Journal of Clinical Nursing, 19(7–8), 1056–1064. https://doi.org/10.1111/j.1365-2702.2009.03016.x
- ↑ Nesbitt, C., Gupta, A., Jain, S., Maly, K., & Okhravi, H. R. (2018). Reliability of Wearable Sensors to Detect Agitation in Patients with Dementia (pp. 73–77). https://doi.org/10.1145/3232059.3232067
- ↑ Kikhia, B., Stavropoulos, T., Andreadis, S., Karvonen, N., Kompatsiaris, I., Sävenstedt, S., Pijl, M., & Melander, C. (2016). Utilizing a Wristband Sensor to Measure the Stress Level for People with Dementia. Sensors, 16(12), 1989. https://doi.org/10.3390/s16121989
Appendix
Interviews
Questions for caregivers
The mail was written in Dutch, since that is the language that is used in the care homes that we contacted.
Beste persoonlijke informatie ,
Wij zijn studenten op de Technische Universiteit in Eindhoven. Hiervoor volgen een vak aan de TU/e genaamd Project robots everywhere (0LAUK0) en voor dit project willen wij een prototype ontwikkelen voor mensen met dementie. Het idee is dat wanneer een persoon met dementie onrustig wordt dat er een apparaat is dat muziek afspeelt en zo de patiënt kalmeert. Wij zijn heel erg benieuwd naar de ervaringen van zorgverleners die veel met dementie patiënten te maken hebben. Als u tijd heeft zou er dan een mogelijkheid zijn om deze email naar de zorgmedewerkers te sturen zodat deze de onderstaande vragen kunnen beantwoorden naar hun eigen professionele mening en ervaring? Als jullie er voor openstaan dan zouden wij ook graag hierover willen bellen om hier wat uitgebreider over te hebben.
- Op welke manier werkt u met patiënten met dementie?
- Waar aan merkt u bij een patiënt dat die rusteloos/ geïrriteerd is?
- Op wat voor momenten merkt dat een patiënt rusteloos/ geïrriteerd is?
- Wat zijn uw interventies normaal gesproken wanneer een patiënt gefrustreerd of rusteloos is?
- Wordt er al wel eens muziek afgespeeld bij patiënten (ook als ze rustig zijn)? Zo ja,
- Wat voor effect heeft het?
- Wat voor muziek zou dat dan zijn?
- Heeft verschillende muziek dan ook een ander effect?
- Zou muziek afspelen werken terwijl een patiënt al gefrustreerd is om ze te kalmeren? Of is het beter om al eerder muziek af te spelen wanneer patiënten nog kalm zijn?
- Zou muziek afspelen op momenten dat een patiënt rusteloos/ geïrriteerd is ook een averechts effect kunnen hebben? Zo, ja op welke manier?
- Zou dit prototype ook werken in een groepssetting?
- Zou u een mogelijkheid zien om van ons boven benoemde prototype ook gebruik van maken in de praktijk?
- Zijn er bij z’n soort prototype dingen waar we rekening mee moeten houden waar we nu nog niet aan hebben gedacht?
Alvast heel erg bedankt! Voor vragen of opmerkingen kunt u altijd e-mailen naar: l.v.d.berg@student.tue.nl.
Met vriendelijke Groet,
Lisa van den Berg
The email was send to these emails:
- info@zorgvillaweisshorn.nl
- zorgadvies@vitalisgroep.nl
- info@sintannaklooster.nl
- passaathofvanstrijp@archipelzorggroep.nl
- fleuriade@archipelzorggroep.nl
- eerdbrand@archipelzorggroep.nl
- servicepunt@archipelzorggroep.nl
- familyoffice@domusvaluas.nl
- servicedesk@zorginoktober.nl
- woonzorg@bloezem.nl
- info@elkedageenfijnedag.nl
- contact@pietervanforeest.nl
- info@azora.nl
- IDA@netwerkouderenachterhoek.nl
- info@alzheimer-nederland.nl
- info@tangenborgh.nl
- contact@innoforte-zorg.nl
- adviesteam@pleyade.nl
- info@hetlaar.nl
Responses summarized
· Waar aan merkt u bij een patiënt dat die rusteloos/ geïrriteerd is?
| Reply 1 | Reply 2 | Reply 3 | Reply 4 | Reply 5 |
| Boos kijken | Houding | Lichaamshouding | Kort-af reageren | Stilletjes worden |
| Rusteloos dwalen | Lichaamstaal | Spanning in de spieren/ gezicht | Verdriet | Geïrriteerd |
| Aan deuren trekken | Emotioneel | Onrust in de ogen (paniekblik) | Afsluiten voor je | Boos |
| Weglopen | Boosheid | Loopgedrag | Geen hulp aanvaarden | Blijven lopen |
| Korte antwoorden geven | Teruggetrokken | Wiebelen | Boos gedrag | Geen rust vinden |
| Op zich heen kijken | Loopgedrag | Veel praten | lopen | |
| Plukken | Elke client vertoont zijn eigen tekenen van onrust | Geen rust in het lichaam hebben |
· Op wat voor momenten merkt dat een patiënt rusteloos/ geïrriteerd is?
| Reply 1 | Reply 2 | Reply 3 | Reply 4 | Reply 5 |
| Als de nabije veiligheid weg is | Kunnen heel divers zijn | Als er iets voorgevallen is | Als er net familie/ visite is geweest en deze weer weg gaan. | Verschillende momenten op de dag |
| Tijdens zorgmomenten want dan wordt er van alles gevraagd van een cliënt en dit zorgt voor onrust en irritatie | Als iets anders dan ander is. | Rond 16u in de middag | ||
| Bij de dagbesteding als iemand nieuw is en/of eigenlijk niet wil komen kan er onrust zijn. | Een slechte nacht | Na een activiteit beneden in de gasterij (ontmoetingsruimte/ restaurant) die te veel prikkels hebben gegeven. | ||
| Of als er vooraf iets voorgevallen is, dit kan iets kleins zijn maar ook groot, dit kan aan de persoon zelf liggen in welke fase van dementie dit is of psychische aandoening. | Een cliënt wil gewoon niet op de dagopvang zijn maar thuis. |
· Wat zijn uw interventies normaal gesproken wanneer een patiënt gefrustreerd of rusteloos is?
| Reply 1 | Reply 2 | Reply 3 | Reply 4 | Reply 5 |
| Emotie laten uiten | Achterhalen waar het aan ligt door 1 op 1 gesprek of in de rapportage terug te lezen wat het kan zijn | Afhankelijk van persoonlijkheid van patiënt | Inschatten wat de patiënt nodig heeft soms: praatje, soms knuffel. Soms poosje laten, rust op kamer | Laat de bewoner even |
| Naar buiten gaan | Extra ruimte geven, door apart te zitten of naar eigen kamer brengen | Nabijheid bieden | Onrustmedicatie geven | Veel 1 op 1 contact in rustige omgeving |
| Als je de trigger van boosheid weet, deze weghalen | Zorgen voor afleiding | Uit de situatie halen of ‘meebewegen’ zodat de client het gevoel krijgt weer de regie in handen te hebben | Favoriete CD voor bewoner aanzetten. |
· Wordt er al wel eens muziek afgespeeld bij patiënten (ook als ze rustig zijn)? Zo ja,
| Reply 1 | Reply 2 | Reply 3 | Reply 4 | Reply 5 |
| Ja, heel zachtjes op de achtergrond | Divers muziekaanbod | De meeste mensen krijgen emotie van muziek blij, verdrietig en gaan vaak terug naar het verleden/herinneringen
Als de mensen nog "taal" tot hun beschikking hebben vertellen ze vaak verhalen over vroeger naar aanleiding van muziek. Of lichaamstaal aflezen welke emotie bepaalde muziek bij mensen teweeg brengt |
Bij sommige cliënten helpt dit zeker. Het meeste effect zien wij dan als we de client een koptelefoon op kunnen geven, zodat alle andere geluiden uit de omgeving weg zijn. Toch heb ik het nog niet meegemaakt dat het DE oplossing is. Niet voor een langere periode op een dag. | Muziek zorgt voor ontspanning en genieten van bewoners |
| Afwisseling van muziek want niet iedereen houdt van hetzelfde | Heeft positief effect, maar kan ook emotioneel effect hebben | Mensen die al verder in het dementie proces zijn herkennen muziek die ze vroeger luisterden. Ook reageren deze mensen goed op natuurgeluiden gecombineerd met rustige muziek. Meditatie-muziek, klankschalen, handpan etc | Muziek is verschillend per mens | Verwisselt per bewoner |
| Ook bij onrust muziek opzetten, en dit is niet altijd rustige muziek maar vooral herkenbare muziek want door herkenning worden ze rustig | Klassiek, jaren 50/60, Nederlandstalig, rustgevende muziek of op aanvraag van de cliënt. | Ja bij rustige muziek kunnen mensen ook verdrietig worden of onrustig. Je weet nooit welke herinneringen muziek teweeg brengt, er bestaat geen recept voor een bepaalde reactie, muziek en emotie is zeer persoonsgebonden | Muziek gaat vooral om afleiding. De prikkel moet een positief effect hebben. | Als het de bewoner niet aanstaat dan kan hier ook weer irritatie uit voortkomen. |
| Jazeker, er komen stofjes (oxytocine) vrij in de hersenen en deze zorgen voor een positief effect (geluk stofje). De muziek zorgt voor het stukje samenhorigheid/verbinding, betere motoriek.
Maar kan ook een emotionele kant hebben, bijvoorbeeld als iemand in het verleden iets vervelens meegemaakt heeft en dit wordt dan ook weer teruggehaald, door een bepaald liedje. |
o Wat voor effect heeft het?
o Wat voor muziek zou dat dan zijn?
o Heeft verschillende muziek dan ook een ander effect?
· Zou muziek afspelen werken terwijl een patiënt al gefrustreerd is om ze te kalmeren? Of is het beter om al eerder muziek af te spelen wanneer patiënten nog kalm zijn?
| Reply 1 | Reply 2 | Reply 3 | Reply 4 | Reply 5 |
| Muziek kan helpen maar kan dan ook te vel prikkels geven | Muziek helpt tegen rusteloosheid want het zorgt voor afleiding | Soms wel maar niet altijd want soms zijn de prikkels/ negatieve gedachtes te sterk | Het mooiste zou zijn als je het voor bent, dat je al muziek afspeelt als de bewoner nog kalm is. | |
| Als iemand onderprikkeld is dan helpt muziek juist | Hoeft niet echt daarvoor want rust is ook fijn |
· Zou muziek afspelen op momenten dat een patiënt rusteloos/ geïrriteerd is ook een averechts effect kunnen hebben? Zo, ja op welke manier?
| Reply 1 | Reply 2 | Reply 3 | Reply 4 | Reply 5 |
| Ja en het is echt aftasten. Wat nu werk werkt morgen misschien niet | Ja als het te hard staat of verkeerde muziekkeuze, of al overprikkeld, dan werkt het niet meer | Kan te veel zijn, vooral harde geluiden zijn meestal een trigger | Muziek kan emotie versterken, te veel prikkels, niet bij machte zijn om nee te zeggen waardoor frustratie |
· Zou dit prototype ook werken in een groepssetting?
| Reply 1 | Reply 2 | Reply 3 | Reply 4 | Reply 5 |
| Moeilijk te zeggen vanwege groepsdynamiek maar beter 1 op 1 | Yes | Groepsverband is moeilijk maar als iemand alleen woont en je een sensor zou hebben waarop te zien is dat iemand veel bewegingsdrang heeft dat dan de muziek automatisch aangaat. | Kan als het niet te luid is maar andere bewoners kunnen er wel van schrikken. |
· Zou u een mogelijkheid zien om van ons boven benoemde prototype ook gebruik van maken in de praktijk?
| Reply 1 | Reply 2 | Reply 3 | Reply 4 | Reply 5 |
| Zeker lijkt fijn | Ja is het proberen waard | Ideaal zou zijn een prototype wat zelf onrust kan detecteren, waar muziek uitkomt waar mensen geen herinnering aan hebben maar wel kalmerend werkt. Bv solfeggio frequenties, mantra's , natuurgeluiden. maar ook liedjes die mensen kennen. | Nee meer mogelijkheden waar mensen nog zelfstandig wonen. | 1 bewoner die wisselende stemming heeft, wellicht zou muziek iets voor haar zijn. |
· Zijn er bij z’n soort prototype dingen waar we rekening mee moeten houden waar we nu nog niet aan hebben gedacht?
| Reply 1 | Reply 2 | Reply 3 | Reply 4 | Reply 5 |
| Goed rekening houden met de levensgeschiedenis van de bewoner | Vriendelijke uitstraling | Makkelijk en klein neer te zetten | Volume moet makkelijk te gelen zijn zonder dat we aan bewoner moeten zitten | |
| Tegen vallen/ gooien bestand zijn. | Makkelijk schoon te maken |
Questions for research group
- Have you done any research on the effects of music for dementia patients? If yes,
- What is your role inside this expertise centre?
- What are the challenges you face when designing for dementia patients?
- What are things we should take into account in the design of our prototype?
- What are things we should take into account in the implementation of our prototype?
Mail for research group
Dear {name},
Together with 5 other students I am currently working on a project for the course Project robots everywhere (0LAUK0). We believe your expertise in the field of {field} could elevate our research, and we would love to discuss our idea with you and hear your insight. In this project we are investigating if music can have a calming effect on patients with dementia when they are distressed. We aim to create a design with a wearable stress monitor that automatically turns on specific music when the user is agitated.
If you have time this week or next week and are interested, I would like to sit together with you for 10-15 minutes. Please let me know if you would like to participate and then we can find a date and time that works for both of us!
Kind regards,
Agnes Kiekebeld
Interview Karlijn van Rijen MSc.
The interview was conducted in Dutch, but the questions were prepared before in English. Since the interview was in Dutch the notes taken during and after the interview are also in Dutch.
Interview questions for Karlijn van Rijen MSc.
- What is your role inside this expertise centre?
- I read your paper on RelivRing can you tell me a bit more about this?
- What are some steps you took in designing this device that you would advice us to take into account in the design process?
- In your information blurb on the ECDT website’s team tab, it says that for your PHd you are doing research into the implementation of technology for elderly care, can you tell me a bit more about that? What are important things to take into account (that might be different than designing for other target groups)?
- It also says that you are researching the cooperation between researchers, entrepreneurs and healthcare, could you tell me a bit about some of your findings?
- Have you done any research on the effects of music for dementia patients? If yes,
- What are the challenges you face when designing for dementia patients?
- What are things we should take into account in the design of our prototype?
- What are things we should take into account in the implementation of our prototype?
Notes taken during and after the interview
Humesock meet stress en stressopbouw en visualiseert dit via een sock. Door een vroegtijdige waarschuwing kan je eerder reageren en escalatie voorkomen. Misschien goed als we kijken of we kunnen vinden wat voor soort algoritmes deze gebruikt. https://mentechinnovation.eu/hume/
Misschien handig om Joyce Westerink te contacteren of naar haar onderzoek te kijken want zij werkt in de HTI group en werkt veel met psychophysiology in producten en applications. Haar research focust op general wellbeing (mental balance, eudemonia, stress, happiness, arousal) en hoe dat is reflected in physiology en how unobtrusively measure that. https://www.tue.nl/en/research/researchers/joyce-westerink
Ze vertelde ook dat het belangrijk is om mee te nemen of iets pacifier technology is, en dat je dus moet kijken naar de ethische risicos en z’n device niet moet aanzetten als een quick fix want dat zorgt voor onmenselijkheid.
Het is misschien ook goed om ipv naar muziek te kijken naar ambiend sounds (dus ook andere content aanbieden) want die zijn ook veel belovend. (Maarten Houben onderzoek, al gemaild maar nog geen reactie)
De vorm van je device is ook heel belangrijk want zulk soort dingen zijn snel stigmatiserend en zitten niet lekker. Evt, kijken dus naar die sokken of iets van die tracker ringen vertelde ze. Mensen met dementie doen al deze dingen vaak heel snel af. Goed om specifiek te kijken naar fitbits en mensen met dementie was haar advies want ze dacht dat daar ook veel onderzoek naar was gedaan. En hoe zorg je dat mensen dit product in huis willen hebben.
Fitbit werkt niet goed, maar bijv. traditioneel horloge wel meer, enerzijds mooi zijn en anderzijds praktisch dat ze er wel iets mee kunnen.
Goradio is iets waar we naar kunnen kijken want dat is ene ouderwetse radio voor mensen met dementie die je met 1 knop kan aanzetten. Gemaakt door olaf mastenbroek. Ze zei dat we hem een mail konden sturen met dat we zijn gegevens via ECDT hebben. olaf@stichtinggoradio.nl
Marjolijn wintermans is ook goed om literatuur van te lezen, haar onderzoeksperspectief is muziek afspelen dat mensen op hun gemak stelt.
Zij werkt daar via luct, dat is een adviesbureau, soort van als team coordinator over bijv. hoe trekken we funcing aan en welke kant gaan we op met ECDT en ze doet een phd.
Slim om als je echt met mensen in de zorg onderzoek wil doen, zoals dementie patiënten dat je zorgt dat je wat terug doet voor zorgtehuizen, dan willen ze sneller mee werken. Dus maak er een leuke dag van bijv.
Goed om te weten wat ons product als belang is in de realiteit, moeten we goed in beeld brengen. TRL zijn technological readiness levels over hoe ver je bent met je product en wat voor stappen je hiervoor moet ondernemen. Misschien wel slim om dat uit te werken om te kunnen laten zien. Stappen zijn bijv ook zo snel mogelijk funders aantrekken en nwo subsidies, hierna investeerders. Zorg ook dat we goed in beeld hebben wie onze eingebruikers zijn. Kinderen betalen vaak voor zulk soort producten of verzekeraars. Voor wie is het, markt of zorg. Maak dit van te voren duidelijk. Denk aan dat sommige dingen te duur zijn zoals robots die rond het huis lopen maar die wel daarvoor eigenlijk bedoeld zijn.
Hoe zie je dit business model voor je? Aan welke kanalen ga je het verkopen? Is allemaal goed om duidelijk te hebben in je design process.
Approach
Start by ature study. We want to make/ build a prototype and then interview healthcare workers on their opinions on our idea.doing a liter
| Week 1 | Week 2 | Week 3 | Week 4 | Week 5 | Week 6 | Week 7 | Week 8 |
|---|---|---|---|---|---|---|---|
| 13/02 Mail with topic and group | Start looking for interviewees | Set up interview schedule | Research all components necessary for a working product | Make a plan on how to integrate the components of our product into a working device. | Interpret results from the | Design an Inteface of app | Complete Wiki page |
| Set up project | Research possibilities for prototype design | Gather parts necessary for prototype | Conduct interviews and send surveys | Conduct interviews and send surveys | Research how data is being analyzed by chosen monitoring device | Prepare presentation | |
| Search and summarize 25 research papers | Literature Research about types of stress measurement | Literature Research about dementia, stress and music | Literature research about what types of music to use | Design visualization of the workings of our device. | Presentation | ||
| Work on Problem statement, Objectives, Users, approach, Milestones, Deliverables,
and Planning |
*rough estimate in planning
Milestones
What are the big checkpoints, so how long will we be working on each section e.g.
Week 1:
- Finish Problem statement, Objectives, Users, approach, Milestones, Deliverables, and Planning sections
- Finish State of the art section
Week 2:
- Finish making sketches
- Finalise the prototype design
Week 4:
- Finalise Informed consent form
- Finalise interview schedule
Week 5:
- Finalise the idea of our product and receive feedback
Week 6:
- Receive all data from the interviews
Week 7:
- Give final presentation
Deliverables
What we will be handing in (so are we making a prototype, literature study, etc.)
- Complete concept of the workings of our product and it's parts
- Result of the interviews
- Report about the project in this Wiki
Logbook
| Week | Task | Hours |
|---|---|---|
| 1 | Brainstorm | 1 |
| Search literature studies | 2 | |
| Summarize literature studies | 5 | |
| Problem statement | 1 | |
| Approach, Milestones, and Deliverables | 2 | |
| Total | 11 | |
| 2 | Do research about design of prototype | 3 |
| Meeting Monday | 1 | |
| Prototype meeting Thursday | 1 | |
| Meeting Friday | 1 | |
| Find components for prototype | 2 | |
| Total | 8 | |
| 3 | Meeting Monday | 1 |
| Brainstorm design | 4 | |
| Research about Bluetooth connections | 2 | |
| Total | 7 | |
| 4 | Meeting Monday | 1 |
| Write design requirements | 2 | |
| Total | ||
| 5 | Meeting Monday | 1 |
| Research stress monitor devices | 3 | |
| Write design proposal | 2 | |
| Actors section | 2 | |
| Total | 8 | |
| 6 | Meeting Monday | 1 |
| Write Testing possibilities | 2 | |
| Make app designs | 2 | |
| Total | 4 | |
| 7 | Meeting Monday | 1 |
| Finish design proposal | 2 | |
| Finish Actors | 2 | |
| Presentations | 3 | |
| Total | 8 |
| Week | Task | Hours |
|---|---|---|
| 1 | Brainstorm | 1 |
| Search literature studies | 1.5 | |
| Summarize literature studies | 5.5 | |
| Users (and their requirements) | 2 | |
| Total | 10 | |
| 2 | Meeting monday | 1 |
| Research about stress sensors | 3 | |
| Summarizing findings | 3 | |
| Meeting friday | 1 | |
| Total | 8 | |
| 3 | Meeting monday | 1 |
| Research about dementia and music | 3 | |
| Researching when to play music | 2 | |
| Research about the stages of dementia | 3 | |
| Summarizing findings | 3 | |
| Total | 12 | |
| 4 | Meeting monday | 1 |
| Research about relaxing music | 4 | |
| Summarizing findings | 3 | |
| Meeting friday | 1 | |
| Total | 9 | |
| 5 | Meeting monday | 1 |
| More research on characteristics of relaxing music | 4 | |
| Research effects of music in brain dementia patient | 4 | |
| Summarizing findings | 2 | |
| Meeting friday | 1 | |
| Total | 12 | |
| 6 | Meeting monday | 2 |
| Research about We-Be band | 4 | |
| Research about how physiological data is analyzed | 4 | |
| Summarizing findings | 3 | |
| Working on explaining limitations of our project | 4 | |
| Meeting friday | 1 | |
| Total | 18 | |
| 7 | Meeting monday | 1 |
| Research about specific target users | 2 | |
| Cleaning up Wiki | 2 | |
| Write text for presentation | 3 | |
| Prepare for presentation | 4 |
| Week | Task | Hours |
|---|---|---|
| 1 | Brainstorm | 1 |
| Setting up the wiki page | 2 | |
| Search literature studies | 2 | |
| Summarize literature studies | 3 | |
| Objectives | 2 | |
| Total | 10 | |
| 2 | Meeting monday | 1 |
| Prototype meeting thursday | 1 | |
| Prototype research | 4 | |
| Meeting friday | 1 | |
| Brainstorm after meeting | 1 | |
| Finish summarizing (not yet finished) | 4 | |
| Total | 12 | |
| 3 | Meeting monday | 2 |
| Research wearables | 4 | |
| Brainstorm prototype | 3 | |
| Meeting friday | 2 | |
| Total | 11 | |
| 4 | Meeting monday | 1 |
| Research group settings | 4 | |
| Set up mailing list (with Lisa) | 3 | |
| Finalize emails | 2 | |
| Meeting friday | 2 | |
| Total | 12 | |
| 5 | Meeting monday | 2 |
| Brainstorm new setup | 2 | |
| Research limitations | 4 | |
| Meeting friday | 1 | |
| Total | 9 | |
| 6 | Meeting monday | 1 |
| Write limitations | 3 | |
| Clean up wiki | 2.5 | |
| Meeting friday | 1 | |
| (I was sick this week) | ||
| Total | 7.5 | |
| 7 | Meeting monday | 1 |
| Make visualizations | 3 | |
| Meeting wednesday | 3 | |
| Presentations and prep meeting | 4 | |
| Evaluation | 2 | |
| Total | 13 |
| Week | Task | Hours |
|---|---|---|
| 1 | Brainstorm | 1 |
| Planning | 2 | |
| Search literature | 3 | |
| Total | 6 | |
| 2 | meeting monday | 2 |
| Summarize literature | 3 | |
| meeting friday | 1 | |
| Research sensors | 3 | |
| Total | 9 | |
| 3 | Meeting Monday | 2 |
| Summarize research | 3 | |
| Meeting Friday | 1 | |
| Heart rate variability research | 3 | |
| Total | 9 | |
| 4 | Meeting Monday | 1 |
| Set up mailing list (with agnes) | 3 | |
| Research Dementia & Technology centre | 3 | |
| Set up interview questions | 2 | |
| Send emails | 2 | |
| Meeting Friday | 2 | |
| Total | 13 | |
| 5 | Meeting Monday | 3 |
| Research Karlijn van Rijen | 3 | |
| Interview Karlijn van Rijen | 3 | |
| Write notes on interview | 1 | |
| Send more emails | 1 | |
| Look into information gathered from interview | 3 | |
| Meeting Friday | 1 | |
| Total | 15 | |
| 6 | Meeting Monday | 1 |
| Summarize Interviews with healthcare workers | 6 | |
| Limitations | 2 | |
| Meeting Friday | 1 | |
| Total | 10 | |
| 7 | Meeting monday | 1 |
| Meeting Wednesday | 2 | |
| Make & prepare presentation | 5 | |
| Meeting Thursday (also before presentations) | 5 | |
| Total | 13 |
| Week | Task | Hours |
|---|---|---|
| 1 | Brainstorm | 1 |
| Search literature | 2.5 | |
| Summarize literature | 6 | |
| Total | 9.5 | |
| 2 | Meeting Monday | 1 |
| Research prototype | 4 | |
| Summarize findings | 3 | |
| Meeting Friday | 1 | |
| Brainstorm after meeting | 1 | |
| Total | 10 | |
| 3 | Meeting Monday | 1 |
| Brainstorm design | 4 | |
| Clean up the wiki | 2.5 | |
| Meeting Friday | 1 | |
| Total | 8.5 | |
| 4 | Meeting Monday | 1 |
| Update approach, milestones and deliverables | 3 | |
| Clean up wiki | 4 | |
| Meeting Friday | 1 | |
| Total | 9 | |
| 5 | Meeting Monday | 1 |
| Restructure Wiki | 3 | |
| Rewrite problem statement | 1 | |
| Help with design proposal | 2 | |
| Start on cleaning up state of the art | 2 | |
| Meeting Friday | 1 | |
| Total | 10 | |
| 6 | Meeting Monday | 1 |
| Clean up state of the art | 5 | |
| Find new articles for state of the art | 3 | |
| Summarize new articles | 2 | |
| Meeting Friday | 1 | |
| Total | 12 | |
| 7 | Meeting Monday | 1 |
| Prepare presentation | 4 | |
| Practice presentation | 2 | |
| Presentations | 3 | |
| Total | 10 |