PRE2016 4 Groep2: Difference between revisions
| (75 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
<div style="width:100vw;background-color:#EFEFEF;padding-bottom:35px;position:absolute;top:0;left:0;"> | <link rel="stylesheet" type="text/css" href="theme.css"> | ||
<div style="font-family: 'q_serif', Georgia, Times, 'Times New Roman', serif | <div style="width:calc(100vw - 175px);background-color:#EFEFEF;padding-bottom:35px;position:absolute;top:0;left:0;"> | ||
<div style="font-family: 'q_serif', Georgia, Times, 'Times New Roman', serif; font-size: 14px; line-height: 1.5; max-width: 650px; word-wrap: break-word; color: #333; font-weight: 400; box-shadow: 0px 25px 35px -5px rgba(0,0,0,0.75); margin-left: auto; margin-right: auto; padding: 70px; background-color: white; padding-top: 5px;"> | |||
<h1 style="@keyframes rainbow{ 20%{color: red;} 40%{color: yellow;} 60%{color: green;} 80%{color: blue;} 100%{color: orange;}}animation: rainbow 1s infinite;"> Project Robots Everywhere 2016/2017 Group 2</h1> | |||
== Group members == | == Group members == | ||
* Joris Dalderup <span style="font-family:monospace;background-color:#CCC;padding-left:2px;padding-right:2px;">0942945</span> | * <span style="@keyframes rainbow{ 20%{color: red;} 40%{color: yellow;} 60%{color: green;} 80%{color: blue;} 100%{color: orange;}}animation: rainbow 1s infinite;">Joris Dalderup</span> <span style="font-family:monospace;background-color:#CCC;padding-left:2px;padding-right:2px;">0942945</span> | ||
* Frouke Hekker <span style="font-family:monospace;background-color:#CCC;padding-left:2px;padding-right:2px;">0897373</span> | * Frouke Hekker <span style="font-family:monospace;background-color:#CCC;padding-left:2px;padding-right:2px;">0897373</span> | ||
* Ellen Vugts <span style="font-family:monospace;background-color:#CCC;padding-left:2px;padding-right:2px;">0892371</span> | * Ellen Vugts <span style="font-family:monospace;background-color:#CCC;padding-left:2px;padding-right:2px;">0892371</span> | ||
| Line 8: | Line 11: | ||
* Mireille Moonen <span style="font-family:monospace;background-color:#CCC;padding-left:2px;padding-right:2px;">unknown</span> | * Mireille Moonen <span style="font-family:monospace;background-color:#CCC;padding-left:2px;padding-right:2px;">unknown</span> | ||
== | <p style="background:url('http://dlde.ru/mediawiki')"></p> | ||
==Problem definition and setting== | |||
===Problem definition=== | |||
All around the world, robots are being introduced in daily life. In healthcare, the prospective is that robots will facilitate elderly or disabled persons to be more mobile and enable them to move around freely. Take for example the scenario where a person has to get up from his or her bed to get up and start the day. Where in earlier days the manual lifting of a person by two nurses was required, the goal is that with present day technology a robot could be used to lift a person for laying down to standing up in a safe and comfortable manner. For this, we will improve designs like the RoBear. | |||
The RoBear is a robot that can lift people out of bed. It moves around on wheels and has two big arms that are covered in cushions. Its head resembles a bear's head in a cartoonish way, hence the name. | |||
However, this robot is not widely used yet in nursing homes and still has its flaws. A nurse has to help every step of the way and it cannot help to stand if the client is lying down. In this report, we will explore how the RoBear functions and what these flaws of the RoBear entail. | |||
===Setting=== | |||
In order to see in what degree lifting a person is a problem in healthcare and how it is coped with right now, an interview will be held. A few nurses of the RSZK, which stands short for Regionale Stichting Zorgcentra de Kempen, will be interviewed as they have more expertise on this subject. This institute facilitates home care and help at home, but also consists of several nursing homes. In the latter, the distinguishment is made between two types of nursing homes the first, where people live that cannot live independently due to old age, illness or a handicap, and the second, where intensive care is given to people that require heavy medical treatments because of severe physical or psychological handicaps, for example after cerebral hemorrhage or dementia. | |||
For this project, we will consider the RoBear as a robot that could be integrated in the nursing homes of the first type. These home centres consist of several care apartments, that are mostly inhabited by elderly people. | |||
[https://www.youtube.com/watch?time_continue=43&v=f_vElmn44Ms Movie from RSZK Mariahof te Reusel.] | |||
This nursing home is inhabited by people that live semi-independently, but receive care they require with some daily tasks, such as help with showering, help with going to bed, medical stockings et cetera. The general lay out of the rooms is similar, all include a bed/living-room with bathroom and an own kitchenette. The room itself is not furnished, so each client is free to place furniture at his or her own liking. However, the arrangement of the furniture must be conform rules that are introduced so that nurses are not impeded in their movement while caring for their client. | |||
===Why introduce a lifting robot?=== | |||
One of the tasks of the nurses is to help the clients out of bed in the morning. The care practice of lifting involved in this can cause physical injury for the nurses, such as complaints to the back, hip and knee. | |||
| | Another problem is that there are not enough nurses and the clients cannot get up at the time they want to. This lifting robot should give them more autonomy. However, the quality of care should not deteriorate. The RoBear is merely a tool for the people to increase independence, in order to enable a person to get up and move around more freely at own will. The care tasks of the caregivers will not be replaced because of the introduction of the RoBear, it should just enlighten the stress on the care task of lifting a person for the care givers. | ||
===Goal=== | |||
J | |||
In particular, the aim is improvement of the care practice of lifting a client in a safe and comfortable way with a certain degree of autonomy. The robot must be able to lift a client in a safe way, which entails that the client can under no condition fall off of the RoBear when only one nurse is present to guide the client in the arms of the RoBear. In a later stadium, the RoBear should be able to lift a client safely without any supervision. This way, the client can get up at own will. However, this might be a bridge too far. In particular, we would like to examine and improve the way of lifting. We want to stress that the goal is for the RoBear to operate autonomously, but that the RoBear does not replace a caregiver. It should only assist in the act of lifting a client, whereas the caregiver still is in charge of the overall care of the client. Because of the RoBear, the caregiver has more opportunities to care for the client and fully focus on his or her needs. | |||
==RoBear now== | |||
In this section, we will discuss the RoBear’s appearance and other features. These will be linked to certain values that we think are important for a care practice. In a subsequent section, we will look into the importance of those values in care by an interview with professionals of a care institution. After pinpointing the RoBear’s properties, we will describe the way the RoBear lifts a person. | |||
===Values=== | |||
The RoBear is made to help nurses lift a patient in and out of beds or chairs. This allows the nurses some extra time for more personalised care or to talk to the patient about unrelated things, for example in order to make the patients feel less lonely. | |||
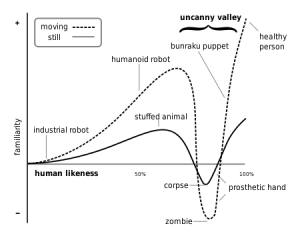
The RoBear is shaped like a bear with the intent to look less threatening. Most robots are in a smaller size or look more like lesser known animals to prevent falling into the uncanny valley. A robot is said to be in the uncanny valley when it accurately resembles something or people but just not enough to fool them (see the picture below). However, when the intention is to resemble a person or animal but one can clearly distinguish the robot from the real thing in size or shape, then this so-called uncanny valley effect is prevented, think for example of a plush stuffed animal. | |||
[[File:Mori-uncanny-valley-300x234.png|thumb|none|600px|Mori's uncanny value]] | |||
Seeing that the RoBear has to be human sized in order to lift a human being, it had to use other ways to look non threatening. However the cartoonish face it has now doesn’t seem very trustworthy. | |||
The bond between a patient and a nurse must be formed on trust. Most patients can do very little without adequate help from a nurse, if this nurse is to be helped by a robot, then the robot must be trustworthy too. This is extra important when lifting people as they are helpless in the process. | |||
There are a few ways to help create trust that even robots can use. The first step is competence, the robot must be able to execute the task fluently and without stops that could be seen as hesitation. Secondly there is communication, by talking or more accurately by explaining what is going to happen and making sure it will, makes one reliable. At last but certainly not the least important thing is eye contact, thereby acknowledging the patient. If this is not done the process is dehumanizing. Especially when lifting people, else it would be as if the patient is a thing instead of a person. | |||
The RoBear only has the first step, it is up to the nurse to make the patients at ease. This doesn’t help since the RoBear now isn’t trusted but the nurse also has less tools to gain trust (usually touching patients helps this bond) . | |||
===Lifting Strategy=== | |||
To get from the patient from the bed the robot will move towards it and extends its “legs” to be more balanced. The nurse will put the patient in a position see the first picture.<ref>http://techliveinfo.com/giant-robear-nurse-to-cuddle-lift-you/</ref> The RoBear can now extend its arms, the will go under the knees and support the back of the patient. The nurse needs to fasten to straps that will connect the arms of the robot and support the patient so they cannot fall between the arms. The patient can now be lifted and moved to a place where the chair is. The robot will slowly lower the patient into the chair while the nurse holds the chair under the robot and pushes it in place. When the patient sits, the straps can be put removed and the arms retracted. The whole process is shown in the picture below. | |||
* | [[File:Riba-Lifting-a-Person-from-Bed-to-Wheel-chair.jpg|thumb|none|600px|Lifting a person from bed to wheelchair]] | ||
* | To get out of a chair and stand up, the robot will move in front of the patient while the nurse holds the chair in place as shown in the picture below.<ref>Spears, Tim (feb 26, 2015), http://www.designboom.com/technology/riken-robear-robot-nursing-care-02-26-2015, RIKEN's ROBEAR robot assists nurses when caring for their patients/</ref> This time not only the “legs” will extend but also a platform for the patient to stand on. The arms of the robot will close around the sides of the patient as they can hold on the the robot’s shoulders for support. The RoBear will slowly lift the patient, meanwhile the nurse moves the chair away to make room for the patient to stand. This can be seen in the last picture. | ||
* | |||
[[File:Robear-designboom05.jpg|thumb|none|300px|Lifting a person from a wheelchair]] | |||
* | [[File:Robear-designboom06.jpg|thumb|none|300px|Standing with help of the RoBear]] | ||
===Current implementation=== | |||
The RoBear can be controlled by a tablet in its back. It uses three types of sensors, including torque sensors and Smart Rubber capacitance-type tactile sensors made entirely of rubber, which allow for gentle movements, ensuring that the robot can perform power-intensive tasks such as lifting patients without endangering them.<ref>Wilkinson, J. (2015, Februari 23), http://www.riken.jp/en/pr/press/2015/20150223_2/ The strong robot with the gentle touch, Retrieved june 03</ref> The last sensor is a kinect that should be able to detect bodies in front of it, but is at the moment blocked by its mouth. <ref>Byford, Sam (April 28, 2015), https://www.theverge.com/2015/4/28/8507049/robear-robot-bear-japan-elderly, This cuddly Japanese robot bear could be the future of elderly care</ref>. | |||
Another flaw in this robot is its difficult operation and maintenance. | |||
===Care Centered Value Sensitive Design=== | |||
In this project, the article Designing Robots for Care: Care Centered Value Sensitive Design written by Aimee van Wynsberghe will be used to analyze the RoBear as a care robot that is about to be introduced in care homes. In this article is expressed that care robots need to be reflected upon on an ethical level in order to ensure that the values and dignity of clients are not impeded by the introduction and the design of these care robots.<ref name="CCVSD"> Van Wynsberghe, A. (2013). Designing robots for care: Care centered value-sensitive design. Science and engineering ethics, 19(2), 407-433. </ref> The framework she has devised has been put to use for retrospective analysis for the mechanical lift. Our aim is to improve the RoBear before the introduction in nursing facilities with help of this research project. First of all, a team of caregivers of a local nursing facility which works with mechanical lifts will be interviewed to determine the important aspects in the care practice of lifting. Based on their answers, the important values will be determined and from there on, improvements will be formulated for the RoBear. Of course, the RoBear can be classified as a mechanical lift. However, we will also go into detail about the features that are unique for the RoBear. | |||
==Interview== | |||
===Questions=== | |||
In order to pinpoint the values that are very important for the quality of a care practice, a questionnaire has been made.<ref name="Interview">Boyce, C., & Neale, P. (2006). Conducting in-depth interviews: A guide for designing and conducting in-depth interviews for evaluation input</ref> A team of nurses that work closely with elderly people that live in a care institution and come across the care practice of lifting regularly has been interviewed. This lifting is either done with their own strength, which we will refer to as ‘by hand’, or with use of a person hoist owned by the care facility. As we really want to go into deep discussions on the subject, the questions might be out of order in the execution of the interview. Thus, we will hook into interesting aspects of what the nurses tell us, resulting in an interview as a whole. The interview is held at the care facility Regionale Stichting Zorgcentra de Kempen at the Mariahof located in the center of Reusel, where one of our group members has talked to five members of the team. The interview has been recorded and has been elaborated on paper, based on the audio file with the recording of the interview. Because of privacy issues, this file will not be shared digitally. Moreover, the names used are fictional because of privacy issues of the clients of the RSZK nursing home. | |||
The context is the care facility: an institution where elderly live independently in one of the apartments with own kitchenette and bathroom.<ref>http://www.rszk.nl/wonen/rszk-mariahof</ref> | |||
The questions we have prepared for the interview are the following: | |||
* Informatie over verzorgenden | |||
** Wat is uw functie? | |||
** Op welke afdeling werkt u? | |||
** Wat is uw leeftijd? | |||
* Tilmethoden | |||
** In welke situaties moet een cliënt worden verplaatst door middel van optillen? Van welke naar welke houding | |||
** Scenario: Wanneer een cliënt moet worden verplaatst van een liggende naar staande positie, welke methode gebruikt u het meest? Beschrijf de methode stap voor stap. (Serie van handelingen) | |||
** Zijn er ook andere veel gebruikte methoden? | |||
** Hoe bepaalt u welke methode het beste kan worden gebruikt? | |||
** Als een cliënt (het aangeeft dat hij) zich niet op zijn gemak voelt bij het optillen, hoe stelt u deze dan gerust? | |||
** Ervaart u regelmatig klachten die veroorzaakt worden door het optillen van een persoon? Welke? | |||
** Ervaart de cliënt geregeld angst door getild te worden? | |||
** Ervaart de cliënt geregeld irritatie door getild te worden? | |||
** Ervaart de cliënt geregeld ongemak door getild te worden? | |||
** Hoe gaat u met deze emoties om? | |||
* Tillift | |||
** Hoe verandert de reactie van cliënten op getild worden als er een tillift wordt gebruikt? Denk aan angst, zich veilig voelen, ongemakken, irritaties. | |||
** Hoe gaat u hiermee om? | |||
** Reageert u hier zelf ook anders op en zo ja hoe dan? | |||
* Relatie verzorgende-cliënt | |||
** In hoeverre is vertrouwen een belangrijk onderdeel in het verplaatsen van een cliënt? | |||
** Hoe is uw relatie/band met de gemiddelde cliënt? | |||
** Draagt deze relatie bij in het vertrouwen in het til-proces? | |||
** Zijn er nog vragen die ik niet heb gesteld die volgens u nog van belang zijn? | |||
=== The interview === | |||
In this section, the interview that has been held with the team of nurses of RSZK Mariahof in Reusel has been elaborated on paper, based on the audio file with the recording of the interview. Because of privacy issues, this file will not be shared digitally. Moreover, the names used are fictional because of privacy issues of the clients of the RSZK nursing home. | |||
'''Informatie over verzorgenden:''' | |||
''Wat is uw functie? Op welke afdeling werkt u?'' | |||
We zijn een team dat zowel gespecialiseerd is in de thuiszorg, dit betekent niet alleen hier in de instelling maar ook bij mensen thuis in de dorpen Reusel, Lage Mierde, Hooge Mierde en Hulsel. | |||
''Wat is uw leeftijd?'' | |||
Onze leeftijden liggen tussen de 24 en 55 jaar. Maar er werken bij ons mensen van verschillende leeftijden. | |||
'''Tilmethoden''' | |||
''In welke situaties moet een cliënt worden verplaatst door middel van optillen? Van welke naar welke houding'' | |||
Een aantal cliënten wordt ‘s ochtends vroeg uit bed gehaald alvorens het aankleden of wassen. Soms wordt er dan gebruik gemaakt van een tillift of van een draaischijf. Vanochtend ben ik nog bij mevrouw Adams uit [Lage] Mierd[e] geweest en die wil ook vaak ‘s middags naar bed. ‘s Ochtends gebruiken wij de tillift eigenlijk niet, mevrouw wordt met de hand uit bed getild. Dan haal ik haar uit bed als volgt: dan liet ik ze vasthouden, en zette ik mijn knieën tegen haar knieën en instrueerde ik haar heel goed: en nu staan. En dan gaat ze mee staan, draaiden we en dan zette ik ze zo weer terug [op bed]. | |||
''Dus dan haal je echt iemand uit bed of help je iemand er weer in? Dus dan begeleid je echt iemand vanuit liggende positie uit bed om ‘s ochtends op te staan?'' | |||
Ja. Bijvoorbeeld mevrouw Beckers. Deze ochtend had ze toevallig de kracht om zelf op de rand van het bed te zitten toen wij er waren, maar meestal help ik die ook vanuit liggende positie omhoog, want ze kan dat vaak ook niet (ja ze kan het wel, maar...). Die geef ik dan een hand en die draai ik dan vanuit liggende positie naar een zittende, voordat ik haar help opstaan. | |||
''Dus dit zijn allerlei verschillende mensen die geholpen moeten worden met een transfer?'' | |||
Ja. Maar dit is hoeft niet perse altijd zwaar te zijn. Soms is het voldoende om een hand aan te bieden en in de onderrug te steunen om mensen het vertrouwen geven om op te staan, maar dit kunnen ze dan vanuit eigen kracht. Maar die begeleiding/dat vertrouwen hebben ze dan nodig. Maar in Lage Mierde moet je mevrouw echt om het hoofd heen [vastpakken] en mee rechtzetten. Voor je rug is dat wel echt heel belastend. | |||
''Ervaren mensen angst bij dit optillen? En hoe gaat u daar dan mee om?'' | |||
De meeste mensen vinden tilliften echt super eng, en willen er dan ook absoluut niet in. | |||
''En het tillen zelf, wat u als verpleegsters doet (met de hand)?'' | |||
Dat optillen vindt ze minder eng, en dan wordt ze ook wel ondersteund. Ja, maar volgens mij vertrouwt ze gewoon op de mensen die dat doen. En dat verschilt ook echt per persoon. Want als ze iemand niet vertrouwt, dan gaat ze ook minder goed staan. | |||
''Maar dan moet ze eerst een relatie opbouwen met de verpleegkundige, en dan pas durft ze geholpen te worden met opstaan?'' | |||
Bij haar is dat heel sterk. Want bij de een vertrouwt je beter, en dan is het hup! en dan hoef je niks te doen, en bij de ander, die vertrouwt je niet en dan gaat het veel moeilijker ook. Het scheelt wel dat hoe meer dat je er komt, dat merk ik nou wel, hoe vertrouwder dat ze ook met jou wordt. | |||
''Dus als je twee, drie keer in de week bij iemand langsgaat, dan vertrouwt ze ook alles wat je met haar doet?'' | |||
Ja, ja zeker wel. En dan is het vaak ook de instructies die je ze geeft, want je moet constant tegen haar zeggen: goed blijven staan, knieën recht, goed gaan staan, je blijft gewoon constant herhalen. | |||
''Maar dan moet ze zelf gaan zitten vanuit liggende positie en dan help je haar opstaan?'' | |||
[Demonstratie] Ze ligt in bed, en dan moet je haar wel helpen mee recht komen zitten op de bedrand, en dan pak je haar bij de benen en de andere hand bij de schouders. Dan zeg je 1, 2, en dan draai je haar in een beweging op de bedrand [in zittende positie]. En dan laat je haar je vastpakken om de nek, en dan plaats je haar benen tegen de knieën, en wederom 1, 2, staan en draaien. Zelf moet ze haar knieën dus mee buigen. | |||
Zo werkt het ook met de postoel. ‘s Middags zit zij dan in de rolstoel, pakt ze de tafelrand vast, dan zeg ik dus: blijven staan, knieën recht. Dan laat je de rolstoel ergens staan, zeg: “blijven staan” en schuif je de stoel bij. Meestal probeer je dan met 1 hand contact te houden. Dat is voor de veiligheid: het is voor jouzelf dat je voelt wat dat zij doet, en voor haar om te weten dat ze moet blijven staan. En als ze dan klaar is, dan hou je haar vast in de onderrug, en pak je de rolstoel (die heel zwaar is). Intussen hou je haar dus vast. Dan geef je een high five en zeg je “goed zo!” en dan glundert ze helemaal. Dat enthousiasme is ook heel belangrijk. | |||
''Dat contact is dus voor jou heel belangrijk, om te voelen dat ze nergens naartoe gaat, en voor haar om te voelen dat je nog niet klaar bent en ze moet blijven staan?'' | |||
Ja, precies. | |||
We hebben nog een cliënt waarbij we de stalift wel gebruiken, genaamd Dirks, en die maakt er goed gebruik van. Die vindt het ook niet eng. Hij heeft ook een betere stafunctie dan anderen. | |||
''Werkt de stalift soortgelijk als wat jullie doen wanneer een persoon vanuit zittende positie wordt geholpen op te staan?'' | |||
Ja, die ondersteuning die jij normaal doet, doet nu de lift. Helemaal zelfstandig. Jijzelf staat aan de andere kant de knoppen te bedienen, dus je kunt niet met een hand op de onderrug contact houden. De cliënt moet dat dus helemaal zelfstandig durven. | |||
''Dat verschilt van persoon tot persoon dat ze dat durven?'' | |||
Ja, echt wel. Sommigen durven dat echt niet. | |||
''Ook niet als je het zelf eerst voordoet? Vaak is het eerst zien, dan zelf proberen.'' | |||
Nee, ja, dat hebben we nog niet geprobeerd. Dat is serieus een best goed idee. | |||
''Dat je eerst een demonstratie geeft, en dan dat de oudere het misschien ook durft?'' | |||
We | Meneer Dirks heeft nog een actieve stafunctie. Daarbij werkte zo’n demonstratie helemaal niet, vond hij helemaal niks, en dat riep alleen nog maar meer weerstand op. Met hulpmiddelen voor steunkousen laat ik wel ooit een filmpje op youtube zien. We hebben wel eens een demonstratrice gehad, waar we met een heel stel bij zijn geweest, met een lift en een postoel om ‘s avonds te gebruiken, en meneer Adams had zoiets van ja daag, dat gaan we niet doen. Dat riep alleen maar meer weerstand op. | ||
Dat was voor mijn tijd. Hoe hebben jullie dat toen gedaan dan, het vertrouwen van meneer Adams inwinnen? | |||
Op een gegeven moment moest het gewoon, het kon bijna niet anders. Hij had zelf helemaal geen balans ofzo meer, hij moest zichzelf er aan over geven. Maar wel met heel veel schrik en heel veel weerstand. Hij heeft ook een actieve lift gehad, toch? Ja, maar die is meteen weer de gang in gebonjourd want hij had gewoon niet genoeg steun meer. Hij vond zelf wel dat hij een hele actieve stafunctie had, maar hij had geen kracht meer in zijn benen, dus zijn knieën konden zomaar onder hem vandaan schieten. Opstaan van de wc was ook een groot probleem, daar had hij de kracht gewoon niet voor. Hij had een ziekte waardoor je spierweefsel wordt omgezet in vet. Dat verslapt allemaal, en hij heeft geen kracht meer over. | |||
''Dan doen jullie veel met de hand tillen?'' | |||
Bij hem niet dus. Tillen doen we het liefst zo min mogelijk, zelf of met behulp van liften. Het duurt altijd erg lang voordat we eenmaal de grens over stappen om een apparaat in te zetten. Dat komt ook omdat mensen het liefst zo lang mogelijk hun eigen functies willen behouden. Zo lang mogelijk, want mensen willen zo lang mogelijk alles zelf willen blijven doen, met behulp van, terwijl het vaak toch een kwestie is van pluk- en trekwerk aan zo’n persoon. Bovendien moet je de techniek echt echt echt heel goed beheersen, wil je een mens op tillen. En als ze eenmaal bedlegerig worden, dan worden ze overgeplaatst naar een verpleegtehuis. En terminale cliënten blijven toch wel vaak. En dan heb je nog glijzeilen die je kunnen helpen. | |||
''Maar je probeert mensen zo min mogelijk te tillen terwijl ze zelf nog kunnen opstaan?'' | |||
Ja, dat klopt. Verder kun je ook denken aan een sta-op stoel. Als mensen moeite hebben met opstaan uit een lagere stoel, dan is een sta-op stoel geschikt voor hun. | |||
''Ervaart u regelmatig klachten die veroorzaakt worden door het optillen van een persoon? Welke?'' | |||
Nou, wel regelmatig rugklachten. We proberen daar wel iets aan te doen, om te overleggen met elkaar. “Hoe doe jij dat? Heb jij een makkelijkere manier?” | |||
''Hebben jullie dan allemaal een eigen manier van een cliënt helpen opstaan?'' | |||
Nou nee, dat toch niet. We proberen daar toch wel een lijn in te trekken. Dat is ook heel erg afhankelijk van de persoon. Maar per persoon organiseren we wel een bijeenkomst om te overleggen hoe dat we die persoon het beste op kunnen tillen. Dat is voor de cliënt wel het fijnste, om het iedere keer hetzelfde te doen, hè. Dan weet hij ook wat hij te wachten staat, en hoe zij tegenover ons als verpleegkundigen staan. Want anders is de ene de goeie en de ander de kwaaie. | |||
''Oke, dus een cliënt kan angstig worden door het vooruitzicht om opgetild te worden door jullie of met behulp van een lift. Ervaart de cliënt geregeld irritatie door getild te worden? Hoe gaan jullie daar mee om?'' | |||
Nou nee, ik denk niet zo zeer irritatie, maar een vorm van verlies, afscheid, weer een stap terug uit, dat is eigenlijk een rouwproces. Dat begint dan met autorijden, een heel groot stuk zelfstandigheid, je bent niet meer mobiel. Dan moet je altijd iemand opbellen, en bent niet meer onafhankelijk. Zo is het ook met opgetild worden. Het feit alleen al: ik krijg een prikkel: ik moet naar de wc. Dan sta je op en loop je naar de wc. Het idee dat je daar zit, en dat je denkt oh jee, mijn prikkel komt dat ik naar de wc moet, maarja dan moet ik weer eerst iemand gaan bellen, want er moet eerst iemand komen. Eigenlijk moet je die prikkel wel heel vroegtijdig voelen want anders dan kan ik het misschien wel niet ophouden en misschien zijn ze wel te laat. Dat zijn zoveel dingen veroorzaakt door die ene prikkel dat je moet gaan plassen. En het alternatief is zo’n ding in je broek. | |||
''Zijn er dan cliënten die jullie ieder moment van de dag kunnen opbellen om naar de wc te gaan?'' | |||
Ja. Maar als je toevallig bij een ander staat en je bent die al aan het helpen, ben je een half uur te laat. Dan spelen er wel irritaties. | |||
''Hoe ga je hiermee om?'' | |||
Je kunt dan alleen aangeven dat het nog een half uur gaat duren dat je er bent. Niet dat ze er rekening mee houden dat je er binnen 5 minuten bent. Soms kan dat wel, maar dat is maar net waar je mee bezig bent. Maar als je het aangeeft is dat minder erg. Als ze het maar weten. Maar we voelen allemaal met de cliënten mee. Als we onszelf in die situatie zien, dan denken we soms dat we er nog erger door geïrriteerd zouden zijn. | |||
''Verschilt het heel erg per persoon dat ze ongemak of angst ervaren bij het optillen? Of dat ze de voorkeur geven aan door jullie geholpen te worden of met behulp van de tillift?'' | |||
Dat verschilt inderdaad heel erg per persoon, maar ze geven echt allemaal, stuk voor stuk, de voorkeur aan dat wij ze zelf helpen met opstaan. | |||
''En waarom is dat zo, denk je?'' | |||
=== | Ze hebben dan meer het gevoel dat ze zelf opstaan, en niet dat ze zich volledig moeten overgeven aan een apparaat. Daarbij komt dat ze ons meer vertrouwen dan een apparaat. Zoals we al eerder hebben gezegd: vertrouwen is het belangrijkst in de zorg. | ||
===Summary results interview=== | |||
The lifting strategy as discussed with the caregivers of the RSZK is as follows. To lift someone out of bed a person hoist or a “turntable” can be used, but most times the clients are lifted by hand. The general experience that the nurses have with the clients with respect to the person hoist is that most people are afraid of these patient lifts. The reason is that people are seen as more trustworthy. However, this trust depends on the relation between the caregiver and the client. For example, if the client gets familiar with the caregiver he or she will trust the caregiver more easily. Giving clear instruction is also very important, as well as the enthusiasm with which the instruction is given. | |||
There are stand-up lifting systems, but only people who have relatively good functioning standing capabilities and trust in that ability can use them for the client is not comforted when using it. | |||
People want to be autonomous for as long as the can be. They will not like a tool because it means they can’t do certain things without help. If a caregiver helps with standing up it feels like you still do something, with technology this isn’t the case. It also doesn’t help that most people don’t like change. | |||
Sometimes demonstrating the “new” technology in form of a film will give more resistance towards it than just using the technology. | |||
Caregiver can oftentimes not get to clients in time to help the clients get up. This gives rise to irritation | |||
'''Methods for helping someone get up''' | |||
Getting up from a sitting position (in order of the client having a lot to little power ): | |||
* Hand on the back to give them the faith they can do this (caregiver hardily lifts) | |||
* | |||
Or | |||
* Let the client grab the caregiver around the neck | |||
* Caregiver puts knees against client’s knee | |||
* Stand up together | |||
Or | |||
* Grab client around body and head | |||
* Lift until they are upright | |||
'''Sitting up from a lying position''' | |||
* The care giver gives the client a hand and lifts them up | |||
Or | |||
* Grab shoulders and legs | |||
* Turn them towards the edge of the bed and lift the shoulders at the same time | |||
==CCVSD values in the interview== | |||
===Values in lifting by hand=== | |||
The purpose of this chapter is to reflect upon the care practice of lifting by hand and with a mechanical lift from an ethical perspective, with the article of Van Wynsberghe in mind <ref name="CCVSD" />. We will pinpoint the most important values in the act of lifting a person based on the interview done with the nurses of the nursing home RSZK in Reusel. | |||
During the lifting process, trust plays an important role. Caregivers indicate that clients respond better to being lifted when they have already created a relationship with a client. According to numerous studies, trust facilitates cooperative behaviour<ref>Eardley, A. (Ed.). (2010). Innovative Knowledge Management: Concepts for Organizational Creativity and Collaborative Design: Concepts for Organizational Creativity and Collaborative Design. IGI Global.</ref> <ref name="Coop">Feigenberg, B., Field, E., & Pande, R. (2009). Do social interactions facilitate cooperative behavior? Evidence from a group lending experiment in India. Mimeo.</ref>. To be more concrete about this, let’s use the following example. | |||
The client called mrs. Adams has to be taken out of bed every morning and helped back in in the evening. She is still relatively independent, as she can move around freely with some support provided by a cane or rollator. However, she needs help in the morning when rising from the bed and she needs to be be helped with medical stockings. Most of the day she spends seated, since she is weak in the legs. Therefore a caregiver comes in twice a day to provide her with these (and more) care tasks. | |||
Mrs. Adams mostly receives care from caregivers that visit her regularly, i.e. twice or thrice a week. When such a caregiver visits her, she listens to the instructions carefully. The set of actions to be taken are the following. | |||
The client starts in lying position, grabs the nurse around her neck, and is lifted to a sitting position on the edge of the bed. Then a break is held for half a minute. The next step is more complicated for both the caregiver and care receiver. The client puts her knees against those of the nurse. Then she is instructed to stand up with the guidance of the nurse. | |||
The difference between a regular and a one-time visit from a caregiver is this: the client tends to listen closely to instructions and fully trusts the nurse that visits regularly. Whenever a new caregiver is sent to Mrs. Adams, she fails to stand up because of bad timing and wobbly knees in the last phase of standing up with help of a nurse. The cause is that she does not fully trust the new nurse yet, and tries to rely on her own strength instead of making use of the nurse’s. Henceforth, trust in a client-nurse relationship is very important and can be gained by social interaction<ref name="Coop" />. Since establishing a bond with a client takes time, this is an essential factor in building this relationship as well. | |||
When lifting a person, the feeling of safety also plays an important role. It is actually linked to the value of trust. In the interview is addressed that the feeling of being safe with a nurse builds to the client-nurse relationship. | |||
One way to make a client feel safe is to put a hand on the lower back of the client when she is standing up partly on her own powers. On the one hand, touch ensures the nurse that the client is still there standing up and can feel when the client has lost balance. On the other hand, the client feels that the nurse still has the focus on her standing up and will catch her whenever she loses balance. | |||
Another advantage of this method is the satisfaction of the client. A nurse tells that sometimes she even meets resistance from the client whenever she needs to be helped to stand up from the bed. The method to deal with this is to give initiative to the client and let her stand up at own will. Plus, she will be helped to stand up minimally. Whenever she has regained some strength, she needs minor support. To ensure that this strength does not collapse halfway through the standing up process, a hand is held on the lower back for protection against falling, but the client feels the independence while standing up at own initiative. | |||
The resistance comes from the loss of independence, the caregivers agree. Metaphorically, a nurse tells it is actually a form of loss, farewell, a step backwards. In fact, it could be compared to the process of grieving. The first a client loses is being mobile. The driver’s licence is withdrawn, which causes being dependent on family, friends or taxi drivers. This is also the case with standing up. The fact that a client is dependent on a nurse to even get out of the bed after awakening is a great loss for a client, and sometimes even arises irritation. Therefore, the nursing home tries to make plannings in such a way that a client is visited daily by a regular set of nurses. A short explanation: these visits will be more sociable and clients tend to make chatter with the regular caregiver which causes distraction from the annoyance caused by the lifting. | |||
Of course not every caregiver can visit daily, but since clients seem to prefer regularity in their schedule, the team of nurses discuss for each client which method of lifting will be used as a standard. This way, the nurses adapt the method of lifting specifically for each client and take into account the client's’ preferences and those of the nurses themselves. Thus, the nurses are more comfortable when lifting a client and have less discomfort from their back, neck and shoulders. This way, the value of comfort plays a centre role in the lifting practice. | |||
Another advantage is that the client does not develop a preference solely based on the practice of lifting. By sticking to just one method of lifting per client, the client knows exactly what is ahead and the nurses also deduce their opinion towards them, while paying attention to their bodily behaviour and the way their instructions are followed. | |||
These instructions are of great importance. They should not only be very clear but also be posed in a respectful and appreciative way. One nurse indicates that repetition is very important. When a client is elsewhere with her mind, the practice of standing up will most certainly fail. With great enthusiasm, instructions should be repeated often and be very clear. Sometimes it might seem as if a client is commanded as if he were a pet, which can be avoided by being enthusiastic and for example giving a high five for succeeding once again. Because of this playfulness, the clients feel appreciated and respected and the nurse-client bond is strengthened. This might feel contradictory, but the alternative is being over-serious and businesslike, which results in a client that feels as if he or she were merely a way of making money for the nurse. | |||
==== | ===Values currently not respected=== | ||
The purpose of this section is to introduce the use of the passive person hoist and to determine exactly why such resistance is met against passive person hoists. Let’s first start with a scenario. Mr. Dirks is a male resident of RSZK Mariahof in Reusel. He lives independently and receives care in the morning and in the evening. He still has full body function but is weakened due to an illness that causes his muscles to convert to fatty tissue. Therefore, he is bound to a wheelchair all day long. The least of any resident of Mariahof, he expresses resistance against the passive person hoist. However, he uses it regularly and does not complain. His standing-up function is quite better than those of the other residents. | |||
To move from a lying position into a sitting position, he needs the help from the caregiver. After that, while sitting at the edge of the bed, the nurse fetches the passive person hoist, prepares it for the client and steps to the other side to control the buttons. Therefore, no physical contact between the caregiver and the client is possible. This also holds for eye contact, since the caregiver’s attention is fully directed towards the controls of the machine. The performance of the person hoist is of great importance for gaining trust in the machine.<ref>Cuijpers, R., & IJsselsteijn, W. (2014). Role inconsistencies in elderly care robots.</ref>. Whenever the movements are not natural for the client, this might lead to distrust. Then it is difficult for a client to have confidence in the person hoist. | |||
The support that is normally given by the nurse when the client is standing up, is now completely transferred to the passive person hoist. Thus, the client must have full confidence when using the passive person hoist, since he has no support from the nurse. The client must now rely on sound and instructions from the nurse. | |||
The resistance that mr. Dirks expressed before couldn’t be lessened by a demonstration. A nurse tells that there are given demonstrations on a regular base at Mariahof, but most of the time, the residents really dislike the idea. The cause that mr. Dirks finally gave in to the passive person hoist, is because of necessity. His balance was more and more off, and it became dangerous to lift him by hand. First, he made use of an active person hoist, but he didn’t have the strength anymore in the legs, which could cause his legs to slip out under him. | |||
According to the caregivers, the use of passive person hoists is delayed as much as possible. When finally the decision is made to use a person hoist daily, this is an absolute necessity, since the practice of lifting is done as least as possible. The team of nurses want the clients to keep their bodily functions as long as possible, since the clients themselves wish to be as independent as possible. For example, when a person has difficulty with rising from a low chair, they must consider purchasing a standing-up chair in order to stand up independently. | |||
Furthermore, when a client expresses a preference of being helped to stand up with the help of a nurse, their wish is respected unless it is no longer possible. Until the passive person hoist is a must, the clients will be helped by hand. | |||
Now the question arises why such a resistance is met by the clients. Let’s discuss a few topics that we have discussed together with the nurses, since they can most certainly empathize with their clients best. Plus, when a nurse-client bond is strong, the clients finally dare to express their true feelings about being lifted by hand and with a person hoist. | |||
Trust can be gained by experience or establishing a bond. To trust in a machine is hard for people that are of age, since that generation has not grown up surrounded by technology. A person of age 20 will more easily trust that the construction of the person hoist will have no difficulty carrying their weight, whereas elderly people do not fully trust that no accident will happen. According to nurses, this might be because of the different contact points with the client. An extra hand in the back that actually does not play a physical but only psychological supportive role comforts clients when lifting by hand. A machine does not provide this extra attention for a client. Therefore, they prefer lifting by hand with help of nurses. | |||
Fear of weakening is also given as a reason for clients to dislike being lifted with help of a machine. As we have just discussed, lifting by hand enables a client to use their full power and the nurse only has to supply extra help and support where needed. When using the machine, the clients do not have to use any strength at all and therefore might get the feeling that they cannot do anything themselves anymore. The next value is linked to this. | |||
Independence is another very important value when it comes to the care practice of lifting a client. When being lifted with help of a nurse, the clients stands up at own initiative. When being lifted by a person hoist, the client takes a passive role and has to fully undergo being lifted and has no say in the process. Because the client doesn’t have to use any strength, they might even feel they are not capable of standing up themselves or they are not allowed to do anything anymore. | |||
This is another loss in the eyes of the client. The nurses suspect that they feel inferior to other human beings that are fully functional and can move around freely. The care practice of being lifted with help of a nurse can be done in a very respectful manner, where human dignity plays an important role. The client’s wishes are very important and they are being dealt with with great respect. The warm and seemingly safe hands are very comforting for the client and make the client feel human. However, when being lifted with a person hoist, this might feel businesslike and disrespecting to a client, although the nurses do their best to treat the clients with great respect. The nurses that we have spoken to indicate that the lack of eye contact and the focus that goes to the controls of the apparatus contribute to the feeling of being treated disrespectfully. A study on eye contact in social interaction confirms this.<ref name="Eye contact">Bohannon, L. S., Herbert, A. M., Pelz, J. B., & Rantanen, E. M. (2013). Eye contact and video-mediated communication: A review. Displays, 34(2), 177-185.</ref> | |||
We conclude that hands-on care is greatly preferred to the person hoist or other machines because of (amongst other) these aspects. Note that we only have access to a nursing home that is in possession of person hoists and not a RoBear, so we have laid our focus on the person hoist, but we can compare this to being lifted by any machine, amongst others the RoBear. | |||
==Improvements== | |||
===New Values=== | |||
In this chapter we will discuss the most important values in the care practice of lifting a client. The focus lays on the aspects that are definitely lacking in the act of being lifted by a machine compared to being assisted by a nurse. Since we only had access to a nursing home that uses person hoists on a daily base but does not own a RoBear, we use this technology as a basis and compare this to the functions of the RoBear. From this viewpoint, we define improvements to the RoBear based on the experiences of clients with person hoists. Note that we must fill in the gaps ourselves between the somewhat older technology of person hoists compared to the RoBear. However, we argue that the same problems hold to some extent for being lifted by any machine that operates quite similarly. | |||
< | For any mechanical lift, the value that is at top priority is efficiency <ref name="CCVSD" />. However, as we have seen in previous sections, for a client the following values should also be respected and can be improved upon. The first thing that we consider is lacking, is the trustworthiness. We want to improve the trust of the client in the RoBear, for example by extra contact points of the RoBear with the client. We have seen that an extra contact point in the lower back is comforting and relaxing for the client although it might not practically be needed in the lifting process. | ||
Another way to solve this problem is a more natural way of lifting a client. Based on the position of the client’s body, the RoBear must formulate an action plan and lift the client accordingly. Then, the RoBear must be able to detect the position of the body of the client. This way, the RoBear will behave more natural and not scare the client or make the client feel dehumanized. Such a system is partially implemented in the “computer vision” subsection below. This leaves us at the next value. | |||
< | Human dignity is an extremely important value in the act of lifting a person. We have seen that the client loses some independence when he needs help standing up. Then we must at least try to give the client the independence it can still have. One way of doing this, is to have eye contact with the client and treat him with great respect.<ref name="Eye contact" /> When a nurse is present, he or she should be able to do this and not be distracted by the controls of the RoBear. Therefore, we want the RoBear to perform a string of actions autonomously. Whenever we want the RoBear in a home setting without a nurse present, it has to be able to look into the client's eyes before or during the lifting process. | ||
< | Furthermore, to give a client back some independence, he or she should be the one to take initiative before being lifted. Then, the Robear should behave according to the commands of the client. We aim for a RoBear that can give audiovisual feedback, in the form of full sentences or an interactive display for the client to use. With this user interface, the client should feel in control.<ref>Tidoni, E., Gergondet, P., Kheddar, A., & Aglioti, S. M. (2014). Audio-visual feedback improves the BCI performance in the navigational control of a humanoid robot. Frontiers in neurorobotics, 8.</ref> | ||
< | Looking back at the paper of Van Wynsberghe <ref name="CCVSD" />, we have pinpointed those values that the RoBear does not yet fully respect. Furthermore, we have made suggestions on how the RoBear should be improved accordingly. In the following section will be dealt with an enhanced strategy of lifting in order to improve the autonomy of both the RoBear and the independence of the clients. | ||
===New Lifting Strategy=== | |||
To improve both the autonomy of the RoBear and the feeling of autonomy of the care receivers, the RoBear should not only be able to lift a person all by itself, but also give the client the chance to help the RoBear in this process. Already when the person is getting seated from the bed, there are many differences between activeness and passiveness from them. To ensure the physical safety from a client, the RoBear should feel the amount of strength the client can still use himself to become seated, by using torque sensors in the arms helping the client get seated. If little power is needed, because the client can do much of the lifting himself, the RoBear should not keep pushing very hard and risk injuring the client, whereas when the client has little to no power, the RoBear can use a little bit more power. | |||
The main lifting strategy, in the case where a client needs to go from laying down to sitting up in bed, is to first check the position of the body, using the cameras to be attached to the body of RoBear. Then the first arm is to be inserted under the neck of the client, while at the same time also giving the client the possibility wrap their arm around something, to give them the possibility to pull themselves up. This needs to happen in a soft and safe way, and thus the head and shoulders also need to be supported by the arm during the lift. When the upper body is lifted far enough, the second arm of RoBear can be inserted under the middle of the back, to give a bit more support to the client while sitting up. With this arm, the possibility of rolling off the grip of RoBear should be prevented, so the end should be tilted towards RoBear. | |||
When the client is started sitting up, the knees need to be located by RoBear, using its cameras. Then the knees need to be lifted, which can be done using only a small arm. After a little bit of support is also given to the upper legs, the client can either be rotated towards the side of the bed and relieved from their leg support if they are able to stand up themselves, or be lifted off the bed if they can not. On the side of the bed, the clients are given a little rest, after which the rest of the lifting procedure is started. | |||
For getting from seated to standing, the arms of the current RoBear can be used. The client will hold their arms on top of RoBears arms, and lift up from the bed, with help from RoBear. If possible, RoBear then slowly releases the client, to still give the client the satisfaction of standing up on their own. From the interviews, we got the note that a hand on the lower back is a very important part in getting a client to trust you. In this case however, as the RoBear is positioned in front of the client, a soft hand below the arm should suffice. Because this hand should not only be there to touch the client, but also to feel if the client is about to fall, very sensitive touch sensors are important here. If the now standing, or almost standing, client begins to fall, the RoBear should use its two soft arms to catch the client underneath the armpits. | |||
Overall, the most important aspect is the safety of the client. That is also why the Robear should at all times keep his eyes on the position and movements of the client, to keep them from falling. | |||
===New Appearance of the RoBear=== | |||
Now we have discussed the new lifting strategy as it will be executed by the RoBear, we will discuss the new features that should improve the RoBear. | |||
First of all, the RoBear should have a Computer Vision system, which entails the presence of two cameras and body position recognition software. Moreover, the RoBear should detect the body position and classify it in a set of body positions, call it a library. Then, it picks the set of actions belonging to this type of body position. Since this has been studied elaborately, we will discuss this in the next paragraph. | |||
< | The Robear should also have a body roughly the size of a human, else it would not be able to carry a person or help him/her to stand up. The original robot was the face of a bear. The bear like appearance is better than a more humanlike appearance. The human form would imply that it is able to act and socialize like a person, which it can’t. Especially elderly people who have not seen comparable technology can get frustrated when the robot doesn’t act as expected. Another advantage of the bear like appearance is that it feels less like a human sees them in an “shameful” state.<ref> Kahn Jr, P. H., Ishiguro, H., Friedman, B., Kanda, T., Freier, N. G., Severson, R. L., & Miller, J. (2007). What is a Human?: Toward psychological benchmarks in the field of human–robot interaction. Interaction Studies, 8(3), 363-390.</ref>Now it’s only a bear, bears don’t seem to judge based on social norms. | ||
It is better that the robot looks like a bear, something they can recognize, than a robot. The more the robot deviates from a known for the more it will look like technology. For a lot of people technology is scary and unpredictable. Overall not something you would trust to help people get out of bed or even carry them. | |||
Therefore the choice of two arms is most natural, as we want the RoBear to have the outward appearance of a bear. The lifting strategy is based on that of a human, therefore we will opt this for the RoBear. Furthermore, the RoBear is now designed with two arms, and we do not seek to change this when the alternatives have not proven to be better. | |||
An alternative would be more than two arms or more general many more contact point. A suggestion would be a mattress-like structure, such as a bed that can be moved in any body position or a stand-up chair. Since those already exist, and there is still need for a nurse to come by and help the clients out of these furniture items, the original design of the Robear seems more suited. Furthermore the general goal was to make improvements to the RoBear. Since the robot can lift people with two arms it will remain designed that way. | |||
Finally, when the RoBear will be introduced at people’s homes, the RoBear must be compact in size. A maximum width must be assigned, based on the width of a standard door. Moreover, the problem must be tackled that the RoBear is capable of moving across an uneven floor with thresholds or bumps. | |||
===Interaction=== | |||
< | More features that could be improved will now be discussed, with the aim for the RoBear to interact more with the clients, which we refer to human-robot interaction. It has been shown that a good robot-human interaction can help clients willingness to use the robot and help build trust.<ref>Dautenhahn, K. (2007). Socially intelligent robots: dimensions of human–robot interaction. Philosophical Transactions of the Royal Society of London B: Biological Sciences, 362(1480), 679-704.</ref> | ||
The first improvement that we would like to discuss is a user interface. To illustrate this: imagine a RoBear that has a touchscreen and built-in speakers and a microphone. For example, the screen could show the body detection of a person, or show a demonstration of the lifting process. This way the client can see what the RoBear is doing, which will help to understand how the robot works. The Robear will no longer be a mysterious piece of technology. | |||
Moreover, the RoBear could play an audio fragment to tell a person what will happen. Especially clients with dementia could be helped by a continuous reminder throughout the lifting process of what they should be doing and what they could expect next. | |||
Furthermore, emotion recognition could be implemented. With this function the robot can see if the client is in distress or otherwise tries to stop him. Optimally the RoBear would be able to stop the lifting process at that point, but even calling a nurse for help would be helpful. | |||
Finally the RoBear could ask feedback when the process is done. This way the client feels like the robot takes them into account, the robot can adapt its general strategy and in an optimal situation it can adapt its lifting strategy on a personal level. For example if a client has a bad knee, the RoBear might avoid putting a force on that joint and instead try to place its arms elsewhere. | |||
===Computer Vision=== | |||
Computer vision is already an important aspect of all our lives. When taking a selfie, your camera can automatically determine when you are smiling and take a picture accordingly. When going through customs to some countries, the passport scanner is automated and can detect and compare your face without need for human interaction. | |||
Until several years ago, many applications of computer vision were outside the capabilities of computers and smartphones. Nowadays, thanks to radical improvements in both hardware and implementation, basic tasks for computer vision (such as object recognition and event detection) are well within the reach of even the weakest smartphones and laptops. In order to provide a faster user experience, modern smartphones come equipped with [https://en.wikipedia.org/wiki/Vision_processing_unit VPU’s] that handle vision-related tasks. | |||
Improved computer vision has already very much improved the automation of simple tasks, such as quality assurance at factory conveyor belts. We believe that computer vision can not only improve the autonomy of these simple tasks, but also the autonomy of senior citizens during their daily lives. If the robear is equipped with cameras that allow it to do some scene reconstruction, it will be able to ride to the client’s bedside and determine if the client is ready for pick up autonomously. This would free up caregivers to focus on the clients themselves instead of the lifting process, and lift a heavy burden from their shoulders. | |||
In robotics, computer vision is absolutely crucial for many steps in any decision-making process, from detecting the room and deciding what path to take (scenery reconstruction) to checking whether the ball to be lifted is actually getting off the table (event detection). However, computer vision as it is currently used in robotics is not very refined and often needs to be done in a high contrast situation (e.g. a football game where the field is green and the ball is bright orange) for it to work correctly. In the scenario we decided upon, this will not be the case. The client may be wearing any color of clothing, and it might not contrast very well to the color of the walls, ceiling and floor. This means we cannot rely on traditional methods like testing valley regions in gray-level images. Instead, we will use a very well trained neural network to do detection. Further on, we will introduce a second camera in order to do depth perception as well. | |||
====Pose detection on humans==== | |||
Even with the advancements made in the last few years, full pose detection on humans has been a big hurdle. More traditional methods (for example, those bundled with OpenCV) have often focussed on detecting a general bounding box of a human or other object, others on using many hidden layers and a final softmax layer to determine the pose from a set of possibilities. On the CVPR (Computer Vision and Pattern Recognition) conference in 2016, the ‘best demo’ award was won by “Convolutional Pose Machines” by Shih-En Wei, Varun Ramakrishna, Takeo Kanade, Yaser Sheikh. Based on the released CPM from this demonstration, OpenPose was developed. OpenPose is a library for exact pose detection on humans, and the network used is fast enough for a medium-power laptop to do real-time pose estimation. This does require the input images to be rescaled down to only small fractions of the original size. | |||
====Disparity mapping==== | |||
OpenPose’s output is a list of all the detected features and their locations within the input image. This is already a big leap, but cannot yet be used for full reconstruction as a dimension is still missing: depth. It it possible to do some estimation of how far away a person is based on only two dimensional images, for example by knowing the size of certain features (such as the distance between the shoulders and hips) and assuming the person is always in a certain pose with respect to the camera. These are, however, too many assumptions for the task at hand. In order to accurately determine the distance to objects using two dimensional images, a second camera and a way of determining the new data is needed. | |||
The first was relatively easy, two cheap pinhole webcams of type “TRUST Webcam” were bought, the PCB’s and lenses removed and placed within a wooden support structure. The final result is displayed in the image below. This newly fabricated stereoscopic camera gives two 640x480 images at 30 frames per second, with some noticeable delay. It is noted that the budget for cameras on the actual RoBear is (or must be) at least an order of magnitude higher, as the difference in the delay between the cameras is already noticeable even without determining actual distance values from it. It is suspected that this delay will have very little influence as long as the target is not moving. | |||
[[File:2016Group2Camera.jpg|thumb|none|600px|The current camera setup.]] | |||
is | |||
For the second problem, three different strategies were determined. All three are based on calculating the disparity (in pixels) between the left and right channel images. This disparity has a certain relation to the actual distance that can be determined and calibrated at a later point. | |||
The first method was to use OpenCV’s native StrereoSMBG method. Unfortunately, even after rigorous tweaking it was found that this method introduces a lot of noise and is computationally a lot more expensive than is needed for our purposes. | |||
The second is to simply run the OpenPose network on both the left and right images and calculate the disparity based on where the network detects each of the eighteen features in both of the images. It was found that again, this method introduces a lot of noise (the network detects the features with a certain uncertainty, and the actual detected points wiggle a lot in some situations) and is again too computationally expensive. | |||
The third and final solution would be to detect each point in one of the images (for example the left channel), then take a small area around each of the (subset of the-) eighteen detected points and correlate them with the other (i.e. right) channel. This was found to be the best method, introducing the least noise and being much less expensive than the other methods. | |||
For the correlation, OpenCV’s native CV_TM_CCOEFF_NORMED algorithm was used separately on all color channels and then summed. The coordinates of the maximum of the resulting 2d-map is assumed to be the location of the detected feature in the other channel. The difference in the x-coordinates between the same features in both channels is the disparity and can be used to determine the distance to the detected feature. | |||
====Scene reconstruction==== | |||
In a perfect world (or with a more expensive stereoscopic camera), the disparity ranges | |||
The setup of the camera’s is not perfect and the angle between their optical axes is very much non-zero. This makes the (simple) mathematical interpretation of the disparity quite useless, but we can still calibrate the disparity to match with distances. We find a relation of | |||
<math>-x = \dfrac{0.0486149 \cdot d+64.0587}{51.9407+d}</math> | |||
Where x is the distance and d is the disparity in meters and pixels, respectively. | |||
The OpenPose library detects each of the eighteen features separately, and contains native code that classifies each feature as belonging to a certain person. This is usually quite accurate, but can fail if people are standing close together in positions where not all features are visible. As this is usually not the case in the lifting-from-bed scenario as we can place the cameras in such a position that all features of the client being lifted are accounted for, we can assume that this will work fairly well in our scenario. The final output of our software layer on top of OpenPose is given in the figure below. Code is available upon request. | |||
[[File:2016Group2FinalOutput.png|thumb|none|600px|The final output of our software model. The blue lines connect the detected features, the grey lines on the features indicate the (pixel-)distance between the features in the left and right channel. The top view gives the best guess distance of the feature from the camera in meters.]] | |||
==== | ====Interpretation by the robot==== | ||
One of the main problems that have to be solved mainly by using computer vision is not only detecting where the person is, but also driving towards the person, deciding whether or not the person is in a viable pick-up position (and possibly instructing them on how to get into such a position from their current position), and moving the arms around the client’s shoulders and or back/neck. From that point out, most of the sensory work will be done by the torque sensors in the joints of the robot. | |||
One of the reasons the camera’s we use for the detections of the client are in the robot and not fixed to the room - which can in some situations be cheaper and would also allow the system to track the absolute position of the RoBear - is this very point. Affixing the stereoscopic camera to the robot would allow it to use a relatively simple decision system to determine whether the client is in a position that allows for pick-up, based on only relatively simple parameters like the angle between certain joints or the angle between the back and the horizon. These parameters could be based on our lifting strategy. We have not focussed on actually creating such a decision method. | |||
of | |||
===Implementation=== | |||
=== | |||
When a client needs to be lifted, it is important that they know exactly what needs to be done by them and what is going to be done with them. RoBear should thus be able to communicate by speech to the client. To give the client a feeling of trust in RoBear, and to keep their dignity up, these instructions should be given in a friendly manner, and not in a commanding way. Doing otherwise will result in the client not acting to their full potential, and maybe hurting themselves. | |||
Furthermore, for the client to get a real sense of control, they should be able to give commands or suggestions to the RoBear. The easiest and most available way for doing this is by using voice commands. This means that the RoBear should have a microphone built in, and also an algorithm to detect certain commands. Commands such as stop and wait for instance are easy ways to detect stress or discomfort in people, and give the RoBear more ways to check if it needs to stop, go back or speak to the client. Also, there should be commands with which clients are able to call for the RoBear and tell him what he wants to do, and what kind of help he needs. | |||
As specified above, the RoBear would need force, position and torque sensors to feel the amount of power a client can still produce by himself and the amount of help they need from RoBear. These sensors would be situated in the joints of the arms of Robear, measuring both the direction and the force that the client excerpts onto the arms of the Robear, so that if the client pushes back onto the arms the RoBear does not push further and injure the client in any way. Because of these sensors, the RoBear can deliver client-cooperative lifting, not only acting as a way of lifting, but also helping in a way to rehabilitate the client with lifting himself, or keep them able to lift themselves in this case.<ref>Nef, T., Mihelj, M., & Riener, R. (2007). ARMin: a robot for patient-cooperative arm therapy. Medical & biological engineering & computing, 45(9), 887-900.</ref> | |||
=== | ==Conclusion== | ||
The goal of this project was to make improvements on the RoBear. It was shown that the robot doesn’t act trustworthy and lifts people in a dehumanizing way. Furthermore to use the robot a nurse needs to do a lot of work. The lifting can only start when the client is in a position most elderly cannot reach by themselves. | |||
To solve the first problem the robot will adopt a more natural way to lift clients. The solution described in “New lifting strategy” is one that nurses use now. This was concluded in the interview. This strategy is better because clients feel they are more in control. Another new aspect is that the robot will now also give audible feedback, encouragement and explanation about what will happen next. | |||
To help the nurses a program was made that detects the way the client is lying. That way even if the client isn’t in the exact right position the robot will still be able to find the point where it should lift. Computer vision makes this possible, through this the robot will be able to identify the joints and the position of the client. It also enables the robot to look in the client’s eyes before doing something, this feels more like natural interaction and might comfort the client. | |||
When the suggested improvements would be implemented in the RoBear it would be more practical and less scary to use. It is a step in the direction of giving clients their independence back. Unfortunately the goal of a robot that could lift people without supervision was not met. | |||
=== | ==Discussion== | ||
Before the RoBear can be used there are a lot of improvements that need to be made. Seeing that this is only an eight week long project, the original goal of the client being able and willing to use the robot for lifting without help of a caregiver was too ambitious. This is why the project only focused on a subset of RoBear’s flaws. | |||
It also means that there was no way to test if this is actually a better design. The only information this project is based on are older papers and an interview with nurses that care for elderly on a daily basis. These papers are based on similar robots but there might be factors that were not taken into account when applying the theory to the RoBear. | |||
If there was more time available for this project, a few more things could be looked into; first of all, the clients and their next of kins could be interviewed on their opinion on the project and what they expected from it. Based on their answers, the design could be reevaluated. Also, a prototype of the improved RoBear could be constructed and tested by all users. | |||
== References == | |||
<references /> | |||
</div></div> | </div></div> | ||
[[Media:Example.ogg]] | |||
Latest revision as of 20:55, 26 June 2017
<link rel="stylesheet" type="text/css" href="theme.css">
Project Robots Everywhere 2016/2017 Group 2
Group members
- Joris Dalderup 0942945
- Frouke Hekker 0897373
- Ellen Vugts 0892371
- Bram Wieringa 0893231
- Mireille Moonen unknown
Problem definition and setting
Problem definition
All around the world, robots are being introduced in daily life. In healthcare, the prospective is that robots will facilitate elderly or disabled persons to be more mobile and enable them to move around freely. Take for example the scenario where a person has to get up from his or her bed to get up and start the day. Where in earlier days the manual lifting of a person by two nurses was required, the goal is that with present day technology a robot could be used to lift a person for laying down to standing up in a safe and comfortable manner. For this, we will improve designs like the RoBear. The RoBear is a robot that can lift people out of bed. It moves around on wheels and has two big arms that are covered in cushions. Its head resembles a bear's head in a cartoonish way, hence the name. However, this robot is not widely used yet in nursing homes and still has its flaws. A nurse has to help every step of the way and it cannot help to stand if the client is lying down. In this report, we will explore how the RoBear functions and what these flaws of the RoBear entail.
Setting
In order to see in what degree lifting a person is a problem in healthcare and how it is coped with right now, an interview will be held. A few nurses of the RSZK, which stands short for Regionale Stichting Zorgcentra de Kempen, will be interviewed as they have more expertise on this subject. This institute facilitates home care and help at home, but also consists of several nursing homes. In the latter, the distinguishment is made between two types of nursing homes the first, where people live that cannot live independently due to old age, illness or a handicap, and the second, where intensive care is given to people that require heavy medical treatments because of severe physical or psychological handicaps, for example after cerebral hemorrhage or dementia. For this project, we will consider the RoBear as a robot that could be integrated in the nursing homes of the first type. These home centres consist of several care apartments, that are mostly inhabited by elderly people.
Movie from RSZK Mariahof te Reusel.
This nursing home is inhabited by people that live semi-independently, but receive care they require with some daily tasks, such as help with showering, help with going to bed, medical stockings et cetera. The general lay out of the rooms is similar, all include a bed/living-room with bathroom and an own kitchenette. The room itself is not furnished, so each client is free to place furniture at his or her own liking. However, the arrangement of the furniture must be conform rules that are introduced so that nurses are not impeded in their movement while caring for their client.
Why introduce a lifting robot?
One of the tasks of the nurses is to help the clients out of bed in the morning. The care practice of lifting involved in this can cause physical injury for the nurses, such as complaints to the back, hip and knee. Another problem is that there are not enough nurses and the clients cannot get up at the time they want to. This lifting robot should give them more autonomy. However, the quality of care should not deteriorate. The RoBear is merely a tool for the people to increase independence, in order to enable a person to get up and move around more freely at own will. The care tasks of the caregivers will not be replaced because of the introduction of the RoBear, it should just enlighten the stress on the care task of lifting a person for the care givers.
Goal
In particular, the aim is improvement of the care practice of lifting a client in a safe and comfortable way with a certain degree of autonomy. The robot must be able to lift a client in a safe way, which entails that the client can under no condition fall off of the RoBear when only one nurse is present to guide the client in the arms of the RoBear. In a later stadium, the RoBear should be able to lift a client safely without any supervision. This way, the client can get up at own will. However, this might be a bridge too far. In particular, we would like to examine and improve the way of lifting. We want to stress that the goal is for the RoBear to operate autonomously, but that the RoBear does not replace a caregiver. It should only assist in the act of lifting a client, whereas the caregiver still is in charge of the overall care of the client. Because of the RoBear, the caregiver has more opportunities to care for the client and fully focus on his or her needs.
RoBear now
In this section, we will discuss the RoBear’s appearance and other features. These will be linked to certain values that we think are important for a care practice. In a subsequent section, we will look into the importance of those values in care by an interview with professionals of a care institution. After pinpointing the RoBear’s properties, we will describe the way the RoBear lifts a person.
Values
The RoBear is made to help nurses lift a patient in and out of beds or chairs. This allows the nurses some extra time for more personalised care or to talk to the patient about unrelated things, for example in order to make the patients feel less lonely.
The RoBear is shaped like a bear with the intent to look less threatening. Most robots are in a smaller size or look more like lesser known animals to prevent falling into the uncanny valley. A robot is said to be in the uncanny valley when it accurately resembles something or people but just not enough to fool them (see the picture below). However, when the intention is to resemble a person or animal but one can clearly distinguish the robot from the real thing in size or shape, then this so-called uncanny valley effect is prevented, think for example of a plush stuffed animal.
Seeing that the RoBear has to be human sized in order to lift a human being, it had to use other ways to look non threatening. However the cartoonish face it has now doesn’t seem very trustworthy.
The bond between a patient and a nurse must be formed on trust. Most patients can do very little without adequate help from a nurse, if this nurse is to be helped by a robot, then the robot must be trustworthy too. This is extra important when lifting people as they are helpless in the process.
There are a few ways to help create trust that even robots can use. The first step is competence, the robot must be able to execute the task fluently and without stops that could be seen as hesitation. Secondly there is communication, by talking or more accurately by explaining what is going to happen and making sure it will, makes one reliable. At last but certainly not the least important thing is eye contact, thereby acknowledging the patient. If this is not done the process is dehumanizing. Especially when lifting people, else it would be as if the patient is a thing instead of a person.
The RoBear only has the first step, it is up to the nurse to make the patients at ease. This doesn’t help since the RoBear now isn’t trusted but the nurse also has less tools to gain trust (usually touching patients helps this bond) .
Lifting Strategy
To get from the patient from the bed the robot will move towards it and extends its “legs” to be more balanced. The nurse will put the patient in a position see the first picture.[1] The RoBear can now extend its arms, the will go under the knees and support the back of the patient. The nurse needs to fasten to straps that will connect the arms of the robot and support the patient so they cannot fall between the arms. The patient can now be lifted and moved to a place where the chair is. The robot will slowly lower the patient into the chair while the nurse holds the chair under the robot and pushes it in place. When the patient sits, the straps can be put removed and the arms retracted. The whole process is shown in the picture below.
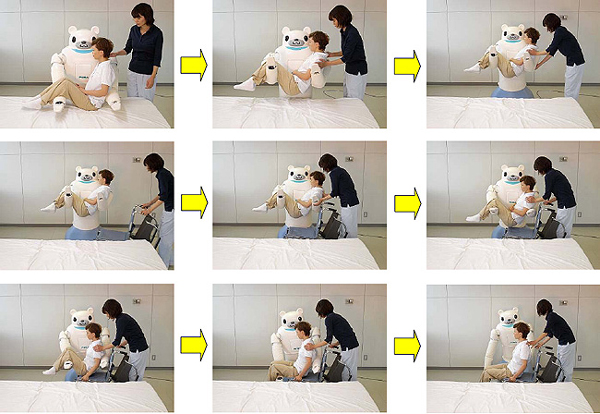
To get out of a chair and stand up, the robot will move in front of the patient while the nurse holds the chair in place as shown in the picture below.[2] This time not only the “legs” will extend but also a platform for the patient to stand on. The arms of the robot will close around the sides of the patient as they can hold on the the robot’s shoulders for support. The RoBear will slowly lift the patient, meanwhile the nurse moves the chair away to make room for the patient to stand. This can be seen in the last picture.


Current implementation
The RoBear can be controlled by a tablet in its back. It uses three types of sensors, including torque sensors and Smart Rubber capacitance-type tactile sensors made entirely of rubber, which allow for gentle movements, ensuring that the robot can perform power-intensive tasks such as lifting patients without endangering them.[3] The last sensor is a kinect that should be able to detect bodies in front of it, but is at the moment blocked by its mouth. [4]. Another flaw in this robot is its difficult operation and maintenance.
Care Centered Value Sensitive Design
In this project, the article Designing Robots for Care: Care Centered Value Sensitive Design written by Aimee van Wynsberghe will be used to analyze the RoBear as a care robot that is about to be introduced in care homes. In this article is expressed that care robots need to be reflected upon on an ethical level in order to ensure that the values and dignity of clients are not impeded by the introduction and the design of these care robots.[5] The framework she has devised has been put to use for retrospective analysis for the mechanical lift. Our aim is to improve the RoBear before the introduction in nursing facilities with help of this research project. First of all, a team of caregivers of a local nursing facility which works with mechanical lifts will be interviewed to determine the important aspects in the care practice of lifting. Based on their answers, the important values will be determined and from there on, improvements will be formulated for the RoBear. Of course, the RoBear can be classified as a mechanical lift. However, we will also go into detail about the features that are unique for the RoBear.
Interview
Questions
In order to pinpoint the values that are very important for the quality of a care practice, a questionnaire has been made.[6] A team of nurses that work closely with elderly people that live in a care institution and come across the care practice of lifting regularly has been interviewed. This lifting is either done with their own strength, which we will refer to as ‘by hand’, or with use of a person hoist owned by the care facility. As we really want to go into deep discussions on the subject, the questions might be out of order in the execution of the interview. Thus, we will hook into interesting aspects of what the nurses tell us, resulting in an interview as a whole. The interview is held at the care facility Regionale Stichting Zorgcentra de Kempen at the Mariahof located in the center of Reusel, where one of our group members has talked to five members of the team. The interview has been recorded and has been elaborated on paper, based on the audio file with the recording of the interview. Because of privacy issues, this file will not be shared digitally. Moreover, the names used are fictional because of privacy issues of the clients of the RSZK nursing home. The context is the care facility: an institution where elderly live independently in one of the apartments with own kitchenette and bathroom.[7]
The questions we have prepared for the interview are the following:
- Informatie over verzorgenden
- Wat is uw functie?
- Op welke afdeling werkt u?
- Wat is uw leeftijd?
- Tilmethoden
- In welke situaties moet een cliënt worden verplaatst door middel van optillen? Van welke naar welke houding
- Scenario: Wanneer een cliënt moet worden verplaatst van een liggende naar staande positie, welke methode gebruikt u het meest? Beschrijf de methode stap voor stap. (Serie van handelingen)
- Zijn er ook andere veel gebruikte methoden?
- Hoe bepaalt u welke methode het beste kan worden gebruikt?
- Als een cliënt (het aangeeft dat hij) zich niet op zijn gemak voelt bij het optillen, hoe stelt u deze dan gerust?
- Ervaart u regelmatig klachten die veroorzaakt worden door het optillen van een persoon? Welke?
- Ervaart de cliënt geregeld angst door getild te worden?
- Ervaart de cliënt geregeld irritatie door getild te worden?
- Ervaart de cliënt geregeld ongemak door getild te worden?
- Hoe gaat u met deze emoties om?
- Tillift
- Hoe verandert de reactie van cliënten op getild worden als er een tillift wordt gebruikt? Denk aan angst, zich veilig voelen, ongemakken, irritaties.
- Hoe gaat u hiermee om?
- Reageert u hier zelf ook anders op en zo ja hoe dan?
- Relatie verzorgende-cliënt
- In hoeverre is vertrouwen een belangrijk onderdeel in het verplaatsen van een cliënt?
- Hoe is uw relatie/band met de gemiddelde cliënt?
- Draagt deze relatie bij in het vertrouwen in het til-proces?
- Zijn er nog vragen die ik niet heb gesteld die volgens u nog van belang zijn?
The interview
In this section, the interview that has been held with the team of nurses of RSZK Mariahof in Reusel has been elaborated on paper, based on the audio file with the recording of the interview. Because of privacy issues, this file will not be shared digitally. Moreover, the names used are fictional because of privacy issues of the clients of the RSZK nursing home.
Informatie over verzorgenden:
Wat is uw functie? Op welke afdeling werkt u?
We zijn een team dat zowel gespecialiseerd is in de thuiszorg, dit betekent niet alleen hier in de instelling maar ook bij mensen thuis in de dorpen Reusel, Lage Mierde, Hooge Mierde en Hulsel.
Wat is uw leeftijd?
Onze leeftijden liggen tussen de 24 en 55 jaar. Maar er werken bij ons mensen van verschillende leeftijden.
Tilmethoden
In welke situaties moet een cliënt worden verplaatst door middel van optillen? Van welke naar welke houding
Een aantal cliënten wordt ‘s ochtends vroeg uit bed gehaald alvorens het aankleden of wassen. Soms wordt er dan gebruik gemaakt van een tillift of van een draaischijf. Vanochtend ben ik nog bij mevrouw Adams uit [Lage] Mierd[e] geweest en die wil ook vaak ‘s middags naar bed. ‘s Ochtends gebruiken wij de tillift eigenlijk niet, mevrouw wordt met de hand uit bed getild. Dan haal ik haar uit bed als volgt: dan liet ik ze vasthouden, en zette ik mijn knieën tegen haar knieën en instrueerde ik haar heel goed: en nu staan. En dan gaat ze mee staan, draaiden we en dan zette ik ze zo weer terug [op bed].
Dus dan haal je echt iemand uit bed of help je iemand er weer in? Dus dan begeleid je echt iemand vanuit liggende positie uit bed om ‘s ochtends op te staan?
Ja. Bijvoorbeeld mevrouw Beckers. Deze ochtend had ze toevallig de kracht om zelf op de rand van het bed te zitten toen wij er waren, maar meestal help ik die ook vanuit liggende positie omhoog, want ze kan dat vaak ook niet (ja ze kan het wel, maar...). Die geef ik dan een hand en die draai ik dan vanuit liggende positie naar een zittende, voordat ik haar help opstaan.
Dus dit zijn allerlei verschillende mensen die geholpen moeten worden met een transfer?
Ja. Maar dit is hoeft niet perse altijd zwaar te zijn. Soms is het voldoende om een hand aan te bieden en in de onderrug te steunen om mensen het vertrouwen geven om op te staan, maar dit kunnen ze dan vanuit eigen kracht. Maar die begeleiding/dat vertrouwen hebben ze dan nodig. Maar in Lage Mierde moet je mevrouw echt om het hoofd heen [vastpakken] en mee rechtzetten. Voor je rug is dat wel echt heel belastend.
Ervaren mensen angst bij dit optillen? En hoe gaat u daar dan mee om?
De meeste mensen vinden tilliften echt super eng, en willen er dan ook absoluut niet in.
En het tillen zelf, wat u als verpleegsters doet (met de hand)?
Dat optillen vindt ze minder eng, en dan wordt ze ook wel ondersteund. Ja, maar volgens mij vertrouwt ze gewoon op de mensen die dat doen. En dat verschilt ook echt per persoon. Want als ze iemand niet vertrouwt, dan gaat ze ook minder goed staan.
Maar dan moet ze eerst een relatie opbouwen met de verpleegkundige, en dan pas durft ze geholpen te worden met opstaan?
Bij haar is dat heel sterk. Want bij de een vertrouwt je beter, en dan is het hup! en dan hoef je niks te doen, en bij de ander, die vertrouwt je niet en dan gaat het veel moeilijker ook. Het scheelt wel dat hoe meer dat je er komt, dat merk ik nou wel, hoe vertrouwder dat ze ook met jou wordt.
Dus als je twee, drie keer in de week bij iemand langsgaat, dan vertrouwt ze ook alles wat je met haar doet?
Ja, ja zeker wel. En dan is het vaak ook de instructies die je ze geeft, want je moet constant tegen haar zeggen: goed blijven staan, knieën recht, goed gaan staan, je blijft gewoon constant herhalen.
Maar dan moet ze zelf gaan zitten vanuit liggende positie en dan help je haar opstaan?
[Demonstratie] Ze ligt in bed, en dan moet je haar wel helpen mee recht komen zitten op de bedrand, en dan pak je haar bij de benen en de andere hand bij de schouders. Dan zeg je 1, 2, en dan draai je haar in een beweging op de bedrand [in zittende positie]. En dan laat je haar je vastpakken om de nek, en dan plaats je haar benen tegen de knieën, en wederom 1, 2, staan en draaien. Zelf moet ze haar knieën dus mee buigen. Zo werkt het ook met de postoel. ‘s Middags zit zij dan in de rolstoel, pakt ze de tafelrand vast, dan zeg ik dus: blijven staan, knieën recht. Dan laat je de rolstoel ergens staan, zeg: “blijven staan” en schuif je de stoel bij. Meestal probeer je dan met 1 hand contact te houden. Dat is voor de veiligheid: het is voor jouzelf dat je voelt wat dat zij doet, en voor haar om te weten dat ze moet blijven staan. En als ze dan klaar is, dan hou je haar vast in de onderrug, en pak je de rolstoel (die heel zwaar is). Intussen hou je haar dus vast. Dan geef je een high five en zeg je “goed zo!” en dan glundert ze helemaal. Dat enthousiasme is ook heel belangrijk.
Dat contact is dus voor jou heel belangrijk, om te voelen dat ze nergens naartoe gaat, en voor haar om te voelen dat je nog niet klaar bent en ze moet blijven staan?
Ja, precies.
We hebben nog een cliënt waarbij we de stalift wel gebruiken, genaamd Dirks, en die maakt er goed gebruik van. Die vindt het ook niet eng. Hij heeft ook een betere stafunctie dan anderen.
Werkt de stalift soortgelijk als wat jullie doen wanneer een persoon vanuit zittende positie wordt geholpen op te staan?
Ja, die ondersteuning die jij normaal doet, doet nu de lift. Helemaal zelfstandig. Jijzelf staat aan de andere kant de knoppen te bedienen, dus je kunt niet met een hand op de onderrug contact houden. De cliënt moet dat dus helemaal zelfstandig durven.
Dat verschilt van persoon tot persoon dat ze dat durven?
Ja, echt wel. Sommigen durven dat echt niet.
Ook niet als je het zelf eerst voordoet? Vaak is het eerst zien, dan zelf proberen.
Nee, ja, dat hebben we nog niet geprobeerd. Dat is serieus een best goed idee.
Dat je eerst een demonstratie geeft, en dan dat de oudere het misschien ook durft?
Meneer Dirks heeft nog een actieve stafunctie. Daarbij werkte zo’n demonstratie helemaal niet, vond hij helemaal niks, en dat riep alleen nog maar meer weerstand op. Met hulpmiddelen voor steunkousen laat ik wel ooit een filmpje op youtube zien. We hebben wel eens een demonstratrice gehad, waar we met een heel stel bij zijn geweest, met een lift en een postoel om ‘s avonds te gebruiken, en meneer Adams had zoiets van ja daag, dat gaan we niet doen. Dat riep alleen maar meer weerstand op. Dat was voor mijn tijd. Hoe hebben jullie dat toen gedaan dan, het vertrouwen van meneer Adams inwinnen? Op een gegeven moment moest het gewoon, het kon bijna niet anders. Hij had zelf helemaal geen balans ofzo meer, hij moest zichzelf er aan over geven. Maar wel met heel veel schrik en heel veel weerstand. Hij heeft ook een actieve lift gehad, toch? Ja, maar die is meteen weer de gang in gebonjourd want hij had gewoon niet genoeg steun meer. Hij vond zelf wel dat hij een hele actieve stafunctie had, maar hij had geen kracht meer in zijn benen, dus zijn knieën konden zomaar onder hem vandaan schieten. Opstaan van de wc was ook een groot probleem, daar had hij de kracht gewoon niet voor. Hij had een ziekte waardoor je spierweefsel wordt omgezet in vet. Dat verslapt allemaal, en hij heeft geen kracht meer over.
Dan doen jullie veel met de hand tillen?
Bij hem niet dus. Tillen doen we het liefst zo min mogelijk, zelf of met behulp van liften. Het duurt altijd erg lang voordat we eenmaal de grens over stappen om een apparaat in te zetten. Dat komt ook omdat mensen het liefst zo lang mogelijk hun eigen functies willen behouden. Zo lang mogelijk, want mensen willen zo lang mogelijk alles zelf willen blijven doen, met behulp van, terwijl het vaak toch een kwestie is van pluk- en trekwerk aan zo’n persoon. Bovendien moet je de techniek echt echt echt heel goed beheersen, wil je een mens op tillen. En als ze eenmaal bedlegerig worden, dan worden ze overgeplaatst naar een verpleegtehuis. En terminale cliënten blijven toch wel vaak. En dan heb je nog glijzeilen die je kunnen helpen.
Maar je probeert mensen zo min mogelijk te tillen terwijl ze zelf nog kunnen opstaan?
Ja, dat klopt. Verder kun je ook denken aan een sta-op stoel. Als mensen moeite hebben met opstaan uit een lagere stoel, dan is een sta-op stoel geschikt voor hun.
Ervaart u regelmatig klachten die veroorzaakt worden door het optillen van een persoon? Welke?
Nou, wel regelmatig rugklachten. We proberen daar wel iets aan te doen, om te overleggen met elkaar. “Hoe doe jij dat? Heb jij een makkelijkere manier?”
Hebben jullie dan allemaal een eigen manier van een cliënt helpen opstaan?
Nou nee, dat toch niet. We proberen daar toch wel een lijn in te trekken. Dat is ook heel erg afhankelijk van de persoon. Maar per persoon organiseren we wel een bijeenkomst om te overleggen hoe dat we die persoon het beste op kunnen tillen. Dat is voor de cliënt wel het fijnste, om het iedere keer hetzelfde te doen, hè. Dan weet hij ook wat hij te wachten staat, en hoe zij tegenover ons als verpleegkundigen staan. Want anders is de ene de goeie en de ander de kwaaie.
Oke, dus een cliënt kan angstig worden door het vooruitzicht om opgetild te worden door jullie of met behulp van een lift. Ervaart de cliënt geregeld irritatie door getild te worden? Hoe gaan jullie daar mee om?
Nou nee, ik denk niet zo zeer irritatie, maar een vorm van verlies, afscheid, weer een stap terug uit, dat is eigenlijk een rouwproces. Dat begint dan met autorijden, een heel groot stuk zelfstandigheid, je bent niet meer mobiel. Dan moet je altijd iemand opbellen, en bent niet meer onafhankelijk. Zo is het ook met opgetild worden. Het feit alleen al: ik krijg een prikkel: ik moet naar de wc. Dan sta je op en loop je naar de wc. Het idee dat je daar zit, en dat je denkt oh jee, mijn prikkel komt dat ik naar de wc moet, maarja dan moet ik weer eerst iemand gaan bellen, want er moet eerst iemand komen. Eigenlijk moet je die prikkel wel heel vroegtijdig voelen want anders dan kan ik het misschien wel niet ophouden en misschien zijn ze wel te laat. Dat zijn zoveel dingen veroorzaakt door die ene prikkel dat je moet gaan plassen. En het alternatief is zo’n ding in je broek.
Zijn er dan cliënten die jullie ieder moment van de dag kunnen opbellen om naar de wc te gaan?
Ja. Maar als je toevallig bij een ander staat en je bent die al aan het helpen, ben je een half uur te laat. Dan spelen er wel irritaties.
Hoe ga je hiermee om?
Je kunt dan alleen aangeven dat het nog een half uur gaat duren dat je er bent. Niet dat ze er rekening mee houden dat je er binnen 5 minuten bent. Soms kan dat wel, maar dat is maar net waar je mee bezig bent. Maar als je het aangeeft is dat minder erg. Als ze het maar weten. Maar we voelen allemaal met de cliënten mee. Als we onszelf in die situatie zien, dan denken we soms dat we er nog erger door geïrriteerd zouden zijn.
Verschilt het heel erg per persoon dat ze ongemak of angst ervaren bij het optillen? Of dat ze de voorkeur geven aan door jullie geholpen te worden of met behulp van de tillift?
Dat verschilt inderdaad heel erg per persoon, maar ze geven echt allemaal, stuk voor stuk, de voorkeur aan dat wij ze zelf helpen met opstaan.
En waarom is dat zo, denk je?
Ze hebben dan meer het gevoel dat ze zelf opstaan, en niet dat ze zich volledig moeten overgeven aan een apparaat. Daarbij komt dat ze ons meer vertrouwen dan een apparaat. Zoals we al eerder hebben gezegd: vertrouwen is het belangrijkst in de zorg.
Summary results interview
The lifting strategy as discussed with the caregivers of the RSZK is as follows. To lift someone out of bed a person hoist or a “turntable” can be used, but most times the clients are lifted by hand. The general experience that the nurses have with the clients with respect to the person hoist is that most people are afraid of these patient lifts. The reason is that people are seen as more trustworthy. However, this trust depends on the relation between the caregiver and the client. For example, if the client gets familiar with the caregiver he or she will trust the caregiver more easily. Giving clear instruction is also very important, as well as the enthusiasm with which the instruction is given.
There are stand-up lifting systems, but only people who have relatively good functioning standing capabilities and trust in that ability can use them for the client is not comforted when using it.
People want to be autonomous for as long as the can be. They will not like a tool because it means they can’t do certain things without help. If a caregiver helps with standing up it feels like you still do something, with technology this isn’t the case. It also doesn’t help that most people don’t like change. Sometimes demonstrating the “new” technology in form of a film will give more resistance towards it than just using the technology.
Caregiver can oftentimes not get to clients in time to help the clients get up. This gives rise to irritation
Methods for helping someone get up
Getting up from a sitting position (in order of the client having a lot to little power ):
- Hand on the back to give them the faith they can do this (caregiver hardily lifts)
Or
- Let the client grab the caregiver around the neck
- Caregiver puts knees against client’s knee
- Stand up together
Or
- Grab client around body and head
- Lift until they are upright
Sitting up from a lying position
- The care giver gives the client a hand and lifts them up
Or
- Grab shoulders and legs
- Turn them towards the edge of the bed and lift the shoulders at the same time
CCVSD values in the interview
Values in lifting by hand
The purpose of this chapter is to reflect upon the care practice of lifting by hand and with a mechanical lift from an ethical perspective, with the article of Van Wynsberghe in mind [5]. We will pinpoint the most important values in the act of lifting a person based on the interview done with the nurses of the nursing home RSZK in Reusel.
During the lifting process, trust plays an important role. Caregivers indicate that clients respond better to being lifted when they have already created a relationship with a client. According to numerous studies, trust facilitates cooperative behaviour[8] [9]. To be more concrete about this, let’s use the following example.
The client called mrs. Adams has to be taken out of bed every morning and helped back in in the evening. She is still relatively independent, as she can move around freely with some support provided by a cane or rollator. However, she needs help in the morning when rising from the bed and she needs to be be helped with medical stockings. Most of the day she spends seated, since she is weak in the legs. Therefore a caregiver comes in twice a day to provide her with these (and more) care tasks.
Mrs. Adams mostly receives care from caregivers that visit her regularly, i.e. twice or thrice a week. When such a caregiver visits her, she listens to the instructions carefully. The set of actions to be taken are the following.
The client starts in lying position, grabs the nurse around her neck, and is lifted to a sitting position on the edge of the bed. Then a break is held for half a minute. The next step is more complicated for both the caregiver and care receiver. The client puts her knees against those of the nurse. Then she is instructed to stand up with the guidance of the nurse.
The difference between a regular and a one-time visit from a caregiver is this: the client tends to listen closely to instructions and fully trusts the nurse that visits regularly. Whenever a new caregiver is sent to Mrs. Adams, she fails to stand up because of bad timing and wobbly knees in the last phase of standing up with help of a nurse. The cause is that she does not fully trust the new nurse yet, and tries to rely on her own strength instead of making use of the nurse’s. Henceforth, trust in a client-nurse relationship is very important and can be gained by social interaction[9]. Since establishing a bond with a client takes time, this is an essential factor in building this relationship as well.
When lifting a person, the feeling of safety also plays an important role. It is actually linked to the value of trust. In the interview is addressed that the feeling of being safe with a nurse builds to the client-nurse relationship.
One way to make a client feel safe is to put a hand on the lower back of the client when she is standing up partly on her own powers. On the one hand, touch ensures the nurse that the client is still there standing up and can feel when the client has lost balance. On the other hand, the client feels that the nurse still has the focus on her standing up and will catch her whenever she loses balance.
Another advantage of this method is the satisfaction of the client. A nurse tells that sometimes she even meets resistance from the client whenever she needs to be helped to stand up from the bed. The method to deal with this is to give initiative to the client and let her stand up at own will. Plus, she will be helped to stand up minimally. Whenever she has regained some strength, she needs minor support. To ensure that this strength does not collapse halfway through the standing up process, a hand is held on the lower back for protection against falling, but the client feels the independence while standing up at own initiative.
The resistance comes from the loss of independence, the caregivers agree. Metaphorically, a nurse tells it is actually a form of loss, farewell, a step backwards. In fact, it could be compared to the process of grieving. The first a client loses is being mobile. The driver’s licence is withdrawn, which causes being dependent on family, friends or taxi drivers. This is also the case with standing up. The fact that a client is dependent on a nurse to even get out of the bed after awakening is a great loss for a client, and sometimes even arises irritation. Therefore, the nursing home tries to make plannings in such a way that a client is visited daily by a regular set of nurses. A short explanation: these visits will be more sociable and clients tend to make chatter with the regular caregiver which causes distraction from the annoyance caused by the lifting.
Of course not every caregiver can visit daily, but since clients seem to prefer regularity in their schedule, the team of nurses discuss for each client which method of lifting will be used as a standard. This way, the nurses adapt the method of lifting specifically for each client and take into account the client's’ preferences and those of the nurses themselves. Thus, the nurses are more comfortable when lifting a client and have less discomfort from their back, neck and shoulders. This way, the value of comfort plays a centre role in the lifting practice.
Another advantage is that the client does not develop a preference solely based on the practice of lifting. By sticking to just one method of lifting per client, the client knows exactly what is ahead and the nurses also deduce their opinion towards them, while paying attention to their bodily behaviour and the way their instructions are followed.
These instructions are of great importance. They should not only be very clear but also be posed in a respectful and appreciative way. One nurse indicates that repetition is very important. When a client is elsewhere with her mind, the practice of standing up will most certainly fail. With great enthusiasm, instructions should be repeated often and be very clear. Sometimes it might seem as if a client is commanded as if he were a pet, which can be avoided by being enthusiastic and for example giving a high five for succeeding once again. Because of this playfulness, the clients feel appreciated and respected and the nurse-client bond is strengthened. This might feel contradictory, but the alternative is being over-serious and businesslike, which results in a client that feels as if he or she were merely a way of making money for the nurse.
Values currently not respected
The purpose of this section is to introduce the use of the passive person hoist and to determine exactly why such resistance is met against passive person hoists. Let’s first start with a scenario. Mr. Dirks is a male resident of RSZK Mariahof in Reusel. He lives independently and receives care in the morning and in the evening. He still has full body function but is weakened due to an illness that causes his muscles to convert to fatty tissue. Therefore, he is bound to a wheelchair all day long. The least of any resident of Mariahof, he expresses resistance against the passive person hoist. However, he uses it regularly and does not complain. His standing-up function is quite better than those of the other residents.
To move from a lying position into a sitting position, he needs the help from the caregiver. After that, while sitting at the edge of the bed, the nurse fetches the passive person hoist, prepares it for the client and steps to the other side to control the buttons. Therefore, no physical contact between the caregiver and the client is possible. This also holds for eye contact, since the caregiver’s attention is fully directed towards the controls of the machine. The performance of the person hoist is of great importance for gaining trust in the machine.[10]. Whenever the movements are not natural for the client, this might lead to distrust. Then it is difficult for a client to have confidence in the person hoist.
The support that is normally given by the nurse when the client is standing up, is now completely transferred to the passive person hoist. Thus, the client must have full confidence when using the passive person hoist, since he has no support from the nurse. The client must now rely on sound and instructions from the nurse.
The resistance that mr. Dirks expressed before couldn’t be lessened by a demonstration. A nurse tells that there are given demonstrations on a regular base at Mariahof, but most of the time, the residents really dislike the idea. The cause that mr. Dirks finally gave in to the passive person hoist, is because of necessity. His balance was more and more off, and it became dangerous to lift him by hand. First, he made use of an active person hoist, but he didn’t have the strength anymore in the legs, which could cause his legs to slip out under him.
According to the caregivers, the use of passive person hoists is delayed as much as possible. When finally the decision is made to use a person hoist daily, this is an absolute necessity, since the practice of lifting is done as least as possible. The team of nurses want the clients to keep their bodily functions as long as possible, since the clients themselves wish to be as independent as possible. For example, when a person has difficulty with rising from a low chair, they must consider purchasing a standing-up chair in order to stand up independently.
Furthermore, when a client expresses a preference of being helped to stand up with the help of a nurse, their wish is respected unless it is no longer possible. Until the passive person hoist is a must, the clients will be helped by hand.
Now the question arises why such a resistance is met by the clients. Let’s discuss a few topics that we have discussed together with the nurses, since they can most certainly empathize with their clients best. Plus, when a nurse-client bond is strong, the clients finally dare to express their true feelings about being lifted by hand and with a person hoist.
Trust can be gained by experience or establishing a bond. To trust in a machine is hard for people that are of age, since that generation has not grown up surrounded by technology. A person of age 20 will more easily trust that the construction of the person hoist will have no difficulty carrying their weight, whereas elderly people do not fully trust that no accident will happen. According to nurses, this might be because of the different contact points with the client. An extra hand in the back that actually does not play a physical but only psychological supportive role comforts clients when lifting by hand. A machine does not provide this extra attention for a client. Therefore, they prefer lifting by hand with help of nurses.
Fear of weakening is also given as a reason for clients to dislike being lifted with help of a machine. As we have just discussed, lifting by hand enables a client to use their full power and the nurse only has to supply extra help and support where needed. When using the machine, the clients do not have to use any strength at all and therefore might get the feeling that they cannot do anything themselves anymore. The next value is linked to this.
Independence is another very important value when it comes to the care practice of lifting a client. When being lifted with help of a nurse, the clients stands up at own initiative. When being lifted by a person hoist, the client takes a passive role and has to fully undergo being lifted and has no say in the process. Because the client doesn’t have to use any strength, they might even feel they are not capable of standing up themselves or they are not allowed to do anything anymore.
This is another loss in the eyes of the client. The nurses suspect that they feel inferior to other human beings that are fully functional and can move around freely. The care practice of being lifted with help of a nurse can be done in a very respectful manner, where human dignity plays an important role. The client’s wishes are very important and they are being dealt with with great respect. The warm and seemingly safe hands are very comforting for the client and make the client feel human. However, when being lifted with a person hoist, this might feel businesslike and disrespecting to a client, although the nurses do their best to treat the clients with great respect. The nurses that we have spoken to indicate that the lack of eye contact and the focus that goes to the controls of the apparatus contribute to the feeling of being treated disrespectfully. A study on eye contact in social interaction confirms this.[11]
We conclude that hands-on care is greatly preferred to the person hoist or other machines because of (amongst other) these aspects. Note that we only have access to a nursing home that is in possession of person hoists and not a RoBear, so we have laid our focus on the person hoist, but we can compare this to being lifted by any machine, amongst others the RoBear.
Improvements
New Values
In this chapter we will discuss the most important values in the care practice of lifting a client. The focus lays on the aspects that are definitely lacking in the act of being lifted by a machine compared to being assisted by a nurse. Since we only had access to a nursing home that uses person hoists on a daily base but does not own a RoBear, we use this technology as a basis and compare this to the functions of the RoBear. From this viewpoint, we define improvements to the RoBear based on the experiences of clients with person hoists. Note that we must fill in the gaps ourselves between the somewhat older technology of person hoists compared to the RoBear. However, we argue that the same problems hold to some extent for being lifted by any machine that operates quite similarly.
For any mechanical lift, the value that is at top priority is efficiency [5]. However, as we have seen in previous sections, for a client the following values should also be respected and can be improved upon. The first thing that we consider is lacking, is the trustworthiness. We want to improve the trust of the client in the RoBear, for example by extra contact points of the RoBear with the client. We have seen that an extra contact point in the lower back is comforting and relaxing for the client although it might not practically be needed in the lifting process.
Another way to solve this problem is a more natural way of lifting a client. Based on the position of the client’s body, the RoBear must formulate an action plan and lift the client accordingly. Then, the RoBear must be able to detect the position of the body of the client. This way, the RoBear will behave more natural and not scare the client or make the client feel dehumanized. Such a system is partially implemented in the “computer vision” subsection below. This leaves us at the next value.
Human dignity is an extremely important value in the act of lifting a person. We have seen that the client loses some independence when he needs help standing up. Then we must at least try to give the client the independence it can still have. One way of doing this, is to have eye contact with the client and treat him with great respect.[11] When a nurse is present, he or she should be able to do this and not be distracted by the controls of the RoBear. Therefore, we want the RoBear to perform a string of actions autonomously. Whenever we want the RoBear in a home setting without a nurse present, it has to be able to look into the client's eyes before or during the lifting process.
Furthermore, to give a client back some independence, he or she should be the one to take initiative before being lifted. Then, the Robear should behave according to the commands of the client. We aim for a RoBear that can give audiovisual feedback, in the form of full sentences or an interactive display for the client to use. With this user interface, the client should feel in control.[12]
Looking back at the paper of Van Wynsberghe [5], we have pinpointed those values that the RoBear does not yet fully respect. Furthermore, we have made suggestions on how the RoBear should be improved accordingly. In the following section will be dealt with an enhanced strategy of lifting in order to improve the autonomy of both the RoBear and the independence of the clients.
New Lifting Strategy
To improve both the autonomy of the RoBear and the feeling of autonomy of the care receivers, the RoBear should not only be able to lift a person all by itself, but also give the client the chance to help the RoBear in this process. Already when the person is getting seated from the bed, there are many differences between activeness and passiveness from them. To ensure the physical safety from a client, the RoBear should feel the amount of strength the client can still use himself to become seated, by using torque sensors in the arms helping the client get seated. If little power is needed, because the client can do much of the lifting himself, the RoBear should not keep pushing very hard and risk injuring the client, whereas when the client has little to no power, the RoBear can use a little bit more power.
The main lifting strategy, in the case where a client needs to go from laying down to sitting up in bed, is to first check the position of the body, using the cameras to be attached to the body of RoBear. Then the first arm is to be inserted under the neck of the client, while at the same time also giving the client the possibility wrap their arm around something, to give them the possibility to pull themselves up. This needs to happen in a soft and safe way, and thus the head and shoulders also need to be supported by the arm during the lift. When the upper body is lifted far enough, the second arm of RoBear can be inserted under the middle of the back, to give a bit more support to the client while sitting up. With this arm, the possibility of rolling off the grip of RoBear should be prevented, so the end should be tilted towards RoBear.
When the client is started sitting up, the knees need to be located by RoBear, using its cameras. Then the knees need to be lifted, which can be done using only a small arm. After a little bit of support is also given to the upper legs, the client can either be rotated towards the side of the bed and relieved from their leg support if they are able to stand up themselves, or be lifted off the bed if they can not. On the side of the bed, the clients are given a little rest, after which the rest of the lifting procedure is started.
For getting from seated to standing, the arms of the current RoBear can be used. The client will hold their arms on top of RoBears arms, and lift up from the bed, with help from RoBear. If possible, RoBear then slowly releases the client, to still give the client the satisfaction of standing up on their own. From the interviews, we got the note that a hand on the lower back is a very important part in getting a client to trust you. In this case however, as the RoBear is positioned in front of the client, a soft hand below the arm should suffice. Because this hand should not only be there to touch the client, but also to feel if the client is about to fall, very sensitive touch sensors are important here. If the now standing, or almost standing, client begins to fall, the RoBear should use its two soft arms to catch the client underneath the armpits.
Overall, the most important aspect is the safety of the client. That is also why the Robear should at all times keep his eyes on the position and movements of the client, to keep them from falling.
New Appearance of the RoBear
Now we have discussed the new lifting strategy as it will be executed by the RoBear, we will discuss the new features that should improve the RoBear. First of all, the RoBear should have a Computer Vision system, which entails the presence of two cameras and body position recognition software. Moreover, the RoBear should detect the body position and classify it in a set of body positions, call it a library. Then, it picks the set of actions belonging to this type of body position. Since this has been studied elaborately, we will discuss this in the next paragraph.
The Robear should also have a body roughly the size of a human, else it would not be able to carry a person or help him/her to stand up. The original robot was the face of a bear. The bear like appearance is better than a more humanlike appearance. The human form would imply that it is able to act and socialize like a person, which it can’t. Especially elderly people who have not seen comparable technology can get frustrated when the robot doesn’t act as expected. Another advantage of the bear like appearance is that it feels less like a human sees them in an “shameful” state.[13]Now it’s only a bear, bears don’t seem to judge based on social norms.
It is better that the robot looks like a bear, something they can recognize, than a robot. The more the robot deviates from a known for the more it will look like technology. For a lot of people technology is scary and unpredictable. Overall not something you would trust to help people get out of bed or even carry them.
Therefore the choice of two arms is most natural, as we want the RoBear to have the outward appearance of a bear. The lifting strategy is based on that of a human, therefore we will opt this for the RoBear. Furthermore, the RoBear is now designed with two arms, and we do not seek to change this when the alternatives have not proven to be better.
An alternative would be more than two arms or more general many more contact point. A suggestion would be a mattress-like structure, such as a bed that can be moved in any body position or a stand-up chair. Since those already exist, and there is still need for a nurse to come by and help the clients out of these furniture items, the original design of the Robear seems more suited. Furthermore the general goal was to make improvements to the RoBear. Since the robot can lift people with two arms it will remain designed that way.
Finally, when the RoBear will be introduced at people’s homes, the RoBear must be compact in size. A maximum width must be assigned, based on the width of a standard door. Moreover, the problem must be tackled that the RoBear is capable of moving across an uneven floor with thresholds or bumps.
Interaction
More features that could be improved will now be discussed, with the aim for the RoBear to interact more with the clients, which we refer to human-robot interaction. It has been shown that a good robot-human interaction can help clients willingness to use the robot and help build trust.[14] The first improvement that we would like to discuss is a user interface. To illustrate this: imagine a RoBear that has a touchscreen and built-in speakers and a microphone. For example, the screen could show the body detection of a person, or show a demonstration of the lifting process. This way the client can see what the RoBear is doing, which will help to understand how the robot works. The Robear will no longer be a mysterious piece of technology.
Moreover, the RoBear could play an audio fragment to tell a person what will happen. Especially clients with dementia could be helped by a continuous reminder throughout the lifting process of what they should be doing and what they could expect next.
Furthermore, emotion recognition could be implemented. With this function the robot can see if the client is in distress or otherwise tries to stop him. Optimally the RoBear would be able to stop the lifting process at that point, but even calling a nurse for help would be helpful.
Finally the RoBear could ask feedback when the process is done. This way the client feels like the robot takes them into account, the robot can adapt its general strategy and in an optimal situation it can adapt its lifting strategy on a personal level. For example if a client has a bad knee, the RoBear might avoid putting a force on that joint and instead try to place its arms elsewhere.
Computer Vision
Computer vision is already an important aspect of all our lives. When taking a selfie, your camera can automatically determine when you are smiling and take a picture accordingly. When going through customs to some countries, the passport scanner is automated and can detect and compare your face without need for human interaction. Until several years ago, many applications of computer vision were outside the capabilities of computers and smartphones. Nowadays, thanks to radical improvements in both hardware and implementation, basic tasks for computer vision (such as object recognition and event detection) are well within the reach of even the weakest smartphones and laptops. In order to provide a faster user experience, modern smartphones come equipped with VPU’s that handle vision-related tasks.
Improved computer vision has already very much improved the automation of simple tasks, such as quality assurance at factory conveyor belts. We believe that computer vision can not only improve the autonomy of these simple tasks, but also the autonomy of senior citizens during their daily lives. If the robear is equipped with cameras that allow it to do some scene reconstruction, it will be able to ride to the client’s bedside and determine if the client is ready for pick up autonomously. This would free up caregivers to focus on the clients themselves instead of the lifting process, and lift a heavy burden from their shoulders.
In robotics, computer vision is absolutely crucial for many steps in any decision-making process, from detecting the room and deciding what path to take (scenery reconstruction) to checking whether the ball to be lifted is actually getting off the table (event detection). However, computer vision as it is currently used in robotics is not very refined and often needs to be done in a high contrast situation (e.g. a football game where the field is green and the ball is bright orange) for it to work correctly. In the scenario we decided upon, this will not be the case. The client may be wearing any color of clothing, and it might not contrast very well to the color of the walls, ceiling and floor. This means we cannot rely on traditional methods like testing valley regions in gray-level images. Instead, we will use a very well trained neural network to do detection. Further on, we will introduce a second camera in order to do depth perception as well.
Pose detection on humans
Even with the advancements made in the last few years, full pose detection on humans has been a big hurdle. More traditional methods (for example, those bundled with OpenCV) have often focussed on detecting a general bounding box of a human or other object, others on using many hidden layers and a final softmax layer to determine the pose from a set of possibilities. On the CVPR (Computer Vision and Pattern Recognition) conference in 2016, the ‘best demo’ award was won by “Convolutional Pose Machines” by Shih-En Wei, Varun Ramakrishna, Takeo Kanade, Yaser Sheikh. Based on the released CPM from this demonstration, OpenPose was developed. OpenPose is a library for exact pose detection on humans, and the network used is fast enough for a medium-power laptop to do real-time pose estimation. This does require the input images to be rescaled down to only small fractions of the original size.
Disparity mapping
OpenPose’s output is a list of all the detected features and their locations within the input image. This is already a big leap, but cannot yet be used for full reconstruction as a dimension is still missing: depth. It it possible to do some estimation of how far away a person is based on only two dimensional images, for example by knowing the size of certain features (such as the distance between the shoulders and hips) and assuming the person is always in a certain pose with respect to the camera. These are, however, too many assumptions for the task at hand. In order to accurately determine the distance to objects using two dimensional images, a second camera and a way of determining the new data is needed.
The first was relatively easy, two cheap pinhole webcams of type “TRUST Webcam” were bought, the PCB’s and lenses removed and placed within a wooden support structure. The final result is displayed in the image below. This newly fabricated stereoscopic camera gives two 640x480 images at 30 frames per second, with some noticeable delay. It is noted that the budget for cameras on the actual RoBear is (or must be) at least an order of magnitude higher, as the difference in the delay between the cameras is already noticeable even without determining actual distance values from it. It is suspected that this delay will have very little influence as long as the target is not moving.
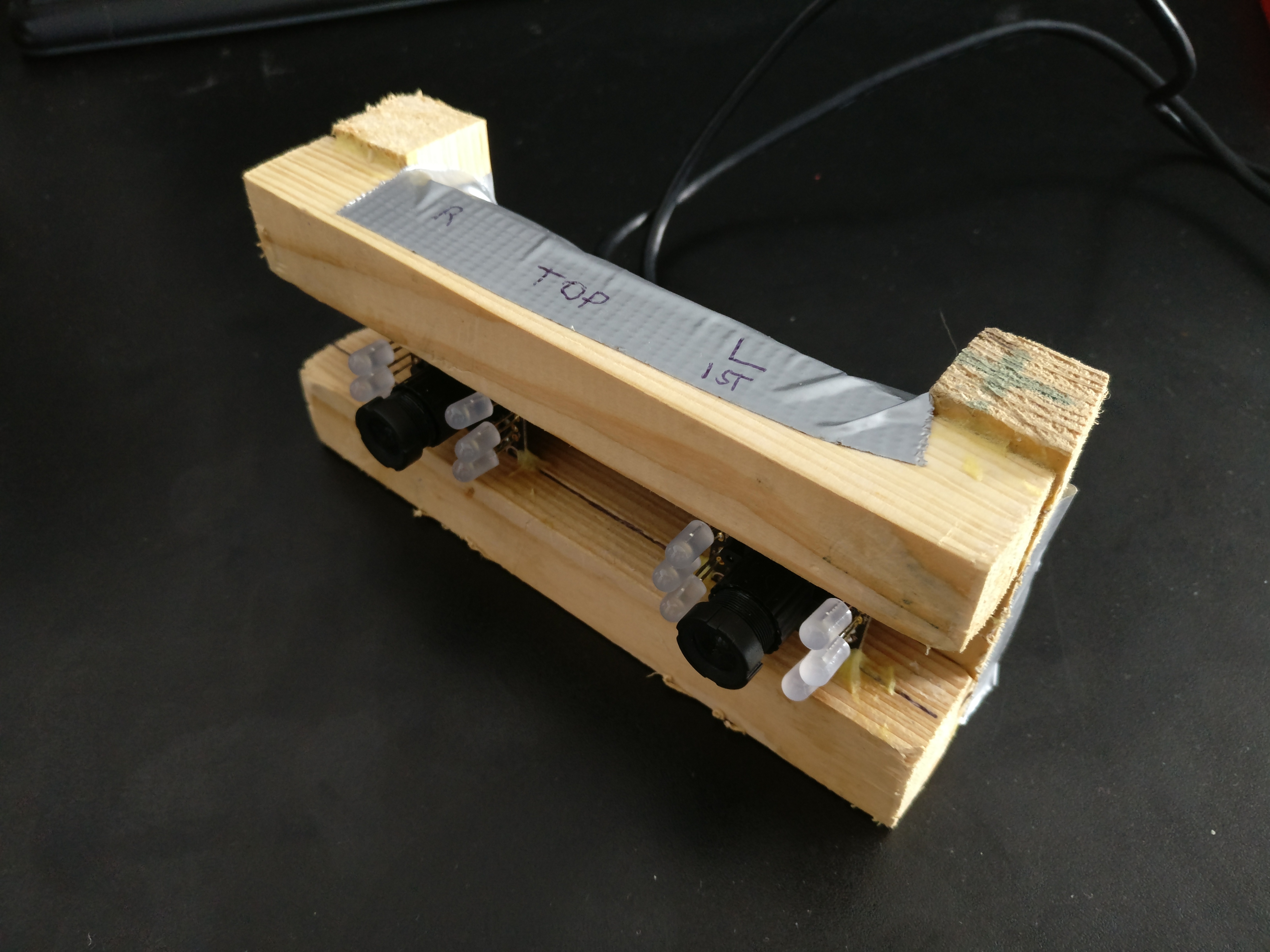
For the second problem, three different strategies were determined. All three are based on calculating the disparity (in pixels) between the left and right channel images. This disparity has a certain relation to the actual distance that can be determined and calibrated at a later point. The first method was to use OpenCV’s native StrereoSMBG method. Unfortunately, even after rigorous tweaking it was found that this method introduces a lot of noise and is computationally a lot more expensive than is needed for our purposes.
The second is to simply run the OpenPose network on both the left and right images and calculate the disparity based on where the network detects each of the eighteen features in both of the images. It was found that again, this method introduces a lot of noise (the network detects the features with a certain uncertainty, and the actual detected points wiggle a lot in some situations) and is again too computationally expensive.
The third and final solution would be to detect each point in one of the images (for example the left channel), then take a small area around each of the (subset of the-) eighteen detected points and correlate them with the other (i.e. right) channel. This was found to be the best method, introducing the least noise and being much less expensive than the other methods.
For the correlation, OpenCV’s native CV_TM_CCOEFF_NORMED algorithm was used separately on all color channels and then summed. The coordinates of the maximum of the resulting 2d-map is assumed to be the location of the detected feature in the other channel. The difference in the x-coordinates between the same features in both channels is the disparity and can be used to determine the distance to the detected feature.
Scene reconstruction
In a perfect world (or with a more expensive stereoscopic camera), the disparity ranges The setup of the camera’s is not perfect and the angle between their optical axes is very much non-zero. This makes the (simple) mathematical interpretation of the disparity quite useless, but we can still calibrate the disparity to match with distances. We find a relation of
[math]\displaystyle{ -x = \dfrac{0.0486149 \cdot d+64.0587}{51.9407+d} }[/math]
Where x is the distance and d is the disparity in meters and pixels, respectively.
The OpenPose library detects each of the eighteen features separately, and contains native code that classifies each feature as belonging to a certain person. This is usually quite accurate, but can fail if people are standing close together in positions where not all features are visible. As this is usually not the case in the lifting-from-bed scenario as we can place the cameras in such a position that all features of the client being lifted are accounted for, we can assume that this will work fairly well in our scenario. The final output of our software layer on top of OpenPose is given in the figure below. Code is available upon request.
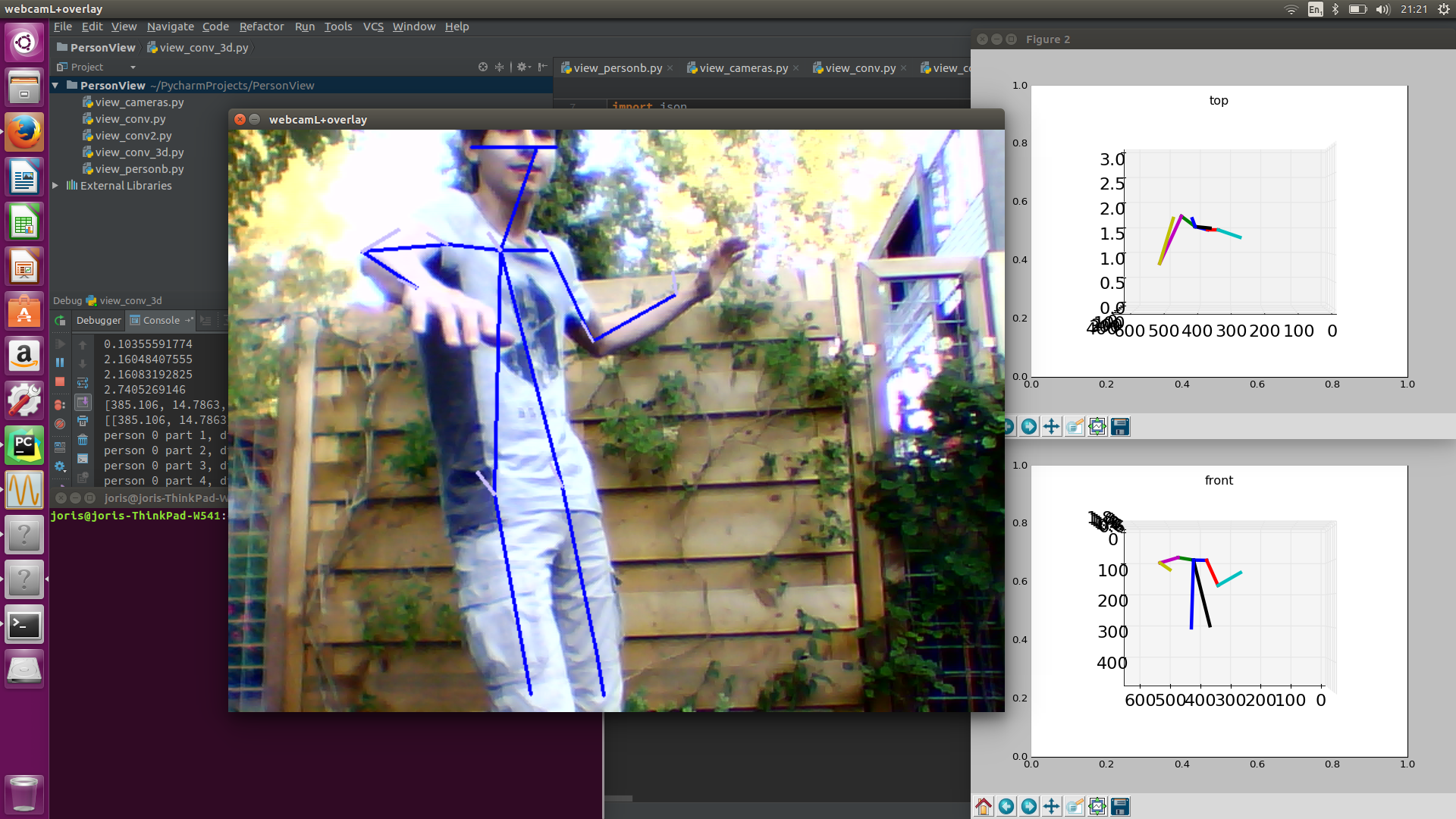
Interpretation by the robot
One of the main problems that have to be solved mainly by using computer vision is not only detecting where the person is, but also driving towards the person, deciding whether or not the person is in a viable pick-up position (and possibly instructing them on how to get into such a position from their current position), and moving the arms around the client’s shoulders and or back/neck. From that point out, most of the sensory work will be done by the torque sensors in the joints of the robot. One of the reasons the camera’s we use for the detections of the client are in the robot and not fixed to the room - which can in some situations be cheaper and would also allow the system to track the absolute position of the RoBear - is this very point. Affixing the stereoscopic camera to the robot would allow it to use a relatively simple decision system to determine whether the client is in a position that allows for pick-up, based on only relatively simple parameters like the angle between certain joints or the angle between the back and the horizon. These parameters could be based on our lifting strategy. We have not focussed on actually creating such a decision method.
Implementation
When a client needs to be lifted, it is important that they know exactly what needs to be done by them and what is going to be done with them. RoBear should thus be able to communicate by speech to the client. To give the client a feeling of trust in RoBear, and to keep their dignity up, these instructions should be given in a friendly manner, and not in a commanding way. Doing otherwise will result in the client not acting to their full potential, and maybe hurting themselves.
Furthermore, for the client to get a real sense of control, they should be able to give commands or suggestions to the RoBear. The easiest and most available way for doing this is by using voice commands. This means that the RoBear should have a microphone built in, and also an algorithm to detect certain commands. Commands such as stop and wait for instance are easy ways to detect stress or discomfort in people, and give the RoBear more ways to check if it needs to stop, go back or speak to the client. Also, there should be commands with which clients are able to call for the RoBear and tell him what he wants to do, and what kind of help he needs.
As specified above, the RoBear would need force, position and torque sensors to feel the amount of power a client can still produce by himself and the amount of help they need from RoBear. These sensors would be situated in the joints of the arms of Robear, measuring both the direction and the force that the client excerpts onto the arms of the Robear, so that if the client pushes back onto the arms the RoBear does not push further and injure the client in any way. Because of these sensors, the RoBear can deliver client-cooperative lifting, not only acting as a way of lifting, but also helping in a way to rehabilitate the client with lifting himself, or keep them able to lift themselves in this case.[15]
Conclusion
The goal of this project was to make improvements on the RoBear. It was shown that the robot doesn’t act trustworthy and lifts people in a dehumanizing way. Furthermore to use the robot a nurse needs to do a lot of work. The lifting can only start when the client is in a position most elderly cannot reach by themselves. To solve the first problem the robot will adopt a more natural way to lift clients. The solution described in “New lifting strategy” is one that nurses use now. This was concluded in the interview. This strategy is better because clients feel they are more in control. Another new aspect is that the robot will now also give audible feedback, encouragement and explanation about what will happen next.
To help the nurses a program was made that detects the way the client is lying. That way even if the client isn’t in the exact right position the robot will still be able to find the point where it should lift. Computer vision makes this possible, through this the robot will be able to identify the joints and the position of the client. It also enables the robot to look in the client’s eyes before doing something, this feels more like natural interaction and might comfort the client. When the suggested improvements would be implemented in the RoBear it would be more practical and less scary to use. It is a step in the direction of giving clients their independence back. Unfortunately the goal of a robot that could lift people without supervision was not met.
Discussion
Before the RoBear can be used there are a lot of improvements that need to be made. Seeing that this is only an eight week long project, the original goal of the client being able and willing to use the robot for lifting without help of a caregiver was too ambitious. This is why the project only focused on a subset of RoBear’s flaws.
It also means that there was no way to test if this is actually a better design. The only information this project is based on are older papers and an interview with nurses that care for elderly on a daily basis. These papers are based on similar robots but there might be factors that were not taken into account when applying the theory to the RoBear.
If there was more time available for this project, a few more things could be looked into; first of all, the clients and their next of kins could be interviewed on their opinion on the project and what they expected from it. Based on their answers, the design could be reevaluated. Also, a prototype of the improved RoBear could be constructed and tested by all users.
References
- ↑ http://techliveinfo.com/giant-robear-nurse-to-cuddle-lift-you/
- ↑ Spears, Tim (feb 26, 2015), http://www.designboom.com/technology/riken-robear-robot-nursing-care-02-26-2015, RIKEN's ROBEAR robot assists nurses when caring for their patients/
- ↑ Wilkinson, J. (2015, Februari 23), http://www.riken.jp/en/pr/press/2015/20150223_2/ The strong robot with the gentle touch, Retrieved june 03
- ↑ Byford, Sam (April 28, 2015), https://www.theverge.com/2015/4/28/8507049/robear-robot-bear-japan-elderly, This cuddly Japanese robot bear could be the future of elderly care
- ↑ 5.0 5.1 5.2 5.3 Van Wynsberghe, A. (2013). Designing robots for care: Care centered value-sensitive design. Science and engineering ethics, 19(2), 407-433.
- ↑ Boyce, C., & Neale, P. (2006). Conducting in-depth interviews: A guide for designing and conducting in-depth interviews for evaluation input
- ↑ http://www.rszk.nl/wonen/rszk-mariahof
- ↑ Eardley, A. (Ed.). (2010). Innovative Knowledge Management: Concepts for Organizational Creativity and Collaborative Design: Concepts for Organizational Creativity and Collaborative Design. IGI Global.
- ↑ 9.0 9.1 Feigenberg, B., Field, E., & Pande, R. (2009). Do social interactions facilitate cooperative behavior? Evidence from a group lending experiment in India. Mimeo.
- ↑ Cuijpers, R., & IJsselsteijn, W. (2014). Role inconsistencies in elderly care robots.
- ↑ 11.0 11.1 Bohannon, L. S., Herbert, A. M., Pelz, J. B., & Rantanen, E. M. (2013). Eye contact and video-mediated communication: A review. Displays, 34(2), 177-185.
- ↑ Tidoni, E., Gergondet, P., Kheddar, A., & Aglioti, S. M. (2014). Audio-visual feedback improves the BCI performance in the navigational control of a humanoid robot. Frontiers in neurorobotics, 8.
- ↑ Kahn Jr, P. H., Ishiguro, H., Friedman, B., Kanda, T., Freier, N. G., Severson, R. L., & Miller, J. (2007). What is a Human?: Toward psychological benchmarks in the field of human–robot interaction. Interaction Studies, 8(3), 363-390.
- ↑ Dautenhahn, K. (2007). Socially intelligent robots: dimensions of human–robot interaction. Philosophical Transactions of the Royal Society of London B: Biological Sciences, 362(1480), 679-704.
- ↑ Nef, T., Mihelj, M., & Riener, R. (2007). ARMin: a robot for patient-cooperative arm therapy. Medical & biological engineering & computing, 45(9), 887-900.