PRE2016 3 Groep14: Difference between revisions
No edit summary |
|||
| Line 58: | Line 58: | ||
The respiration rate of a person is simply said the amount of breaths per minute. This rate can tell a lot about people’s health in general, and it can also be linked to heart failure. A study found that the average respiratory rate increased in the week leading up to patient with heart failure requiring to be hospitalised. [7] | The respiration rate of a person is simply said the amount of breaths per minute. This rate can tell a lot about people’s health in general, and it can also be linked to heart failure. A study found that the average respiratory rate increased in the week leading up to patient with heart failure requiring to be hospitalised. [7] | ||
This respiratory rate can for example be measured with a respiratory inductive plethysmography (RIP). This setup consists of two sensors, placed at the ribcage and abdomen accompanied by electronics that process the signals. The measurements work on the fact that the inductances of the sensors change, depending on the cross-sectional area of the ribcage and abdomen, related to inhaling and exhaling. These have been developing over the years and already are capable of being worked into clothing. | This respiratory rate can for example be measured with a respiratory inductive plethysmography (RIP). This setup consists of two sensors, placed at the ribcage and abdomen accompanied by electronics that process the signals. The measurements work on the fact that the inductances of the sensors change, depending on the cross-sectional area of the ribcage and abdomen, related to inhaling and exhaling. These have been developing over the years and already are capable of being worked into clothing. | ||
=== Types of heart sensors= === | |||
==== Smart watch ==== | |||
The smart watch uses an optical LED light source and sensor to measure the beats per minute. This LED light sensor measures the amount of LED light that reflects back due to the passing red blood cells. The amount of light reflections depends on the number of blood cells passing through, which is more when there is a heartbeat. | |||
According to the official Samsung website, the heart sensor is only to advise the user of his overall health. It can help you with exercise, so that the user knows if the exercise is intense enough, but also if the resting procedure is according to the health standards. | |||
One disadvantage is that the sensor can be afflicted by factors as environmental conditions, types of skin and placement on the skin. The best way to wear the heart sensor is right behind the wrist (see figure…). Also, it cannot tell what your physical health is. It can only advise the user in his health. Also it cannot track any diseases on the heart or in blood vines. For example Samsung clearly states that the heart sensor is not a medical device, but is only used to keep track of your exercises. | |||
[[File:Example.jpg]] | |||
Another disadvantage is that you need to sit still when measuring the heartbeat. Thus when the user is taking a walk, the heart sensor is not able to measure the heartbeat. | |||
For people with a pacemaker the heart sensor can be very dangerous. The heart sensor of the watch can interfere the signal used with the pacemaker. In that case the pacemaker can stop working, or does not function properly. Therefore it is advised to keep the sensor at least six inches away from the pacemaker. [http://www.samsung.com/us/heartratesensor/]. | |||
==== Waist band ==== | |||
A heart sensor can also be implemented in a waist band. Most of the waist bands work with electrodes that measure the heart beat on the chest. A waist band is more accurate than a wrist band, as it uses a better technique and is closer to the heart. Still the sensor cannot keep track of your health, but is only to keep track of your exercise. One difference with some of the waist sensors is that it can be tracked with the phone via Bluetooth. This is easily done with an app that can be downloaded, in which the user can see the beats per minute and even the heart signal. Further it can have the same disadvantages as the smart watch. | |||
==== The National Instruments myDAQ ==== | |||
This setup is used at the course 5XEA0: Spectrum of electrical engineering, care and cure lab. This heartbeat sensor also uses electrodes. These electrodes are coupled to both wrists and one ankle. These electrodes are coupled to the myDAQ, in which it passes a high- and low-pass filter (se figure…). | |||
[[File:Example.jpg]] | |||
With the help of software, the received signal can be filtered to give an exact graph of the heartbeat (see figure…). | |||
[[File:Example.jpg]] | |||
There are some disadvantages to this system. The processing unit is too big to wear, and thus is not easily implemented to the body. Also, the unit needs to be connected to the computer by cable, which is not desirable. | |||
== Heart problems [http://www.hartwijzer.nl/ECG.php]== | == Heart problems [http://www.hartwijzer.nl/ECG.php]== | ||
Revision as of 13:13, 26 March 2017
This is the project page of group 14. Initially, this group was mostly focussed on developing smart home technology for elderly people, while keeping the needs and wished of these people in mind. Because this subject was very broad, it evolved into smart technology for just monitoring people's health by measuring their heartbeat. The group wants to ask elderly people for their preferences and then develop a simple prototype of this smart monitoring system.
Group members
- Jeffrey Baijens
- Margot Emke
- Jari van Ewijk
- Marjolijn Kleijer
- Bram Lustenhouwer
- Wouter Wolthuis
Introduction
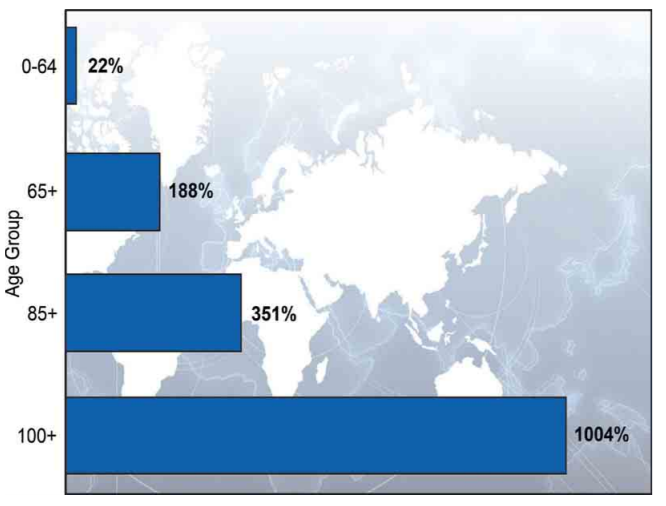
According to the Global Health and Aging report, by the World Health Organization (WHO), the world population is growing and the age composition of the world population is changing over the years. This causes an increase in the amount of elderly, which can be seen in Figure 1. The increase is mainly caused by the “baby boom” between the years 1946 and 1964 in combination with the rising life expectancy within the older population itself.
With the population ageing, there are expected challenges to our health care system. Future shortages of healthcare workers and lack of the diversity of their professions is likely. To be able to manage the increasing demand for healthcare, new models of care will be required. One of the possible solutions is to develop a "smart heart", which observes the heart of an elderly and alarms care givers, family or someone else when something goes wrong with the heart.
Our goal
The goal of our project to build an interface for the application of a smart heart. First, it is important to determine what the needs of the elderly and care givers are.To determine what the elderly and care givers want, a literature research will be done and a questionnaire will be taken. After the questionnaire, the results will be processed and discussed, where after decisions can be made about the design of the user interface.
Measuring the heart
State-of-the-Art
Types of heart measurements [2]
In this wiki, it will be discussed how certain measurements of the heart can detect serious heart problems and failures, as well as certain state-of-the-art devices that can continuously perform these measurements in someone’s daily life. Before going into these topics, a number of the most common or promising types of heart measurements will be discussed, so that these can be referred to further into the wiki.
Electrocardiography:
Electrocardiographs, abbreviated with ECG, and sometimes EKG, are a type of heart monitoring that can measure the electrical activity of the heart. With ECGs, the presence of deviations to the arteries surrounding the heart, disordered heart rhythms, and other types of heart failures can be discovered. This will also be discussed in the next section.
Figure 2: A picture of an electrocardiogram with its stages named. [5]
ECGs are performed by connecting certain wet silver/silver-chloride (Ag/AgCl) electrodes to the body, that measure the differences in electrical charges on the skin, that come as a result from the electrical activity from the heart. A problem is that moving other muscles also causes electrical changes on the skin, which makes continuous monitoring in someone’s daily life more difficult. Over time, however, electrodes have been developed that apply signal amplification, filtering and noise reduction, so that ECGs can be used for wearable health monitoring. A number of these ‘active’ electrodes have already been developed. [3] The requirement of the aforementioned wet electrodes brings a number of downsides. For one, these contacts can cause skin irritation. Secondly, the measured signal becomes less readable over time as these electrodes dry up. To counter these issues, electrodes that can be put on top of clothing and dry electrodes have been developed, respectively.
Photoplethysmogram:
Photoplethysmograms (PPGs) are graphs depicting measurements on the volume of an organ, such as blood vessels. With these graphs, changes in the blood volume can be measured. This can be used to monitor blood oxygen saturation, blood pressure and the amount of blood the heart pumps with every beat. PPGs are made using a light emitter, usually a light emitting diode (LED) and a light detector, usually a photodiode. Light is shone onto a person’s skin and either the reflection of this light, or the light that passes through gets examined. Such measurements can be performed on fingertips, toes, ears and noses. The main issue and advancement for PPGs in wearable technologies is that LEDs require a high power consumption. The advancement is a photodiode that is shaped like a ring, capturing more of the light emitted by the LED and therefore requiring less light and power from the LED [4]
Figure 3: This illustration depicts a PPG sensor, consisting of LEDs and ring-shaped photodiodes. The electronics are composed of a part for signal processing, wireless radio communication and a coin cell battery that lasts for a week. [4]
Blood pressure measurements:
Another way with which blood pressure is normally measured, is with the use of a sphygmomanometer. These measure blood pressure by inflating a cuff to close an artery and release it again, monitoring at what point the blood flows again. Such a device would be immensely uncomfortable for continuous health monitoring, although they are used at times for a day for patients of cardiovascular disease. For long-term monitoring, they are deemed too unpractical however. An alternative that was found when a relation was discovered in the delay between the R-peak from an ECG (figure 2) and the peak of a PPG. This relation, called pulse transit time (PTT) is displayed in figure 4.
Figure 4: A picture of an electrocardiogram and photoplethysmogram with the pulse transit time displayed in red. [2]
This relationship means that blood pressure can be estimated from the measurements of the ECG and PPG, and therefore do not require undesirable use of unpleasant cuffs being regularly inflated. This method is most likely paramount for blood pressure measurements in wearable technologies in the near future, but is still being developed. This PTT is highly individual and different methods for this estimation are still being researched. Methods such as estimating it with ECG, continuous wave radar and bio impedance. [6]
Respiration rate measurements:
The respiration rate of a person is simply said the amount of breaths per minute. This rate can tell a lot about people’s health in general, and it can also be linked to heart failure. A study found that the average respiratory rate increased in the week leading up to patient with heart failure requiring to be hospitalised. [7] This respiratory rate can for example be measured with a respiratory inductive plethysmography (RIP). This setup consists of two sensors, placed at the ribcage and abdomen accompanied by electronics that process the signals. The measurements work on the fact that the inductances of the sensors change, depending on the cross-sectional area of the ribcage and abdomen, related to inhaling and exhaling. These have been developing over the years and already are capable of being worked into clothing.
Types of heart sensors=
Smart watch
The smart watch uses an optical LED light source and sensor to measure the beats per minute. This LED light sensor measures the amount of LED light that reflects back due to the passing red blood cells. The amount of light reflections depends on the number of blood cells passing through, which is more when there is a heartbeat. According to the official Samsung website, the heart sensor is only to advise the user of his overall health. It can help you with exercise, so that the user knows if the exercise is intense enough, but also if the resting procedure is according to the health standards. One disadvantage is that the sensor can be afflicted by factors as environmental conditions, types of skin and placement on the skin. The best way to wear the heart sensor is right behind the wrist (see figure…). Also, it cannot tell what your physical health is. It can only advise the user in his health. Also it cannot track any diseases on the heart or in blood vines. For example Samsung clearly states that the heart sensor is not a medical device, but is only used to keep track of your exercises.
 Another disadvantage is that you need to sit still when measuring the heartbeat. Thus when the user is taking a walk, the heart sensor is not able to measure the heartbeat.
For people with a pacemaker the heart sensor can be very dangerous. The heart sensor of the watch can interfere the signal used with the pacemaker. In that case the pacemaker can stop working, or does not function properly. Therefore it is advised to keep the sensor at least six inches away from the pacemaker. [1].
Another disadvantage is that you need to sit still when measuring the heartbeat. Thus when the user is taking a walk, the heart sensor is not able to measure the heartbeat.
For people with a pacemaker the heart sensor can be very dangerous. The heart sensor of the watch can interfere the signal used with the pacemaker. In that case the pacemaker can stop working, or does not function properly. Therefore it is advised to keep the sensor at least six inches away from the pacemaker. [1].
Waist band
A heart sensor can also be implemented in a waist band. Most of the waist bands work with electrodes that measure the heart beat on the chest. A waist band is more accurate than a wrist band, as it uses a better technique and is closer to the heart. Still the sensor cannot keep track of your health, but is only to keep track of your exercise. One difference with some of the waist sensors is that it can be tracked with the phone via Bluetooth. This is easily done with an app that can be downloaded, in which the user can see the beats per minute and even the heart signal. Further it can have the same disadvantages as the smart watch.
The National Instruments myDAQ
This setup is used at the course 5XEA0: Spectrum of electrical engineering, care and cure lab. This heartbeat sensor also uses electrodes. These electrodes are coupled to both wrists and one ankle. These electrodes are coupled to the myDAQ, in which it passes a high- and low-pass filter (se figure…).
With the help of software, the received signal can be filtered to give an exact graph of the heartbeat (see figure…).
There are some disadvantages to this system. The processing unit is too big to wear, and thus is not easily implemented to the body. Also, the unit needs to be connected to the computer by cable, which is not desirable.
Heart problems [2]
Heart attack
With a heart attack, there is accute danger of life. Especially, lack of oxygen to the brains is causing problems. After only 4 to 6 minutes, brain cells become irreversibly damaged. After that, the other organs can get damaged too.
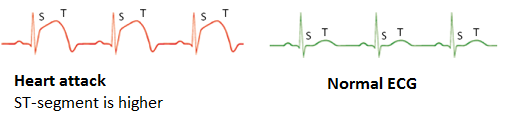
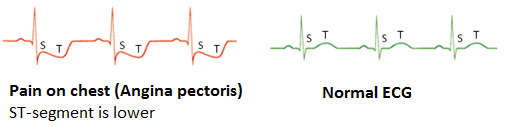
A heart attack can immediately be recognised on an Electrocardiography (ECG), by a deviation in the ST-segment of the ECG. During a heart attack, this segment is higher than normally.
Cardiac arrythmia
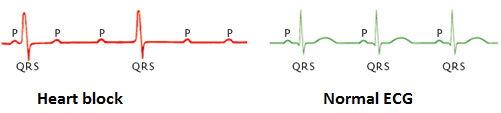
A cardiac arrhytmia is a deviation in the cardiac conduction system, a small electric network that controls the pinch of the heart muscle. There exist a lot of different kinds of a cardiac arrythmia. They can affect the pumping force of the heart, but they are fairly harmless.
An example of a cardiac arrhytmia is a heart block.
Pain on chest
Pain on the chest can be caused by heart failures.
USE aspects
The USE-aspects of a smart heart for elderly are discussed here:
- With a smart heart, more elderly can be saved because of more supervision on heart functions.
- Because of a smart heart, care givers get more time to focus on other tasks then just checking on elderly with heart problems.
- When care givers get more time, they are able to care more elderly. Therefore, family and friends do not have to take care of the elderly anymore, which is an advantage for the society.
- Through the smart heart for elderly a new market is created, which focusses on new monitoring devices, etc. Thereby, new jobs and companies can be developed, which is an advantage for enterprise.
User needs
(?) --> can be adjusted after the results of the questionary
Primary users:
The elderly:
- Should be able to press an alarm button themselves. (?)
- Need a display of their ECG themsleves. (?)
Secondary users:
The care givers:
- Need to be alarmed, within ..... seconds, when there is a cardiac arrythmia.
- Need to be able to alarm people, within ... seconds, in the neighbourhood of the elderly, who are qualified to reanimate.
- Need a screen, which constantly shows the ECG of the elderly or which shows the ECG only when there is a cardiac arrythmia. (?)
The family and friends of the elderly:
- Need to be alarmed, when...........
Tertiary users:
Heart specialists, people that can perform CPR, neighbors of the elderly:
Advantages and disadvantages
Advantages:
- Distance monitoring: With the help of a heart sensor, the elderly can be monitored from a distance. This can improve the living quality of elderly and will make home rehabilitation possible. When there is a heart attack or a raised heart rate, a doctor or the ambulance can be called immediately, giving higher survival rate and the person in need is helped a lot quicker.
- Feeling of safety: when wearing a heart sensor at all time, elderly will feel a lot safer. This is due to the fact that the wearer will know that help will come immediately when he or she has a heart attack. This safety feeling can help with the decision whether or not to move to an elderly house.
- Disease check: With the heart sensor, heart diseases can be checked from a distance. In this way a lot of hospital visits can be cancelled. When a heart disease is monitored by the heart sensor, then the elderly can make a visit to the hospital.
- Economy: With this technology, a new market can be started. Companies will invest in this technology and will possibly gain profit from the heart sensor. In that way the companies can invest in more technologies or can improve the privacy and the security of the heart sensor.
Disadvantages:
- Hackable: the heart sensor will be connected to the internet or Bluetooth at all time. In this way, the heart sensor can be hacked, which allows hackers to gain private data from the elderly. This can be solved by applying extra data security, but that will cost more money.
- high price: as with most of the medical machines that can be used, the heart sensor will be expensive. Therefore, the heart sensor will only be available for the upper class of society. A way to solve this is to let the insurance company pay for the heart sensor. But as in most of the cases, insurance companies only allow the money when medicine of medical appliances are needed.
- Privacy: as with all appliances that are connected to the internet, privacy of the user can be at stake. This can withdraw people for buying a heart sensor.
Prototype
One of the goals of this project is to deliver a prototype of the proposed design. However, considering the limited time, it will be a simplified version of the design to showcase what it is supposed to do. The prototype will consist of a sensor that the primary user carries with them, a server that processes the data and an application to control the system, with different interfaces for the different users. The “brains” behind the prototype will be a Raspberry Pi, acting as a kind of server that receives inputs from the sensor, processes this input and takes the right actions. That a Raspberry Pi would be used as the backbone of the prototype was chosen well before the survey was even carried out. It is a very flexible device that can basically do anything a normal personal computer or server can do, while also being fairly inexpensive.
The result of the survey could be that the primary user (the elderly) would like to have full control over the system and the data it collects and sends to others, in that case a local “processing unit” would be preferred. However, it might be easier to send all data to a data center and process it for all patients, maybe even training the system with all this data it receives. However, no matter the outcome of the survey, our first prototype will be created with the Raspberry Pi as the local processing unit. This gives more flexibility to showcase the main ideas behind our proposed design, without already worrying about every detail in this first prototype.
The control application will be a web-based application, because again this allows most flexibility. A fully-fledged native application for a particular platform (Android, iOS, Windows, or maybe even a custom platform) would require more time and this approach again allows for a more flexible prototype which can easily be extended during the development, while still being able to showcase the main ideas of the design.
Survey
In order to gain proper information in what elderly think of the heart sensor, a survey is held under elderly and care takers. The survey can be found underneath (the survey is in dutch, as it is held under dutch citizens):
1. Bent u verzorger of oudere?
- Verzorger
- Oudere
2. Wat is uw geslacht?
- Man
- Vrouw
3. Wat is uw leeftijd?
Deze enquete gaat over een slimme hartslagmeter. Deze hartslagmeter kan in uw kleding zitten, pacemaker (als u die heeft) of in uw horloge. De komende vragen hebben betrekking op functies die kunnen worden geïmplementeerd in de hartslagmater. Bent u een verzorger, ga dan door naar vraag 17.
4. Heeft u last van hartklachten, of heeft u een pacemaker?
5. Bent u geïnteresseerd in het meten en zien van uw eigen hartslag en waarom?
6. Hoe zou u het vinden als er een hartslagmeter continu uw hartslag in de gaten kan houden?
7. Zou u het fijner vinden als deze hartslagmeter gelijk hulp belt wanneer er geconstateerd wordt dat dit nodig is?
8. Wilt u ook een functie hebben op de hartslagmeter om hulp op te roepen wanneer u zich niet lekker voelt?
9. Zou u langer thuis blijven wonen of hebben gewoond als u een slimme hartslagmeter zou hebben?
10. Zou u eerder alleen uit huis gaan wanneer u een slimme hartslagmeter om zou hebben (om bijvoorbeeld boodschappen te doen of om een wandeling te maken)?
11. Zal u zich veiliger voelen wanneer er met een hartslagmeter continu uw hartslag in de gaten wordt gehouden?
12. Zal u het toestaan voor uw verzorger, thuiszorghulp of familie om van een afstand uw gezondheid in de gaten te houden?
13. Zou u zich er fijner bij voelen wanneer uw verzorger, thuishulp of familie alleen een signaal binnen krijgt wanneer er een afwijking is in uw hartslag, in plaats van een signaal wat ze altijd binnen krijgen?
14. Wilt u zelf controle houden over de hartslagmeter, bijvoorbeeld wanneer hij wel een signaal moet doorgeven en wanneer niet?
15. Wanneer er onregelmatigheden plaats vinden in uw hartslag, vindt u het dan fijn als uw familie automatisch gealarmeerd wordt of niet?
16. Heeft U nog overige opmerkingen of ideeën? De komende vragen zijn alleen voor verzorgers. Bent U een oudere, dan kunt U hier stoppen met deze enquete.
17. Wat vindt u van de technologie dat ouderen met een slimme hartmeter rondlopen?
18. Denkt u dat met deze technologie ouderen langer zelfstandig thuis kunnen blijven wonen?
19. Denkt u dat deze technologie een bijdrage heeft aan de veiligheid van de ouderen?
20. Met deze hartslagmeter is het ook mogelijk dat u de hartslag kunt checken. Heeft u dan de voorkeur om deze constant te kunnen bekijken of alleen wanneer er afwijkingen ontstaan in de hartslag?
21. Via welke apparaten wilt u de hartslag kunnen meten?
22. Denkt u dat deze technologie uw werkdruk verlaagd?
23. Gaat u deze technologie aanraden wanneer het eenmaal op de markt is verschenen?
24. Heeft u nog overige opmerkingen of ideeën?
This survey is published at the website https://www.enquetesmaken.com/s/a835079 ; here we could publish a questionnaire of 20+ questions and have insight in the answers. As of today (22/03) there is 1 response of a caretaker, but this is a work in progress... We have shared a message on facebook regarding our research and how helpful any responses would be.
Logbook
The logbook uses the following abbreviations for the names of the groupmembers:
- JB: Jeffrey Baijens
- ME: Margot Emke
- JE: Jari van Ewijk
- MK: Marjolijn Kleijer
- BL: Bram Lustenhouwer
- WW: Wouter Wolthuis
Note: The logbook is currently incomplete. Individual tasks from the first weeks still have to be added in.
| Member(s) | Description of the activity | Date | Time |
|---|---|---|---|
| JB, ME, JE, MK, BL, WW | Introduction of the project. Formation of the group. Brainstorming about possible ideas. Determining the initial goal to work on a smart home with focus on easy use (for the elderly) and privacy. | 06-02-2017 | 8:45 - 12:30 |
| ??? | ??? | ??? | ??? - ??? |
| ME, JE, MK, BL, WW | Further brainstorming about the idea. Discussing gathered background information. | 09-02-2017 | 13:45 - 15:30 |
| ??? | ??? | ??? | ??? - ??? |
| BL | Literature research about the advantages and disadvantages of smart home technologies | 11-02-2017 | 14:00 - 17:00 |
| ME | Literature search about elderly preferences regarding smart home technologies | 13-02-2017 | 17:00 - 20:00 |
| JB, ME, JE, MK, BL, WW | Presentation | 16-02-2017 | 13:45 - 17:30 |
| ??? | ??? | ??? | ??? - ??? |
| JB, ME, JE, MK, BL, WW | Presentation | 23-02-2017 | 13:45 - 17:30 |
| ??? | ??? | ??? | ??? - ??? |
| BL | Literature research about what elderly want in technology | 28-02-2017 | 13:00 - 15:00 |
| BL | Making the survey based on literature research | 8-03-2017 | 11:00 - 14:00 |
| JE | Preparing the Raspberry Pi, installing software | 11-03-2017 | 13:00 - 17:00 |
| BL | Adjusting survey to new subject | 11-03-2017 | 15:00 - 18:00 |
| MK | Determining user needs, literature search about heart problems and putting this with the goal on wiki | 12-03-2017 | 16:00 - 19:00 |
| MK | Literature search about heart problems | 13-03-2017 | 11:00 - 13:00 |
| ME | contacting elderly homes for possible interviews | 13-03-2017 | 16:00 - 17:00 |
| ME | Literature search about user needs regarding heart monitoring technologies for questionnaire | 14-03-2017 | 10:00 - 13:00 |
| JE | Giving feedback on survey questions | 14-03-2017 | 17:00 - 18:00 |
| BL | updating survey after feedback | 14-03-2017 | 19:00 - 20:30 |
| JE | Small updates to the wiki | 15-03-2017 | 19:30 - 19:45 |
| JE | Preparing the Raspberry Pi to act as the "control unit" of the prototype, working on some software that check for inputs, can process these inputs and take appropriate actions | 18-03-2017 | 13:00 - 16:00 |
| JB | Worked on 'state-of-the-art: wearable devices' | 18-03-2017 | 14:00 - 17:00 |
| ME, BL | Visit elderly home in order to get thumbs up to interview some of the elderly | 19-03-2017 | 13:00 - 14:30 |
| ME | Transforming the survey from a surveymonkey questionnaire to a questionnaire that can be published | 19-03-2017 | 16:00 - 17:00 |
| ME | Again, visit elderly home, now with a proper meeting | 20-03-2017 | 13:30 - 14:30 |
| MK | Changing focus of the wiki from smart home to smart heart | 21-03-2017 | 11:30 - 12:30 |
| BL | research of advantages and disadvantages of a heart sensor | 22-03-2017 | 09:00 - 12:00 |
| JB | Written and uploaded 'state-of-the-art: types of heart measurements' | 22-03-2017 | 11:00 - 14:00 |
| JE | Wrote a small part about the development of the prototype | 22-03-2017 | 14:00 - 15:00 |
| BL | Fill in question form of elderly home, in order to gain allowance to do the survey | 22-03-2017 | 19:00-20:00 |